Abstract
INTRODUCTION
It is vital to diagnose and treat pulmonary tuberculosis (PTB) early, in the interests of the patient and public health. At the Singapore Tuberculosis Control Unit (TBCU), it was not uncommon to discover abnormal chest radiographs (CXRs) predating their PTB diagnosis by months to years in the electronic medical records (EMRs) of sputum acid-fast bacilli smear-positive patients. Our study explored this observation.
METHODS
The EMRs of sputum smear-positive PTB patients treated at the TBCU from January to July 2014 were viewed for abnormal CXRs preceding their PTB diagnosis. Information in the EMRs pertaining to the indication for the CXRs, radiological reports (including whether the possibility of PTB was stated) and action taken was captured.
RESULTS
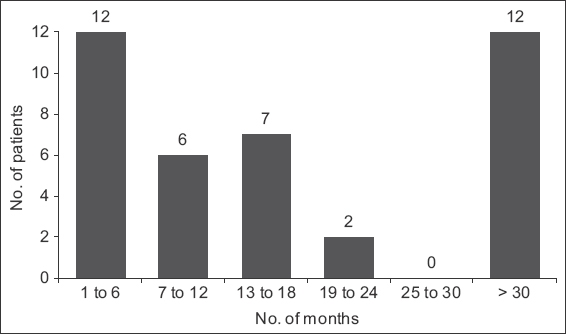
Of the 254 sputum smear-positive patients, 108 had previous CXRs in their EMRs, of whom 39 (36.1%) had previous CXRs compatible with PTB. Most of these were performed in tertiary institutions and for reasons unrelated to PTB. No action was taken in response to these CXRs in 24 (61.5%) patients. 27 (69.2%) patients had abnormal CXRs dating back more than six months, with 12 (30.8%) dating back more than 30 months before the PTB diagnosis. Patients aged ≥ 55 years were significantly more likely to have previous CXRs that were compatible with PTB.
CONCLUSION
PTB patients may be asymptomatic or have chronic indolent disease and remain undiagnosed for years. There is a need for vigilance within our healthcare system to seize opportunities for early diagnosis and treatment to prevent the spread of this infectious disease in Singapore.
INTRODUCTION
The World Health Organization (WHO) declared tuberculosis (TB) a global health emergency in 1993. 25 years later, the WHO estimates that there were 1.6 million deaths and ten million new TB cases in 2017, with eight countries (India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa) accounting for 66% of these cases.(1)
Singapore’s TB rate has stagnated at about 40 per 100,000 population since 2008.(2) The preceding decade had seen the country’s TB rate decline from 58 per 100,000 population in 1998 to 35 per 100,000 population in 2007 due to the initiatives of the Singapore TB Elimination Programme (STEP) launched in 1997.(3,4) We believe that the decade-long stagnation of our TB rate is due to changes in population demographics (i.e. the rapidly ageing population, influx of immigrants and migrant workers from high-TB-burden countries) over the last 15 years and ongoing transmission of TB in a densely populated, urbanised setting. To mitigate transmission, it is vital to detect and treat every TB case as early as possible. At the TB Control Unit (TBCU), the national referral centre where 70% of the country’s TB cases are treated, we observed that a worrying number of sputum acid-fast bacilli (AFB) smear-positive pulmonary TB (PTB) patients had previous abnormal chest radiography (CXRs) in their electronic medical records (EMRs) that had not triggered investigations such as sputum AFB smear or TB molecular testing and mycobacterial cultures, which would have led to diagnosis and treatment of this infectious disease. We conducted the present study to investigate this observation.
METHODS
Ethics approval was obtained from the NHG Domain Specific Review Board (reference no. 2015/00058) for this retrospective study. All newly diagnosed, sputum AFB smear-positive PTB patients seen in the TBCU from January to July 2014 were identified from the STEP Notification Registry. We reviewed the medical records of the 254 notified cases using the patients’ paper case files and EMRs. Any CXRs preceding the last abnormal CXR and their findings were noted. Information regarding the centre where these CXRs were done, the indication for the CXR, whether the possibility of TB was stated in the radiological report, and actions (if any) taken for the abnormal CXR was collected. Abnormal CXRs in the EMR preceding the PTB diagnosis were compared with the CXR used by the TBCU consultant to make the PTB diagnosis to determine PTB compatibility and disease progression. The time interval from the first abnormal CXR to PTB diagnosis (taken as date of TB notification) was ascertained.
Data analysis was done using SPSS Statistics version 17.0 (SPSS Inc, Chicago, IL, USA). Cases without a previous CXR prior to PTB diagnosis were excluded from the analysis. Descriptive analysis was done for cases with previous abnormal CXRs compatible with PTB. Pearson’s chi-square test was used to compare the background characteristics of those with a previous normal CXR and those with a CXR that was compatible with PTB. A p-value < 0.05 was considered to be statistically significant.
RESULTS
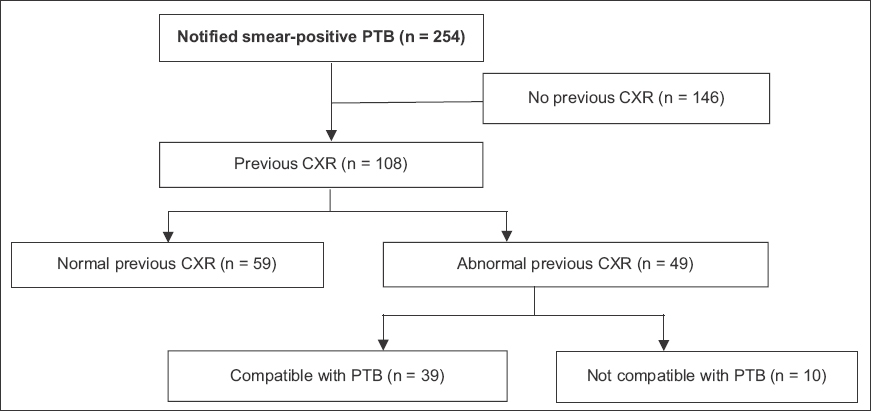
Of the 254 sputum AFB smear-positive PTB cases treated at the TBCU during the study period, 108 (42.5%) patients had previous CXRs in their EMR: 49 (45.4%) had abnormal CXRs, of whom 39 (36.1%) out of 108 patients had CXRs compatible with PTB (
Fig. 1
Flowchart shows the process of data collection. CXR: chest radiograph; PTB: pulmonary tuberculosis
The time intervals between the first previously abnormal CXR and the TB diagnosis (taken as date of TB notification) were noted (
Fig. 2
Chart shows the time interval between the first previously abnormal radiograph and the diagnosis of tuberculosis (taken as the date of notification).
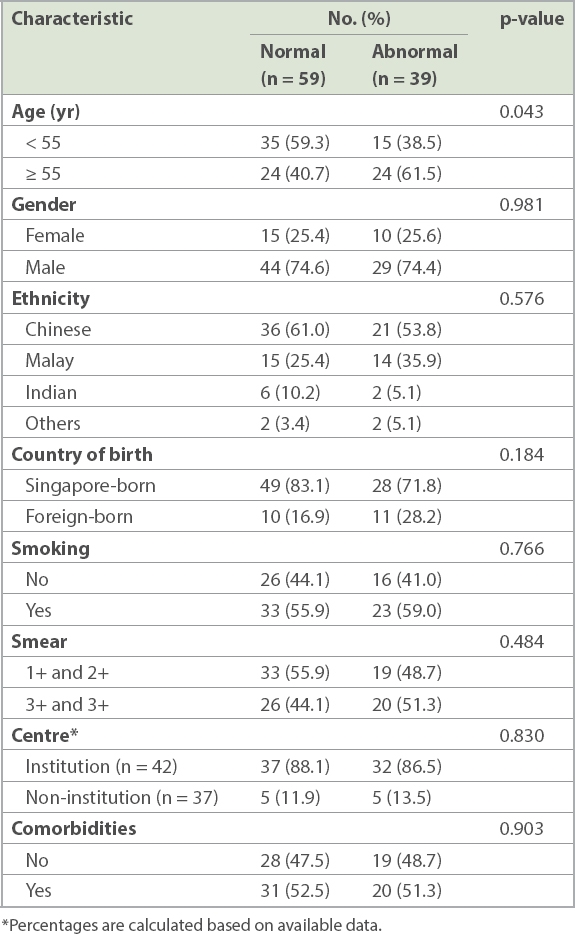
Patients who were aged 55 years and above were significantly more likely to have previous CXRs compatible with PTB (
Table I
Comparison of background characteristics between patients with previous normal CXR and those with previous CXR compatible with PTB.
The majority (n = 32, 82.1%) of the 39 patients with previous abnormal CXRs had them performed in tertiary institutions: emergency departments (n = 16); cardiology departments (n = 4); general medicine departments (n = 2); and at respiratory medicine (n = 1), obstetrics and gynaecology (n = 1), infectious disease (n = 1), general surgery (n = 2) and neurology departments (n = 1). Information pertaining to institution and department was not available for four patients.
Among the 30 patients in whom the indication for CXR could be ascertained, the majority (n = 17) had CXRs performed for reasons unrelated to PTB. These reasons were falls (n = 4), road traffic accidents (n = 2), physical assault (n = 1), preoperative screening (n = 2), cerebrovascular accident (n = 1), biliary colic (n = 1), leg swelling due to proteinuria (n = 1), asteatotic eczema (n = 1), leg cellulitis (n = 1), aortic dissection (n = 1), cholelithiasis (n = 1) and abnormal chest findings of basal crepitations on a background of ovarian carcinoma (n = 1). The remaining 13 patients had CXRs for evaluation of symptoms possibly attributable to PTB (i.e. cough, fever, chest pain). In these patients, the mean and median durations between the first abnormal CXR and the PTB diagnosis were 14 months and nine months, respectively, whereas they were 23 months and 14 months, respectively, among the 17 patients with CXRs performed for reasons unrelated to PTB.
The eventual diagnosis of smear-positive PTB was made in 27 patients when they were admitted with PTB symptoms, diagnosed with PTB and referred to the TBCU for management upon discharge, and in 12 patients when they were referred as outpatients for PTB symptoms to the TBCU (five from polyclinics, three from emergency departments, three from specialist respiratory clinics and one from a general practitioner).
In the CXR reports of the 39 patients with abnormal CXRs, descriptions compatible with PTB (i.e. ‘scarring’, ‘granuloma’, ‘cavity’, ‘fibrosis’) were used in 14 reports, while ‘opacities’ and ‘consolidation’ were used in 29 reports. ‘Tuberculosis’ was mentioned in four CXR reports. More than one description could be used in each report (
Fig. 3
Chart shows the descriptions used by radiologists in the reports of the 39 patients with abnormal radiographs. Each report could have more than one description.
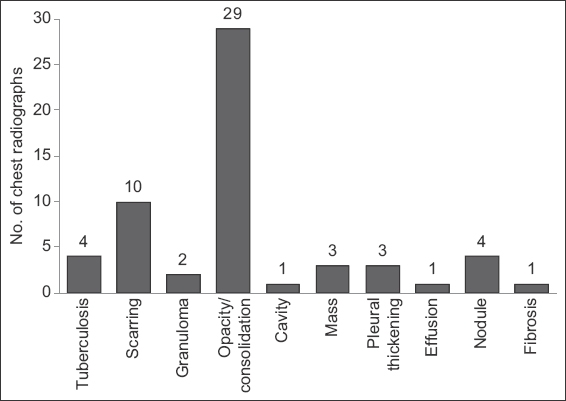
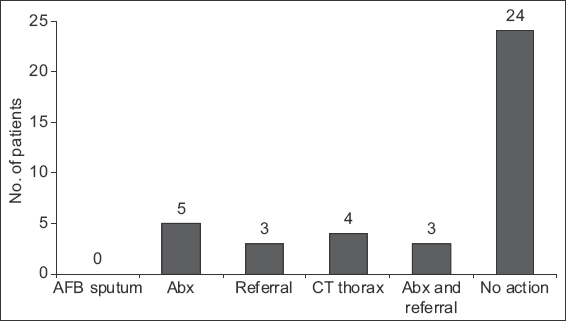
Fig. 4
Chart shows the actions taken in response to the previous abnormal radiographs. Abx: antibiotics; AFB: acid-fast bacilli; CT: computed tomography
DISCUSSION
We found that 36.1% (n = 39) of sputum AFB smear-positive PTB patients with previous CXRs available in their EMRs had prior radiological evidence of active PTB. Most of these CXRs were performed in tertiary institutions for reasons unrelated to TB. No action was taken in response to the abnormal CXRs in 24 (61.5%) patients. The majority of the abnormal CXRs dated back more than six months before the diagnosis of smear-positive PTB. Previous CXRs compatible with PTB were more likely to be found in patients aged 55 years and above.
Active TB mostly affects the lungs and has a wide spectrum of manifestation, ranging from subclinical to fulminant, fatal disease.(5) It may run a chronic indolent course, and patients with culture-positive PTB have even been known to be asymptomatic. This is demonstrated in our patients who had evidence of PTB on CXRs that were performed for unrelated reasons dating back months to years before they were diagnosed with smear-positive PTB. CXR has high sensitivity (87%–98%) but low specificity (46%–89%) for PTB, depending on the interpretative skills of the radiologist.(6) Typical CXR manifestations of PTB are cavitation in the apical/apicoposterior segments of the upper lobes or the superior segment of the lower lobes. However, the radiological manifestations are mainly non-specific, mimicking other conditions such as malignancy and pneumonia. In settings with intermediate and high TB incidence, there should be a high index of suspicion for PTB in persons with abnormal CXR. Clinicians should be aware that radiology reports of scarring, fibrosis and granuloma, which may imply old, healed (i.e. inactive) TB, do not necessarily exclude active PTB, and that microbiological testing of sputum must be carried out. Clinicians should also be cognisant of the entity of culture-negative PTB(7) and appreciate that treatment of patients with early disease has individual and public health benefits in preventing late disease manifestations and minimising transmission in the community.
Early detection and treatment of TB is of the highest priority in TB control. Delay in treatment not only leads to poorer patient outcomes, but also prolongs the exposure period of the infectious case in the community and is associated with greater transmission to contacts.(8) Delayed TB diagnosis may be due to the patient or healthcare system. A systematic review by Storla et al of 58 studies addressing diagnostic delay found heterogeneous risk factors associated with the delay, which included: HIV; coexistence of chronic cough and/or other lung diseases; negative sputum smear; extrapulmonary TB; rural residence; low access (geographical or sociopsychological barriers); initial visitation of a government low-level healthcare facility, private practitioner, or traditional healer; old age; poverty; female gender; alcoholism and substance abuse; history of immigration; low educational level; low awareness of TB; incomprehensive beliefs; self-treatment; and stigma. The symptoms reported in 25 studies were cough (85%), fever (65%), weight loss (62%), chest symptoms (50%) and haemoptysis (25%). Less frequently reported symptoms were sputum, fatigue and increased sweating.(9) Although cough is the most common presentation of the disease, the pathophysiology of TB is such that patients may have low-grade, intermittent symptoms (which they may not bring to medical attention) yet are capable of transmitting the infection to their close contacts in the community.
One limitation of our study is that CXRs done in the private sector or sectors not linked to the EMR system were not captured. Thus, our findings do not fully reflect, and likely underestimate, the extent of missed opportunities for earlier diagnosis in patients who had previously abnormal CXRs prior to PTB diagnosis. Furthermore, we were unable to ascertain the circumstances behind ‘no action taken’ in response to the abnormal CXRs and can only speculate that one of the following occurred: (a) the abnormal CXR report was missed by the requesting physician; (b) the report was noted but not acted upon; or (c) the intention to act was not translated into concrete action. As most of the CXRs were performed for indications unrelated to TB, it is possible that attention may not have been paid to the abnormal CXR results in many of these cases. This is a worrying finding that has implications not only for missed early diagnosis of PTB, but also that of lung carcinoma.
Our study shows that within our public healthcare institutions, failure to recognise or take appropriate action in response to abnormal CXRs has resulted in diagnostic delay of PTB for as long as several years. There is a need to increase vigilance and improve our healthcare system such that CXR findings are noted and acted upon in a timely and appropriate manner. In Singapore, a country with intermediate TB incidence, active PTB should be considered as a differential diagnosis in persons with abnormal CXR and sputum specimens sent for microbiological testing even in the absence of classical symptoms.


