Abstract
INTRODUCTION
Our study aimed to review the quit rates of smokers from our inpatient smoking cessation programme in relation to habits and sociodemographic factors, and also to explore the potential usefulness of electronic cigarettes (ECs) by reviewing smoking motivations.
METHODS
This was a retrospective study of patients recruited into our inpatient smoking cessation programme from June 2008 to June 2015. Sociodemographic factors and information on smoking habits were collected using a counsellor-administered questionnaire. Patients were given intensive counselling followed by a phone interview at one, three and six months to assess smoking status.
RESULTS
A total of 2,722 patients were enrolled. 27.6% of patients were abstinent at six months’ follow-up. Patients who quit smoking were older, married, initiated smoking at a later age and had lower Fagerström Test for Nicotine Dependence scores. There was a trend towards successful quitting in those with higher education levels and Chinese ethnicity, but this was not statistically significant. Patients who planned to quit cold turkey and those who quit because of social pressures were more successful. Of the smoking motivations, only nicotine dependence was an independent predictor of smoking cessation.
CONCLUSION
Smoking motivations such as habitual use and psychological dependence did not influence quit rates and therefore do not support the use of ECs. Instead, a cold turkey method of quitting was shown in our study to contribute to cessation success. We recommend an increased focus on the use of pharmacologic aids as well as involvement of peer/spousal support to aid in such quit attempts.
INTRODUCTION
Smoking is a significant risk factor for chronic disease, including coronary artery disease, lung disease and cerebrovascular disease. Tobacco smoking is the most preventable cause of death, and accounts for one in 10 deaths around the world.(1) Despite numerous efforts with regard to smoke-free laws or advertising bans, the smoking prevalence in Singapore continues to rise, with an upward trend from 12.6% in 2004 to 14.3% in 2010 based on data from our National Health Surveys.(2,3) Other than the prevention of smoking initiation, engagement of active smokers with a view towards cessation plays an important role in managing this public health epidemic, with significant reductions in mortality risk achieved even within five years of smoking cessation.(4) Although smoking cessation programmes can be instituted in various healthcare settings, including community pharmacy chains and various non-government organisations, admission to hospital provides an opportunity to help patients stop the use of tobacco. Inpatient smokers may be more open to receiving help and advice at a time of perceived vulnerability, and may find it easier to quit in an environment where smoking and the use of tobacco is prohibited. In a 2008 systematic review, smoking counselling that began during hospitalisation and included supportive contacts after discharge from hospital increased smoking cessation rates.(5) Our local 2013 clinical practice guidelines also recommend behavioural support by a trained advisor for tobacco use and dependence for all hospitalised patients who are tobacco users.(6) There is, however, little data reflecting the efficacy of inpatient smoking cessation programmes in Singapore. The last study in 2004 by Zow et al evaluating 425 patients in their inpatient smoking cessation programme showed a six-month quit rate of 30%.(7)
In recent years, electronic cigarettes (ECs) have also gained popularity worldwide as an aid to smoking cessation despite conflicting evidence for their safety and efficacy.(8) Although a recent United Kingdom (UK) study suggests an association between declining smoking prevalence and the use of ECs,(9) concerns about ECs having carcinogenic potential,(10) inconsistencies between product labelling and actual ingredients,(11) and ECs serving as ‘gateways’ to traditional smoking remain.(12) With such potential dangers, ECs are currently prohibited in Singapore.(13) However, proponents of ECs suggest that they can more effectively satisfy a smoker’s craving compared with licensed nicotine replacement therapies (e.g. nicotine gum) by also satisfying the psychological aspects and habitual rituals of smoking. We postulate that demonstrating differences in habitual or psychological dependence between successful quitters and non-quitters will provide a perspective on the usefulness of ECs.
The aims of our study are therefore twofold: (a) to describe the predictors of smoking cessation success in our inpatient smoking cessation programme and (b) to evaluate the impact of smoking motivations on smoking cessation and whether our findings support the utility of ECs.
METHODS
This was a single-centre retrospective study of all patients enrolled in our institution’s inpatient smoking cessation programme from June 2008 to June 2015. All patients admitted into participating wards were screened for smoking status and those agreeable were enrolled in the programme. There were no exclusion criteria. Ethics approval for this project was obtained from the SingHealth Centralised Institutional Review Board.
The inpatient smoking cessation programme was first started in September 2006 as a partnership between SingHealth and the Health Promotion Board (HPB) of Singapore, with the aim of integrating tobacco cessation intervention into the existing clinical management of patients. Funding for manpower, training and resources was provided by HPB with hospitals reporting back on reach and quit rates on a quarterly basis.
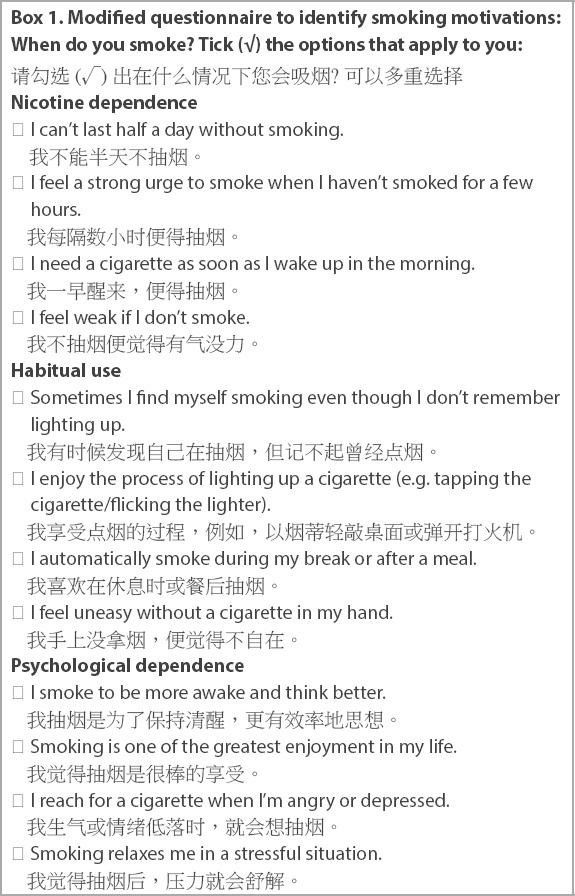
For patients who agreed to be enrolled in the inpatient smoking cessation programme, intensive counselling was provided by certified quit-smoking consultants with each session lasting approximately 45 minutes. All quit-smoking consultants went through courses organised by HPB to attain at least Level 2 certification.(14) During these sessions, sociodemographic data and smoking patterns were collected using a standardised questionnaire. Fagerström Test of Nicotine Dependence (FTND)(15) scores were also collected. A simplified 12-part questionnaire with a Mandarin translation (
Box 1
Modified questionnaire to identify smoking motivations: When do you smoke? Tick (√) the options that apply to you:
Statistical analysis was performed using IBM SPSS Statistics 19.0 (IBM Corp, Armonk, NY, USA). Data was expressed as mean ± standard deviation for continuous variables, and percentages or numbers for categorical variables. Categorical and dichotomous variables were compared using chi-square test, and continuous variables with t-test. Logistic regression modelling (enter method) was used to identify independent predictors for quitting and to estimate the odds ratio (OR) and 95% confidence interval. FTND scores were not included in multivariate analysis due to interactions with smoker types. All comparisons were two-sided and significant differences were defined as p-value < 0.05.
RESULTS
A total of 2,722 patients were enrolled in the inpatient smoking cessation programme. Their mean age was 52.9 years, and the majority (94.4%) of the subjects were male. There were 1,365 (50.1%) Chinese, 1,045 (38.4%) Malay and 211 (7.8%) Indian patients, and 101 (3.7%) were from other ethnicities. 30.1% of the patients were lost to follow-up (and therefore considered non-quitters), while 27.6% were abstinent at six months.
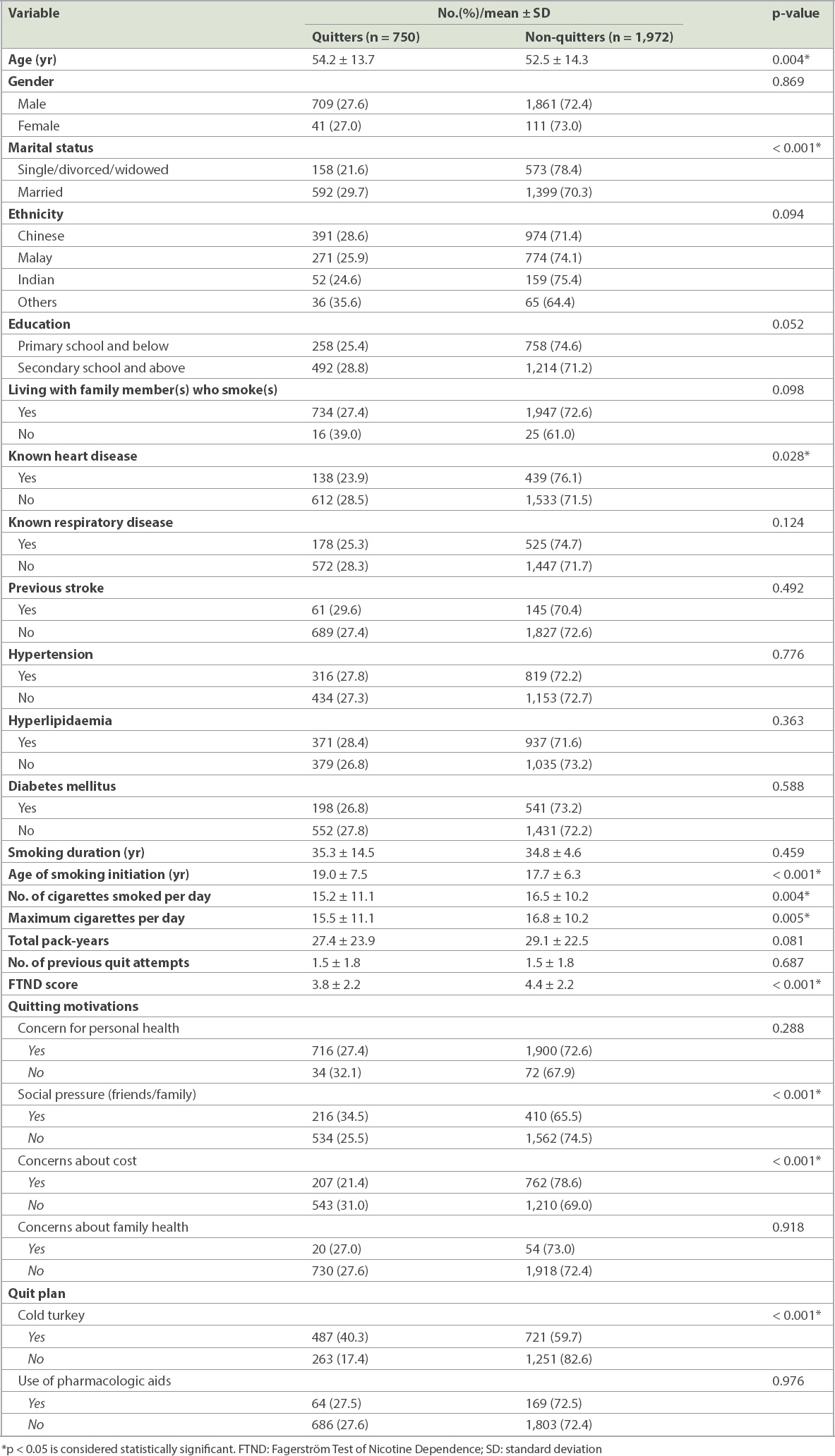
Patients who quit smoking were more likely to be older (54.2 ± 13.7 years vs. 52.5 ± 14.3 years, p = 0.004), married (p < 0.001), had started smoking at a later age (19.0 ± 7.5 vs. 17.7 ± 6.3, p < 0.001), smoked fewer cigarettes a day (15.2 ± 11.1 vs. 16.5 ± 10.2, p = 0.004) and had lower FTND scores (3.8 ± 2.2 vs. 4.4 ± 2.2, p < 0.001) compared to those who did not quit. Patients with prior heart disease were less likely to quit (p = 0.028). Patients who intended to quit smoking via cold turkey rather than by slow reduction (p < 0.001), as well as those who cited social pressures from family or friends (p < 0.001), were also more successful. Those who had cost concerns were less successful in quitting (p < 0.001). There was a non-significant trend for patients with higher educational status (p = 0.052) and those of Chinese ethnicity (p = 0.094) to successfully quit smoking. There was no significant difference found between quitters and non-quitters when evaluating the use of pharmacologic aids (p = 0.976) (
Table I
Demographic predictors of smoking cessation at six months.
Univariate analysis of smoking motivations showed that nicotine dependence (p < 0.001) and habitual use (p = 0.009) were significant predictors of cessation success (
Table II
Univariate analysis of smoking motivations and smoking cessation.
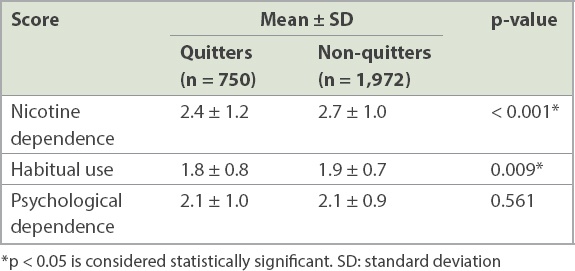
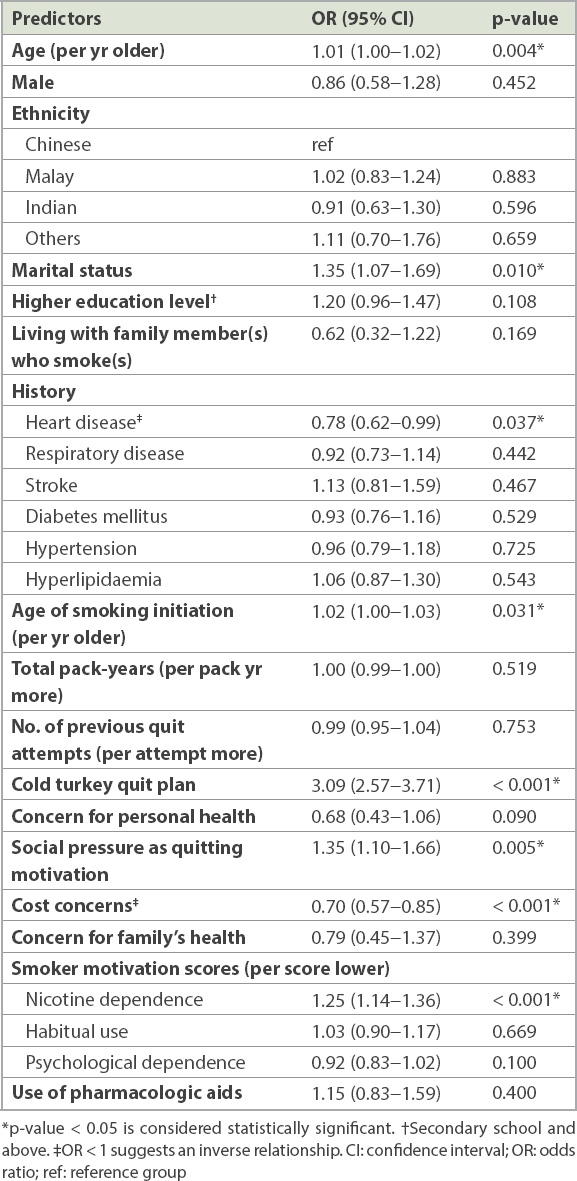
Table III
Logistic regression analysis of predictors of successful smoking cessation at the six-month follow-up.
Analysis of patients’ ethnicity showed no significant differences in terms of marital status or family history of smoking. There was, however, a significant difference in education levels, with 54.6% of Chinese patients, 67.1% of Malay patients, 80.6% of Indian patients and 89.1% of patients of other ethnicities (p < 0.001) having secondary level education and above. When patients with and without heart disease were compared, there were no significant differences in FTND scores, but patients with heart disease tended to be older (57.5 ± 11.8 years vs. 51.7 ± 14.4 years, p < 0.001).
Among the patients (n = 969) who cited cost concerns, 207 (21.4%) were successful quitters, whereas 366 (37.8%) reduced cigarette consumption but continued to smoke. In contrast, the patients who did not cite cost concerns had a higher quit rate of 31.0%, with a lower proportion of subjects (n = 594, 33.9%) having reduced cigarette consumption.
DISCUSSION
Our inpatient smoking cessation programme had a quit rate of 27.6%, consistent with results by Tønnesen, in which an abstinence rate of 25% is expected from a smoking cessation programme.(17) The known common predictors of smoking cessation such as age, age of smoking initiation, marital status and FTND scores were similarly identified in our study.(18)
We found that the presence of heart disease was inversely related to successful quitting. Patients with known heart disease were also older compared to those without heart disease, another factor that should have improved cessation rates. We postulate that many patients who had heart disease were greatly motivated during the time of diagnosis and had therefore already quit smoking, while those who were enrolled in our study were the patients who had more difficulty quitting. It would be interesting to evaluate the impact of admission diagnoses on cessation rates in future research.
In the evaluation of pharmacologic aids, no difference was found between quitters and non-quitters. However, the proportion of patients who utilised pharmacologic aids in our study was also very low at 8.6%, possibly due to cost or physician barriers, and therefore the sample size might have been insufficient to detect differences.
In our review of patients’ smoking motivations, it was enlightening to note that only nicotine dependence, but not habitual use or psychological dependence, was an independent predictor for successful smoking cessation. This suggests that the use of ECs as a means of nicotine replacement and delivery is unlikely to provide additional benefits compared with other forms of nicotine replacement therapies. However, there is evidence that ECs do lead to higher quit rates,(19) and this might be due to their higher speed of nicotine delivery, which is important for smokers’ satisfaction.(20) With the uncertainties surrounding EC use and its current banned status in Singapore, efforts should be focused on promoting and/or subsidising other proven pharmacologic aids that have low rates of use in our institution. In particular, more attention could be placed on nicotine replacements that have more rapid effects, such as nicotine inhalers or sprays. These are likely to provide higher odds for successful quitting than other forms of nicotine replacements when compared to a placebo (OR 2.17‒2.37 for nicotine inhalers/sprays vs. OR 1.71‒2.07 for nicotine gum/patch).(21)
Interestingly, we found that cost concerns had an inverse relation with quit rates. Tobacco taxation has been a cornerstone of policymaking that targets tobacco usage(22) and is one of the MPOWER measures for tobacco control introduced by the World Health Organization.(23) An International Agency for Research on Cancer review of more than 100 econometric studies confirmed that tobacco taxes and consumption have a strong inverse relation.(24) Nevertheless, although most studies found that raising cigarette prices through taxation is an effective measure for reducing smoking among youth, young adults and persons of low socioeconomic status, there is a lack of evidence to support the impact of increases in cigarette prices on smoking behaviour in heavy/long-term smokers.(25) Although our study showed that cost concerns lead to a higher proportion of smoking reduction, there was a significant lower rate of complete cessation. This is of concern, as smoking reduction might not bring about the same benefits as complete cessation. In a large 16-year follow-up study of 19,732 patients by Godtfredsen et al, smoking reduction was not associated with a decrease in mortality from tobacco-related diseases, whereas smoking cessation reduced mortality risk.(26) This was further supported by an opinion paper by Begh et al, who summarised that the evidence of harm reduction from reduced smoking is suggestive but not conclusive due to the lack of detailed characterisation of the extent and length of smoking reduction in relation to health outcomes.(27) Therefore, although excise taxes play an important role in preventing smoking initiation and promoting smoking reduction, the end goal of promoting cessation through reduction should remain, rather than promoting reduction alone. Policymakers need to be aware that tax controls could have minimal impact on the health and well-being of established long-term smokers, especially if they do not lead to complete cessation.
Our study also showed that patients who preferred to quit cold turkey were more successful than those who chose to quit gradually. Although a Cochrane review in 2012 found reduction to be comparable to abrupt cessation,(28) a more recent randomised controlled trial involving 697 smokers from the UK not only showed the superiority of a cold turkey approach, but also that those who preferred to quit gradually were significantly less likely to be abstinent than participants who preferred to quit abruptly, regardless of their trial allocation.(29) We postulate that in patients admitted to a smoke-free hospital environment, planned gradual reduction deters complete abstinence by allowing re-introduction to nicotine with its addictive properties.
To the best of our knowledge, this is the first smoking cessation study that evaluated the impact of ethnicity on smoking cessation in a Southeast Asian population. There was a trend for Chinese patients to have higher quit rates compared to Malay and Indian patients, although this was not statistically significant. Differences in education levels were unable to account for these findings, as the Chinese patients in our study population had lower education levels compared to the Malay or Indian patients, which should have led to lower rather than higher cessation rates. Socioeconomic status is also a known predictor of smoking cessation success(30,31) and could explain these differences, but this was not assessed in our study population. We therefore postulate that household size could account for the higher rates of smoking cessation among the Chinese. In the 2015 Singapore General Household Survey, the average household size of Chinese households was 3.3, compared to 3.9 for Malay households and 3.6 for Indian households.(32) As smokers tend to stay with other smokers, larger household sizes with more smokers living together could result in subjects finding it more difficult to quit when they encounter family members who smoke too, thereby reinforcing mutual behaviour. In our study population, an overwhelming majority (98.5%) of the patients reported living with a family member who smoked. The very small proportion of patients who did not do so was too small a sample to result in statistically meaningful results, although 39.0% of them quit successfully compared to 27.4% of patients who lived with family members who smoked (p = 0.098).
The impact of education level on quit rates also trended towards significance in our study, similar to prior studies. It is likely because education affects an individual’s level of understanding and therefore increases the benefits of counselling sessions.(33,34) Having adequate health knowledge and understanding the health benefits of smoking cessation is an important aspect of cessation counselling. In individuals with lower education levels, longer counselling sessions carried out in a language that the subject is comfortable with, placing additional focus on the patient’s friends or family, and booster counselling sessions as an outpatient could help to improve quit rates.
There were a few limitations to our study. Firstly, a relatively high proportion of patients (31.0%) were lost to follow-up. However, attrition rates in smoking cessation studies are known to be high with rates ranging from 10% to 50%.(35) In our study, these patients were considered non-quitters, an assumption that is generally made in smoking cessation trials.(36) Indeed, in a 2016 Swedish study of quitline evaluation, non-responders were more likely to be continued smokers.(37) Secondly, our study did not carry out biochemical validation to verify abstinence. Nevertheless, self-reporting is considered accurate in most smoking cessation studies,(38) and there was no reason to assume that untrue answers were differently distributed between those who quit and those who did not. This is further supported by a 2015 Cochrane review of psychosocial interventions for smoking cessation in patients with coronary heart disease, which found that studies with validated assessments of smoking status at follow-up had similar efficacy to non-validated trials.(39)
Thirdly, a potential confounder was not evaluated in this study: the degree of intrinsic motivation or readiness to quit smoking. We can assume that all patients who agreed to enrol in our smoking cessation programme were ready to quit smoking, although those who chose to attempt quitting with the cold turkey method could have been more motivated and determined to quit. The number of prior quit attempts by each patient had were also recorded, and this actual quitting behaviour, which was equal in both arms, can be considered as an indication of the desire to quit.(40) Nevertheless, it is uncertain how well a patient’s motivation predicts smoking abstinence; a recent study in 2015 by Ussher et al showed no correlation.(41)
Lastly, our study only had a follow-up period of six months. A longer follow-up of 12 months would have been preferred, as abstinence at 12 months would be a good predictor for long-term abstinence.(42) Conversely, a shorter follow-up period might have resulted in underestimation of quit rates for subjects who planned gradual reduction and chose a quit date beyond six months from the time of counselling. Regardless, abstinence for more than three months can be considered an intermediate criterion for cessation success,(43) and abstinence for a duration of six months is currently recommended as an outcome evaluation indicator in our local guidelines.(6)
In conclusion, tobacco cessation is difficult given the addictive nature of nicotine, as evidenced by the less than ideal quit rates in the present study and other smoking intervention studies. To encourage better quit rates, we propose a cold turkey quit plan for smokers identified during admission to hospital. This should be in conjunction with efforts to support the individual’s quit attempt and to manage withdrawal symptoms by promoting or subsidising pharmacologic aids. The patient’s family or friends should also be actively involved in the process (e.g. sitting in during counselling sessions), and further studies can be conducted to evaluate the benefits of this. Finally, our study did not find that habitual use or psychological dependence affected abstinence rates and therefore cannot support the utility of ECs. Rather, we recommend further studies on other approved rapid-release nicotine preparations.
ACKNOWLEDGEMENTS
The authors would like to acknowledge HPB for its continued support of our inpatient smoking cessation programme. We would also like to thank Ms Carmen Kam Jia Wen, Research Officer, Clinical Trials and Research Unit, Changi General Hospital, for providing statistical consultation.


