Abstract
Appendiceal neoplasms are rare and often only discovered incidentally during surgery performed for acute appendicitis. Computed tomography (CT) has been demonstrated to be a reliable technique for accurately establishing the preoperative diagnosis of appendiceal neoplasms that manifest as acute appendicitis through the presence of certain imaging findings. Other manifestations of appendiceal neoplasms include appendiceal mass, mucocoele, localised abscess formation, ileus, increasing abdominal girth from pseudomyxoma peritonei, and intussusception. This pictorial essay illustrates varied CT findings of neoplasms of the appendix, with emphasis on the more commonly encountered manifestations of these tumours.
INTRODUCTION
Appendiceal neoplasms are uncommon tumours that are mostly found incidentally during appendicectomies performed for appendicitis, accounting for 0.5%–1.0% of appendicectomy specimens.(1) Given the frequent manifestation of appendiceal neoplasms as acute appendicitis, radiological imaging, particularly computed tomography (CT), is often performed for these patients and can lead to diagnosis. Other less common presentations may also be diagnosed on imaging, including appendiceal mass, mucocoele, intussusception, bowel obstruction, secondary genitourinary complications or complications such as perforation with abscess formation or ovarian lesion.(1) It is important to detect appendiceal neoplasms early, as the prognosis is usually poor if they are found at an advanced stage. Early detection is also important because it may change the surgical approach (open vs. laparoscopic surgery) and the surgical procedure (appendicectomy vs. right hemicolectomy).(2) In this pictorial essay, we aimed to highlight the common CT features of appendiceal neoplasms, other less frequent but important manifestations and potential imaging pitfalls.
ACUTE APPENDICITIS
The vermiform appendix is a blind-ended outpouching that typically arises from the posteromedial caecal wall about 2 cm below the ileocaecal valve. On imaging, the normal appendix measures 6 mm or less in maximal outer diameter (
Fig. 1
(a) Gross anatomical graphical illustration of the caecum and appendix with cross sections through the appendix shows key radiological findings in (b) a normal appendix with a diameter < 6 mm; and (c) non-tumoral appendicitis with appendix diameter > 6 mm, mural thickening and periappendiceal fat stranding. (d–h) Illustrations of an appendix with an appendiceal neoplasm show (d) a paucity of periappendiceal fat stranding; (e) outer diameter > 15 mm (white double arrow) or luminal diameter > 13 mm (blue double arrow); (f) intraluminal soft-tissue nodularity; (g) periappendiceal lymphadenopathy; and (h) infiltration of adjacent structures.
Often considered as a non-essential vestigial organ, the appendix is better known for its pathological role in acute appendicitis, one of the most common abdominal surgical emergencies. Acute appendicitis occurs when there is obstruction of the appendiceal lumen, leading to fluid accumulation, luminal distension and inflammation before finally resulting in perforation. CT remains the imaging modality of choice in evaluating adult patients presenting with acute appendicitis because of its high diagnostic accuracy.(4)
On CT, acute appendicitis is diagnosed when there are signs of appendiceal thickening and inflammation. Appendiceal thickening is defined as the appendix having an outer diameter greater than 6 mm. Inflammatory changes include appendiceal wall thickening measuring 3 mm or greater and mural hyperenhancement. Other supportive findings such as periappendiceal fat stranding, extraluminal fluid, phlegmon, appendicolith and lymphadenopathy may be observed.(4)
APPENDICEAL NEOPLASMS
Appendiceal neoplasms are important entities to consider in patients presenting with acute appendicitis. About 30%–50% of appendiceal neoplasms initially manifest as acute appendicitis.(1) Primary appendiceal neoplasms have a diverse histology comprising of epithelial tumours (mucinous and colonic subtypes), neuroendocrine tumours (NETs), goblet cell carcinoids, lymphoma, mesenchymal tumours and sarcomas.(3) NETs are the commonest, followed by epithelial neoplasms. In comparison, the other neoplasms are much rarer.(1,3,5) The histology subtype and extent of disease at the time of diagnosis help to predict survival. For example, the presence of a signet-ring cell formation confers the worst prognosis with an average survival rate of six months, while a low-grade mucinous neoplasm gives a median overall survival of eight years.(5) Prompt diagnosis of appendiceal neoplasms is therefore essential.
CT FEATURES OF COMMON APPENDICEAL NEOPLASMS
Neuroendocrine tumours
NETs are usually less than 1 cm in diameter and are often established incidentally in postoperative appendicectomy specimens. Most are located at the tip of the appendix and are difficult to identify on CT due to their small size. NETs frequently show imaging findings of acute appendicitis and may mimic appendicoliths (
Fig. 2
(a) Contrast-enhanced coronal CT image of a 48-year-old woman with a proven carcinoid tumour of the appendix shows appendiceal mural thickening and hyperenhancement (arrows) with no significant periappendiceal fat stranding. (b) Contrast-enhanced axial CT image of an 80-year-old woman with an appendiceal carcinoid tumour shows a dense nodular lesion mimicking an appendicolith (black arrow) at the tip of the appendix (white arrow).
Non-mucinous (colonic-type) epithelial tumours
Non-mucinous epithelial tumours consist of adenomas, adenocarcinomas and polyps. These may obstruct the appendiceal lumen and often result in acute appendicitis (
Fig. 3
A 69-year-old man presented with right iliac fossa pain. Contrast-enhanced (a) coronal and (b) axial CT images show diffuse mural thickening (white arrows in a & b) and periappendiceal fat stranding (black arrow) without cystic dilatation or discrete soft-tissue mass. The serendipitous diagnosis of invasive moderately differentiated adenocarcinoma of the appendix was only made following appendicectomy and histologic examination.
Fig. 4
A 66-year-old man presented with right iliac fossa pain. Contrast-enhanced (a) coronal and (b) axial CT images show cystic dilatation of the appendiceal tip (white arrow) and diffuse soft-tissue infiltration at the appendiceal base (black arrow) with minimal periappendiceal fat stranding. An enlarged ileocolic lymph node is also present (asterisk). This is suspicious for tumoral acute appendicitis. The diagnosis of a moderately differentiated appendiceal adenocarcinoma was established following surgery and histologic examination.
Mucinous epithelial tumours
The majority of appendiceal epithelial tumours are mucinous. Mucinous neoplasms are generally classified as adenomas, low-grade appendiceal mucinous neoplasms, high-grade appendiceal mucinous neoplasms and mucinous adenocarcinomas (MACAs). MACAs demonstrate infiltrative invasion and are further classified as well, moderately or poorly differentiated.(3)
Most mucinous neoplasms present as mucocoeles and are less likely to manifest as appendicitis than other appendiceal neoplasms. This is because mucocoeles result from chronic luminal obstruction without significant inflammation and generally require superinfection to develop into acute appendicitis. Other manifestations comprise of palpable mass, increasing abdominal girth from pseudomyxoma peritonei (PMP), intussusception, torsion and right ureteral obstruction.(1)
Mucocoeles
Appendiceal mucocoele is defined as dilatation of the appendiceal lumen due to abnormal mucus accumulation.(1,3) CT can be used to diagnose an appendiceal mucocoele with high accuracy.(1) The typical appearance is a round or tubular well-encapsulated cystic mass with little periappendiceal inflammation (
Fig. 5
A 50-year-old man presented with right lower abdominal pain. Contrast-enhanced (a) axial and (b) coronal CT images show a well-encapsulated tubular cystic structure in the right iliac fossa (arrows in a & b) with minimal surrounding fat stranding. There is communication with the caecum (not shown), raising suspicion for an appendiceal mucocoele. Histology confirmed appendiceal mucocoele secondary to low-grade appendiceal mucinous neoplasm.
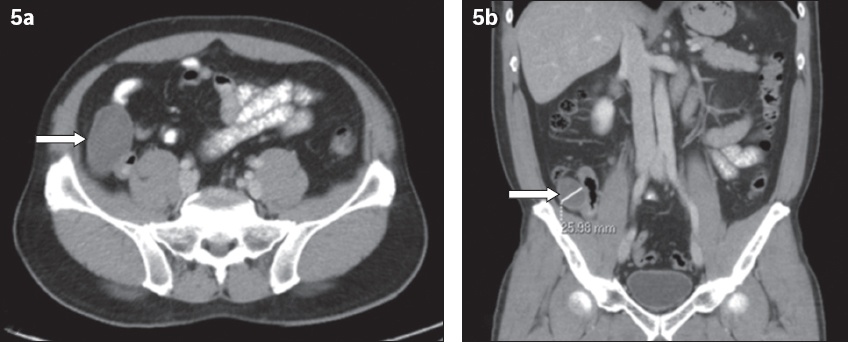
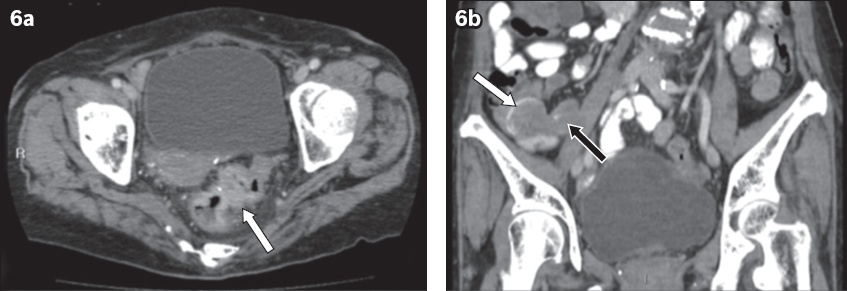
Fig. 6
An 86-year-old woman presented with generalised abdominal pain. (a) Contrast-enhanced axial CT image shows irregular circumferential mural thickening and enhancement in the rectosigmoid (arrow) suggestive of malignancy. (b) Coronal CT image shows tubular dilatation of the appendix with low attenuation contents (black arrow) and curvilinear mural calcification (white arrow). Histology confirmed synchronous rectosigmoid adenocarcinoma and appendiceal mucocoele secondary to low-grade appendiceal mucinous neoplasm.
Mucocoeles can be caused by neoplastic and non-neoplastic conditions. An attempt should be made to differentiate between these two broad groups, as they have differing clinical courses.(7) Generally, neoplastic conditions should be considered when mucocoeles are larger than 2 cm, while non-neoplastic causes rarely result in dilatation larger than 2 cm.(8) Reported CT features suggestive of a malignant mucocoele are wall irregularity, internal soft-tissue attenuation and enhancing nodularity (Figs.
Fig. 7
An 87-year-old woman presented with infiltrative mucinous adenocarcinoma of the appendix. Contrast-enhanced (a) axial and (b) coronal CT images show cystic appendiceal dilatation (black arrow) with nodular mural thickening and enhancement (asterisk). There is a paucity of adjacent inflammatory changes. The appendix was adherent to the adjacent iliacus muscle (white arrow). The tumour was found to be perforated at the time of surgery.
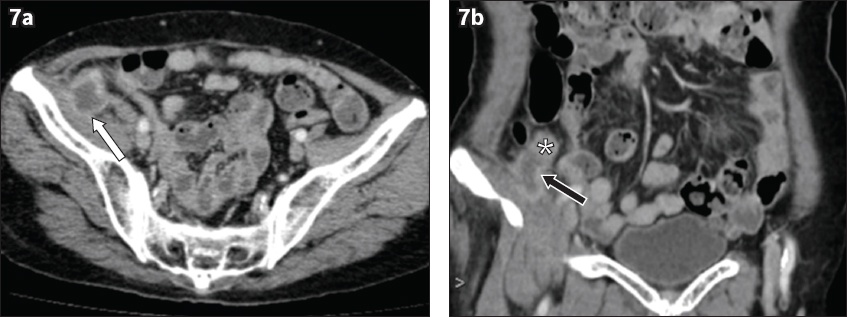
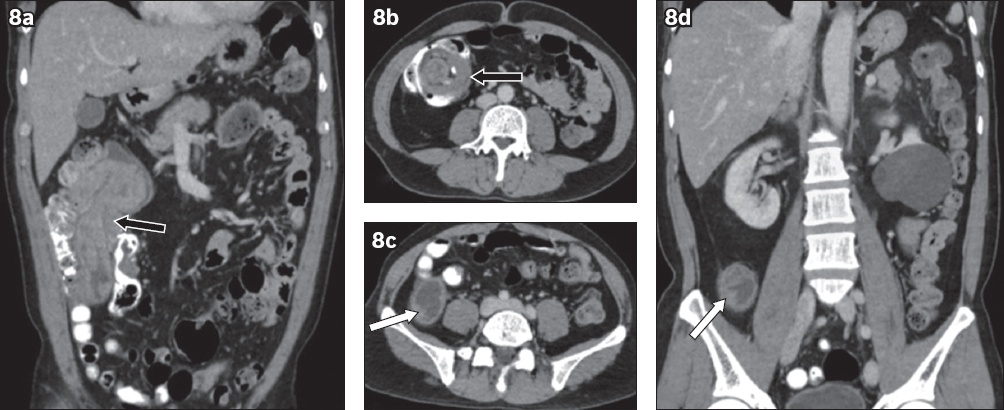
Fig. 8
A 50-year-old man presented with right iliac fossa pain. Contrast-enhanced (a) coronal and (b) axial CT images show appendico-colic intussusception (arrows in a & b) with a ‘target-like’ appearance in (b). (c) Axial and (d) coronal CT images show enhancing mural soft tissue in the dilated appendix (arrows in c & d), raising suspicion for underlying malignancy. Histopathological examination revealed a low-grade appendiceal mucinous neoplasm in association with tubulovillous adenoma.
Acute appendicitis with and without a coexisting mucocoele can be clinically indistinguishable. It is vital to identify the presence of a mucocoele, as the surgical approach needs to be altered to avoid rupture and consequently PMP, for which satisfactory treatment is usually difficult to achieve. CT features suggestive of a coexisting mucocoele encompass cystic dilatation of the appendix, mural calcification, luminal diameter greater than 1.3 cm, or an outer diameter greater than 1.5 cm. In particular, when the maximal luminal diameter of the appendix is greater than 1.3 cm, the sensitivity and specificity for diagnosing a mucocoele are 71.4% and 94.6%, respectively.(9)
Pseudomyxoma peritonei
PMP is a clinical syndrome defined as intraperitoneal accumulation of mucus due to mucinous neoplasia and is characterised by redistribution phenomenon. It includes mucinous ascites, peritoneal implants, omental caking and ovarian involvement. PMP can occur in both low- and high-grade lesions and may be due to spontaneous or iatrogenic perforation of the appendix.(3,7) It most commonly arises from appendiceal neoplasms, but other associated conditions include ovarian, colon, rectum, stomach, pancreas and urachal tumours.(3) Imaging findings are related to foreign body peritonitis with fibrotic response caused by spillage of mucus into the peritoneum.(6)
The diagnostic sign on CT is low-attenuation ascites with visceral scalloping due to implants (
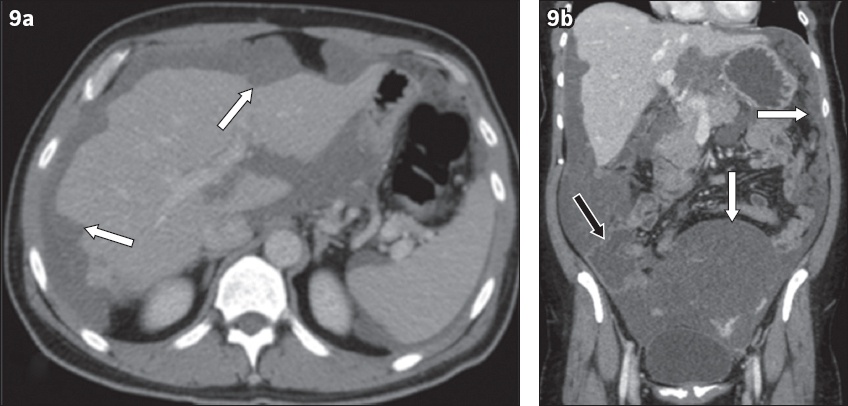
Fig. 9
A 53-year-old man presented with pseudomyxoma peritonei manifesting as increasing abdominal girth that resulted from a ruptured mucinous adenocarcinoma of the appendix. Contrast-enhanced CT (a) axial and (b) coronal CT images show widespread low-attenuation intraperitoneal locules that scallop the hepatic contour (arrows in a) causing a mass effect on the bowel loops (black arrow in b) as well as the mesentery (white arrows in b).
OTHER MANIFESTATIONS AND PITFALLS IN IMAGING
Perforation and abscess formation
In general, it is difficult to differentiate perforated non-tumoral appendicitis from perforated appendicitis secondary to an underlying appendiceal neoplasm.(5,9) In such patients, histopathology and follow-up imaging play an important role in its distinction (Figs.
Fig. 10
A 62-year-old woman presented with right iliac fossa pain. Unenhanced (a) coronal and (b) axial CT images show an abscess adjacent to the base of the appendix (white arrows in a & b) with dilatation of the tip of the appendix (arrowhead). Thin mural calcification (black arrow) is also noted. Histologic examination following surgery showed low-grade mucinous neoplasm of the appendix.
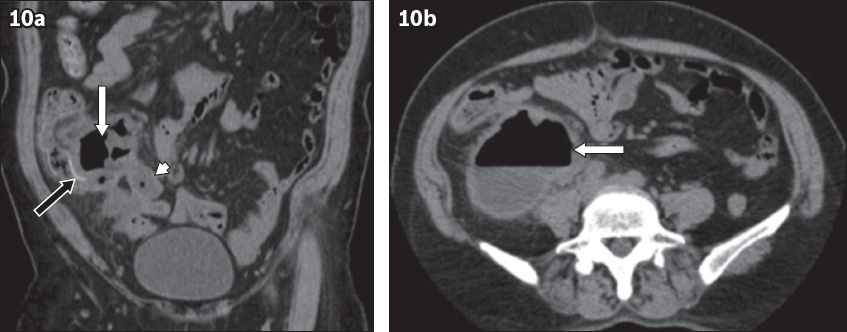
Fig. 11
A 45-year-old woman presented with right iliac fossa pain. Contrast-enhanced (a) coronal and (b) axial CT images show dilatation of the appendix with thickened enhancing walls (white arrows in a & b). There is a contained perforation with abscess formation at the tip of the appendix (black arrow in b). The diagnosis of low-grade appendiceal mucinous neoplasm was made after histopathological examination.
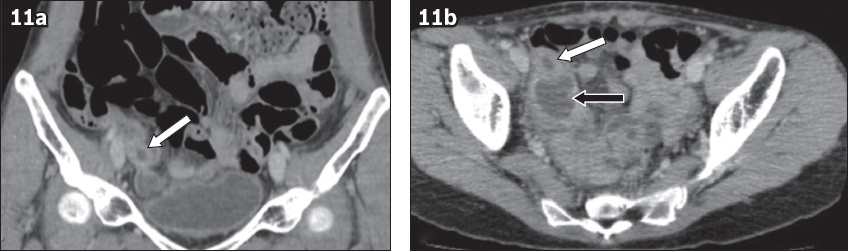
Fig. 12
Contrast-enhanced (a & b) axial and (c) coronal CT images of a 56-year-old woman show appendiceal mural thickening and enhancement (white arrows in a & c) with perforation and abscess formation (black arrows in a–c). A low-grade appendiceal mucinous neoplasm was found on histopathological examination.
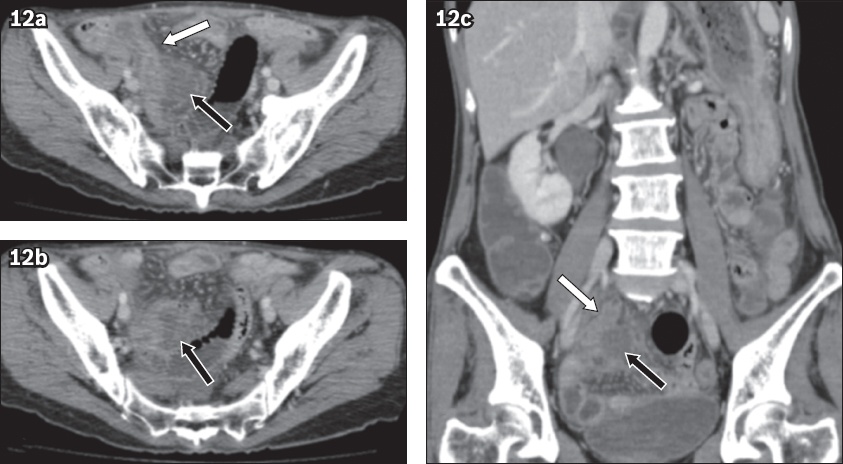
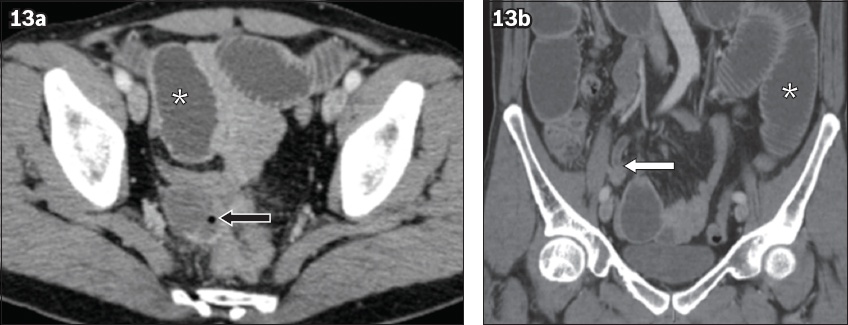
Fig. 13
A 46-year-old man with abdominal pain. Contrast-enhanced (a) axial and (b) coronal CT images show appendiceal mural thickening and enhancement with perforation at the tip (white arrow) and a resultant rim-enhancing abscess containing a gas pocket (black arrow). Dilatation of small bowel loops is suggestive of small bowel ileus (asterisk). Perforated mucinous adenocarcinoma was diagnosed postoperatively following histologic examination.
Intussusception
Intussusception in adults is uncommon, comprising about 5% of all intussusceptions and 1% of all cases of bowel obstruction. The majority of cases are caused by a neoplastic lead point (approximately 65%). The commonest site is the small bowel, followed by the large bowel.(10) By comparison, intussusception of the appendix is even rarer, accounting for 4% of all adult intussusceptions and 0.01% of appendicectomy specimens. The few reported cases in the available literature describe lead points consisting of an endometriotic deposit, appendiceal mucocoele, primary malignancy or metastasis.(11) Intussusceptions with a neoplastic lead point are usually longer (more than 3.6 cm) and have larger diameters (greater than 3.4 cm) than the non-neoplastic ones, while the degree of the dilation of the proximal small bowel is greater with a neoplastic lead point.(10)
The pathognomonic CT appearance is the bowel-within-bowel configuration, which may contain fat or mesenteric vessels (
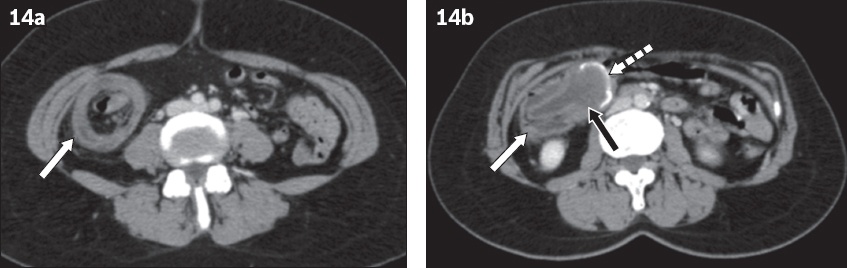
Fig. 14
A 57-year-old woman presented with right iliac fossa pain. Contrast-enhanced axial CT images show ileo-appendicocolic intussusception (white arrows in a & b) with (a) ‘target-like’ and (b) ‘cup and ball’ appearance in a patient with mucocoele of the appendix (black arrow in b). The dilated appendix with mural calcification (dashed arrow in b) was in keeping with a low-grade appendiceal mucinous neoplasm on histopathological examination.
Synchronous appendiceal and colorectal neoplasm
It has been reported that a quarter of patients with appendiceal cancer are found to have a synchronous or metachronous lesion elsewhere in the large intestine, as the appendix is embryologically derived from the large intestine and has a similar mucosal pattern (Figs.
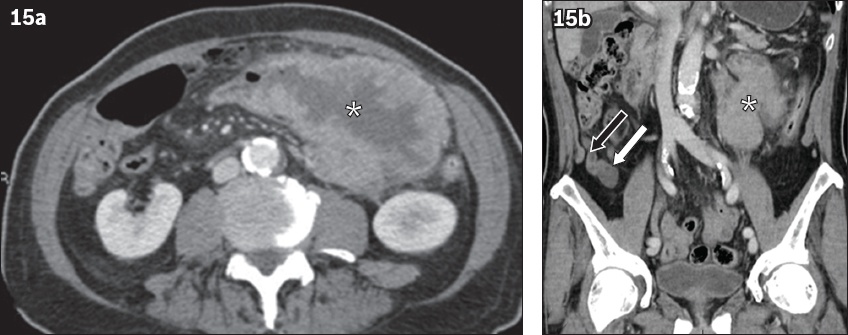
Fig. 15
A 79-year-old man had synchronous non-mucinous, colonic-type adenocarcinoma of the appendix and transverse colon. (a) Contrast-enhanced axial CT image shows irregular mural thickening and enhancement in the transverse colon (asterisks in a & b). (b) Coronal CT image shows soft tissue (white arrow) at the tip of the mildly dilated appendix (black arrow), in keeping with a synchronous tumour.
Small bowel obstruction
Mechanical obstructions caused by appendiceal neoplasms are rare.(14) An appendiceal neoplasm is often missed when it presents as small bowel obstruction, as the clinical features of small bowel obstruction may predominate the clinical picture.
CT helps in diagnosing the location, cause and degree of obstruction. If the zone of transition is in the right iliac fossa, it is important to consider an appendiceal pathology in the list of differential diagnoses for the cause of small bowel obstruction (
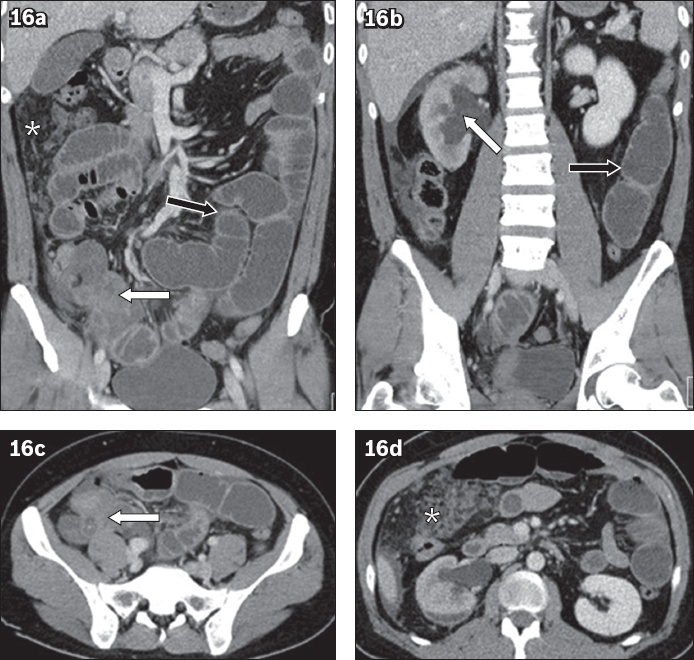
Fig. 16
A 35-year-old woman with abdominal pain. Contrast-enhanced (a & b) coronal and (c & d) axial CT images show a heterogeneous mass in the right lower abdomen (white arrows in a & c). There is omental thickening and nodularity (asterisks in a & d) as well as mechanical small bowel obstruction (black arrows in a & b). The mass involves the right ureter with resultant hydronephrosis (white arrow in b). Histopathology revealed a multifocal mucinous adenocarcinoma involving the appendix, mesentery and gallbladder (not seen on imaging).
OVARIAN PATHOLOGY
An appendiceal neoplasm may mimic an ovarian pathology due to overlapping imaging features (
Fig. 17
A 56-year-old woman presented with right iliac fossa pain. (a–c) Contrast-enhanced axial CT images show an abscess in the right adnexal region (black arrows in a & c) that is suspicious for a tubo-ovarian abscess. The possibility of a perforated appendiceal mucocoele was also raised in view of the close proximity of this lesion to the appendiceal tip (white arrow in c) and presence of curvilinear calcification (arrow in b). Histopathologic examination revealed a mucinous cystadenoma of the appendix.
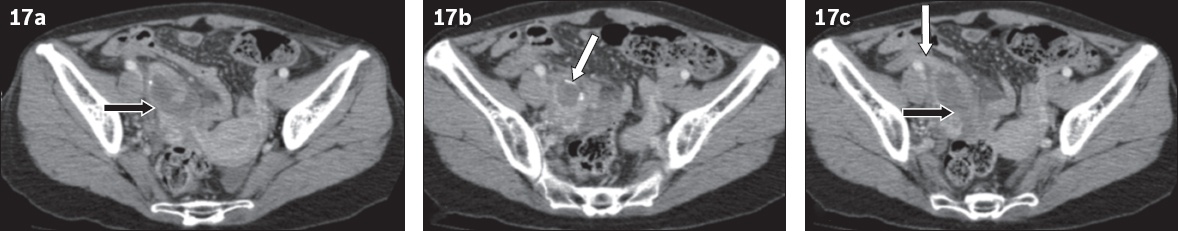
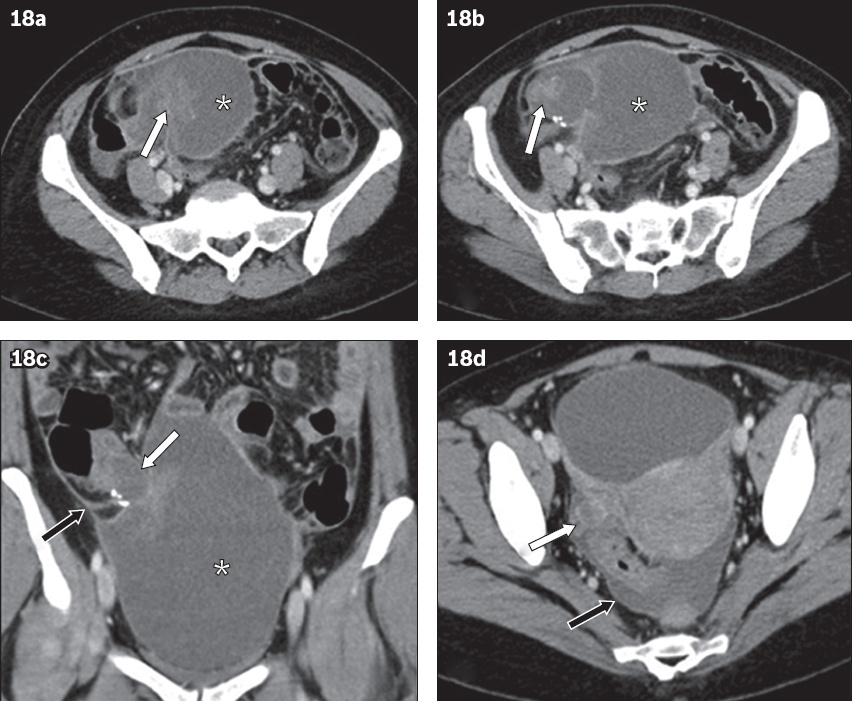
Fig. 18
A 47-year-old woman presented with pain in the right iliac fossa. (a & b) Contrast-enhanced axial CT images show a predominantly cystic mass (asterisks) in the right lower quadrant with an enhancing eccentric solid component (arrows in a & b). (c) Coronal and (d) axial CT images show peritoneal thickening and enhancement (black arrows in c & d). A preoperative diagnosis of a complex right ovarian mass with peritoneal deposits was made. The diagnosis of a low-grade appendiceal neoplasm with pseudomyxoma peritonei was established following surgery. In retrospect, (c) coronal CT image shows a short dilated tubular structure suggestive of the appendix (white arrow in c) leading into this cystic mass (asterisk in c). There is presence of calcification as well. (d) Axial CT image shows normal right ovary with corpus luteum (white arrow in d).
Hydroureteronephrosis
Appendiceal neoplasm causing hydroureteronephrosis is an uncommon but known complication. A right lower quadrant mass with resultant hydroureteronephrosis should prompt the reporting radiologist to consider an underlying appendiceal neoplasm (
CONCLUSION
In all patients being evaluated for lower abdominal pathologies, the appendix should be looked at and carefully assessed for the presence of suspicious features (
SMJ-60-182.pdf
ACKNOWLEDGEMENT
We would like to thank Dr Ahmad M Aljefri, Consultant Radiologist, King Fahd Medical City, Medical Imaging Administration, Riyadh, Kingdom of Saudi Arabia, for contributing the CT images for


