INTRODUCTION
The acromioclavicular joint (ACJ) is a key component of the shoulder girdle which, despite its small size, may be affected by a spectrum of pathologies, including traumatic, degenerative, infective, inflammatory and metabolic causes. Radiography, ultrasonography (US), computed tomography (CT) and magnetic resonance (MR) imaging are the main imaging modalities for evaluating the ACJ. We discuss the key anatomy and imaging features of various ACJ lesions.
ANATOMY
The ACJ is a diarthrodial synovial joint located between the lateral end of the clavicle and the medial acromion (
Fig. 1
Line diagram shows the anatomy of the acromioclavicular joint and the coracoacromial, acromioclavicular and coracoclavicular ligaments.
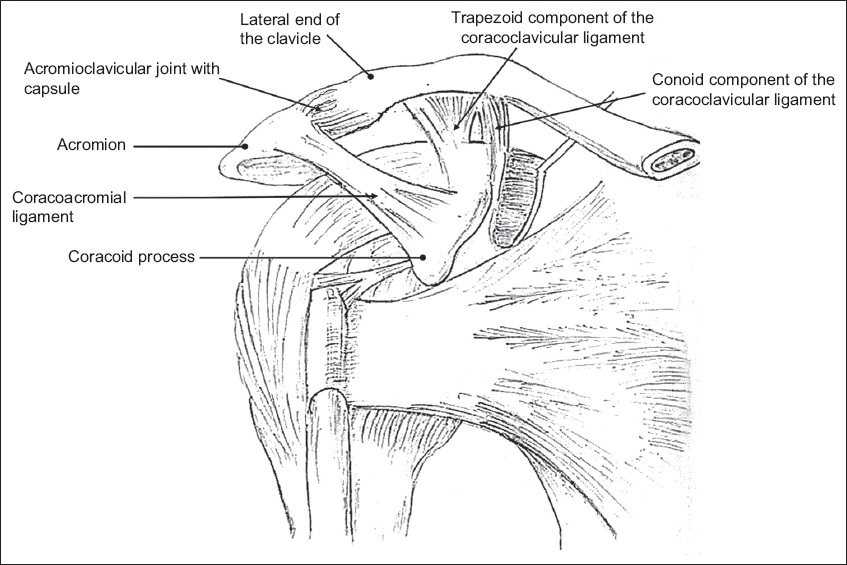
Fig. 2
Imaging anatomy of a normal acromioclavicular joint (ACJ) and related ligaments on coronal T1-W MR images of the left shoulder. (a) Coronal image shows the hypointense articular disc (arrowheads) within the ACJ and the trapezoid component of the coracoclavicular (CC) ligament seen as a fan-shaped striated hypointense structure (arrow). (b) Slightly posterior coronal image shows the medial conoid component of the CC ligament (arrow). Both components of the CC ligament link the superior portion of the coracoid process to the undersurface of the clavicle. The superior acromioclavicular ligament (arrowheads) blends with the ACJ capsule.
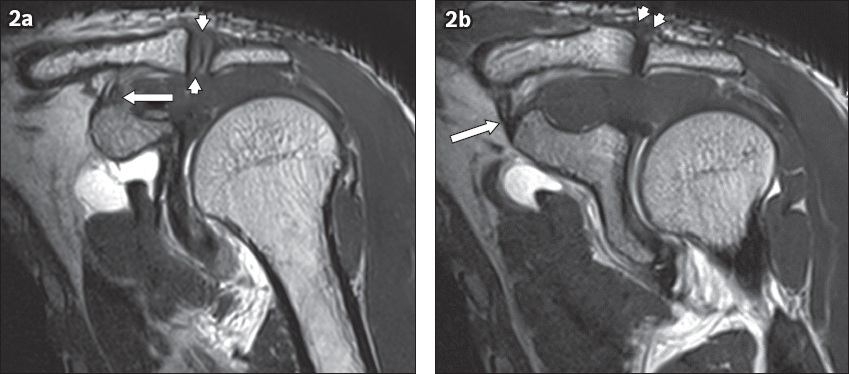
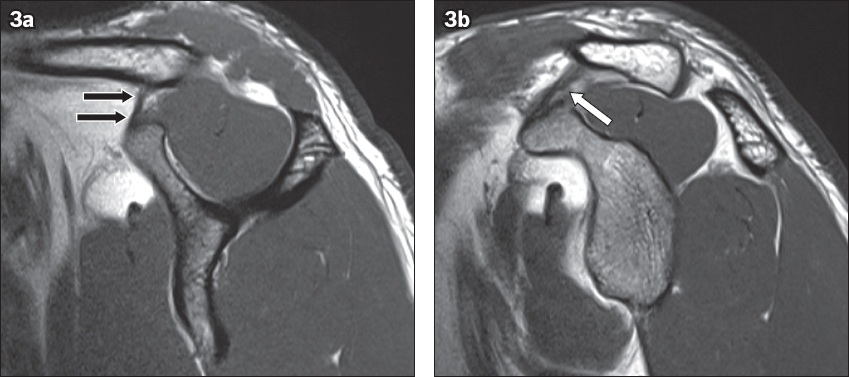
Fig. 3
Imaging anatomy of the coracoclavicular (CC) ligament on sagittal T1-W MR images (same patient as
IMAGING TECHNIQUES
Radiographs enable a basic and quick initial assessment of the ACJ. They serve as a simple and inexpensive preliminary investigation to assess subluxations/dislocations, AC and CC distances, and provide an initial grading of ACJ injuries.(1) Radiographs also help in assessment of ACJ arthritis by depicting osteophytes and reduced joint space in degeneration, articular marginal erosions in inflammation and bony destruction in sepsis.(3,4) Comparison with the contralateral joint and regional joint involvement can also be easily and rapidly assessed. Fractures, gross erosions, and osteolytic and sclerotic lesions are usually initially detected on radiographs. Subtle erosions, early osteolytic lesions, soft tissue masses and occult fractures are not always seen on radiographs and require further imaging.(3,4)
US is helpful for imaging the superficially located ACJ, with the advantages of portability, rapid assessment and no ionising radiation. US is also useful to guide needle placement for joint or bursal fluid aspirations that are helpful in the diagnosis of various arthropathies (e.g. sepsis, gout). US-guided analgesic and/or steroid injections may also provide short-to-medium-term pain relief in ACJ osteoarthritis.(4)
CT is useful for assessing occult osseous abnormalities, including small undisplaced fractures, minor subluxations, erosions and osteolytic lesions. Dual-energy CT allows an accurate diagnosis to be established in gout.(5)
MR imaging is the modality of choice for assessment of soft tissues, including the articular capsule, ligaments, fibrocartilage, surrounding tendons and muscular attachments around the ACJ.(1) Capsuloligamentous injuries ranging from simple sprains to complete tears are clearly delineated. MR imaging is ideal for detecting occult fractures, marrow oedema (due to injuries, inflammation or infection) and early erosions.(1)
LESIONS OF THE ACROMIOCLAVICULAR JOINT
Trauma
Owing to its subcutaneous location, the ACJ is susceptible to both direct and indirect trauma. Road traffic accidents and collision sports remain the leading causes. Direct forces result in ACJ injury, clavicular fracture or a combination. Indirect forces are less common and comprise impaction injuries transmitted from the elbow or fall on an outstretched hand. Ligamentous injuries of the ACJ include mild sprains involving the AC ligaments, moderate injuries involving the CC ligament or severe injuries involving the deltotrapezius muscular attachments.(6)
Rockwood classification
Grading of ACJ injuries is based on the extent of involvement of both static and dynamic stabilisers, and the degree and direction of clavicular displacement. The well-accepted Rockwood classification describes six grades of injuries (
Fig. 4
Line diagrams show the Rockwood classification of acromioclavicular joint injuries with Grades (a) I; (b) II; (c) III; (d) IV; (e) V; and (f) VI injuries, and depict the site of ligamentous injuries with the extent and direction of clavicle displacement.(7)
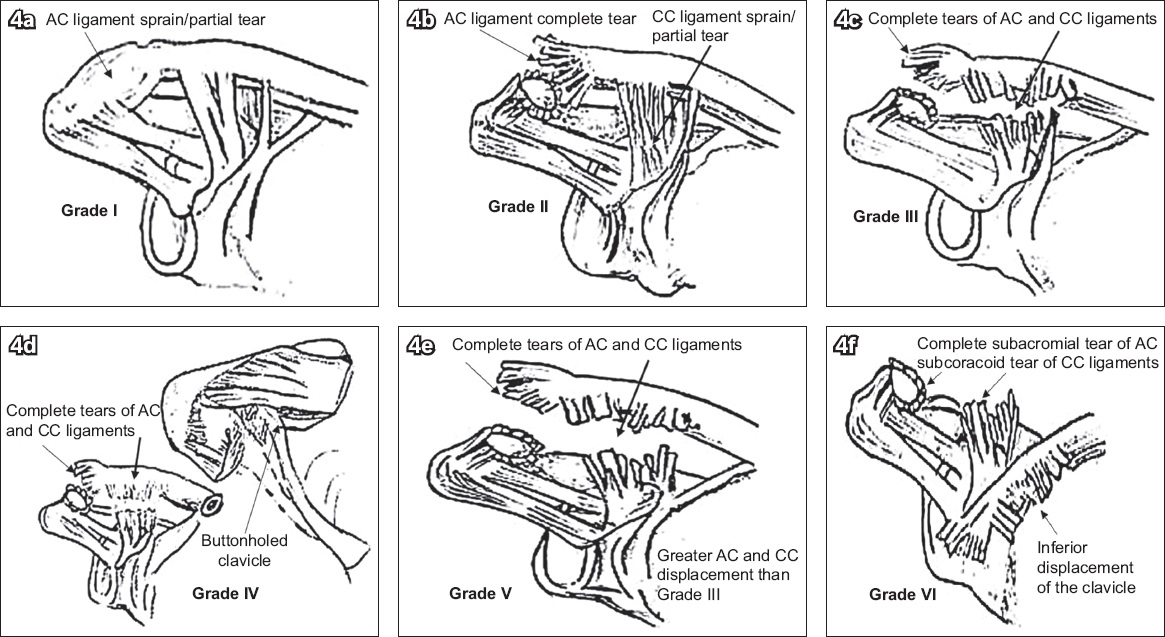
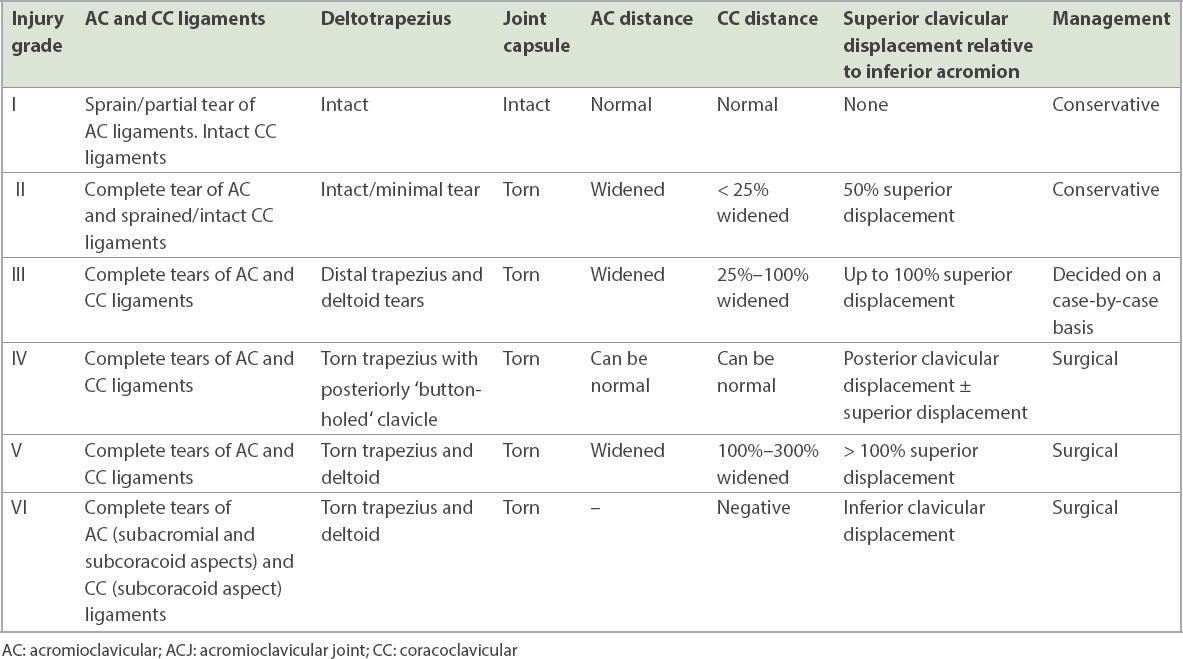
Table I
Summary of Rockwood classification of ACJ injuries.(1,7)
Imaging
Anteroposterior, scapular-Y and axillary radiographic views are useful in suspected ACJ injuries. AC distance > 7 mm indicates widening (
Fig. 5
Rockwood Grade I injury. Frontal radiograph of a 36-year-old man with a clinical history of right-sided acromioclavicular joint (ACJ) injury shows slight widening of the right ACJ (arrow) compared to the normal left side. There is no superior clavicle displacement relative to the acromion.
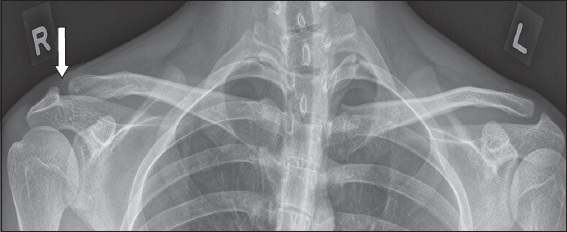
Fig. 6
Rockwood Grade II injury. Frontal right shoulder radiograph of a 30-year-old man presenting with acromioclavicular joint pain shows < 50% superior clavicular displacement relative to the acromion with no coracoclavicular widening.

Fig. 7
Rockwood Grade III injury treated surgically. (a) Non-weight-bearing and (b) weight-bearing frontal radiographs of the left shoulder of a 25-year-old man who complained of pain after weight-lifting exercise show superior displacement of the clavicle relative to acromion and widening of acromioclavicular and coracoclavicular distances on the weight-bearing radiograph. Note the importance of the weight-bearing view in this case, which converted the Rockwood Grade II injury in (a) with up to 50% superior clavicular displacement to Grade III in (b) with 100% superior clavicular displacement (arrows). (c) The patient subsequently underwent hook plate surgical fixation.
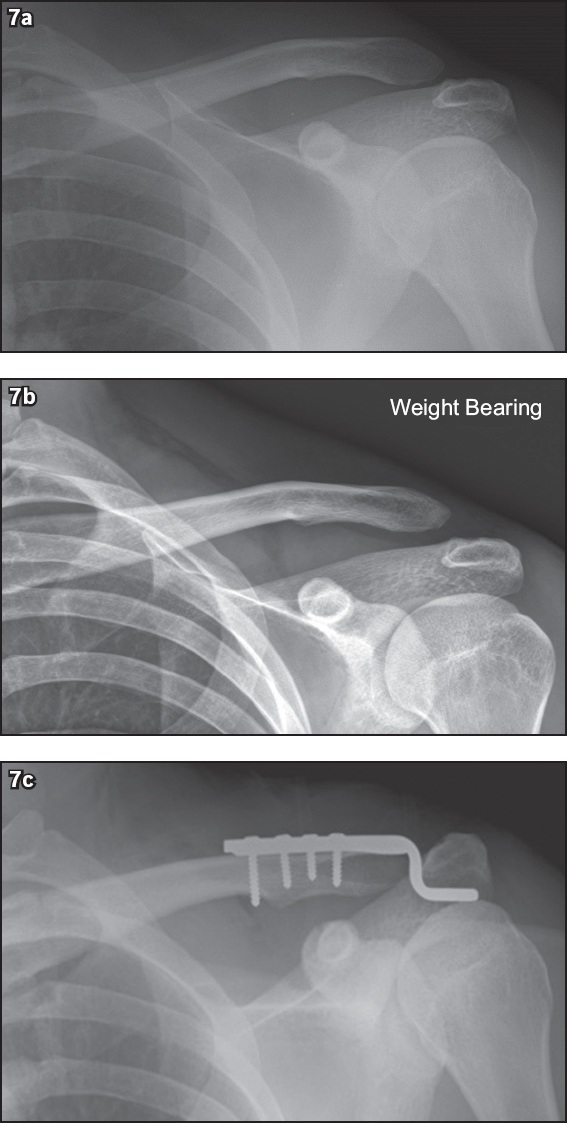
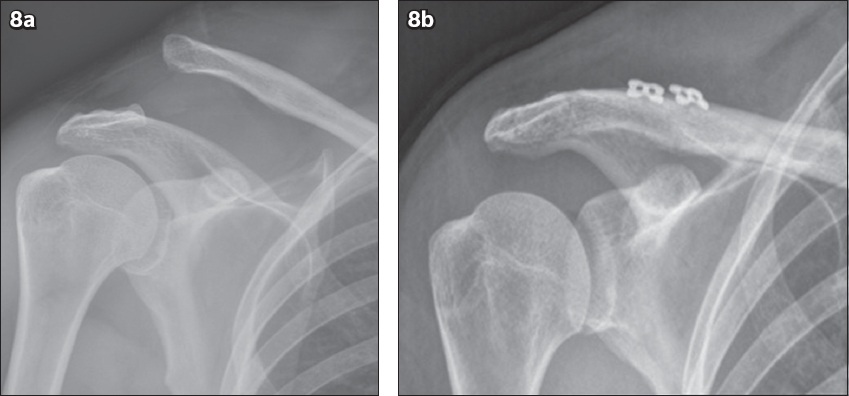
Fig. 8
Rockwood Grade V injury treated surgically. (a) Frontal right shoulder radiograph of a 43-year-old man shows > 100% superior clavicle displacement relative to acromion and markedly-widened corcoclavicular distance. (b) Post-fixation radiograph following surgical repair using the triple endobutton technique shows a well-aligned acromioclavicular joint.
Zanca view is an anteroposterior, 10–15º cephalad, erect ACJ radiograph for identification of small fractures. Axillary view is better for Grade IV injuries (posterior clavicular displacement but normal AC and CC distances).(1) CT is useful to detect occult bony injuries for preoperative planning and for detecting complications such as distal clavicular osteolysis.(7) The extent and severity of ligament and deltotrapezius injuries are directly visualised on MR imaging.(2) Ligamentous and muscle damage/discontinuity, soft tissue/marrow oedema and fluid/blood are depicted on T2-weighted (T2-W) fat-suppressed sequences (
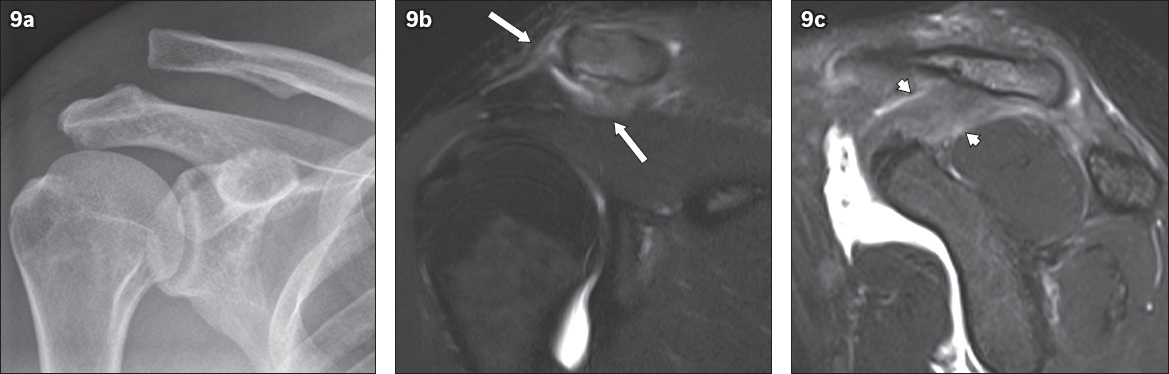
Fig. 9
MR imaging features of a Rockwood Grade III injury. (a) Frontal radiograph of the right shoulder of a 28-year-old man with a history of shoulder injury shows slightly over 100% superior clavicular displacement relative to acromion and widened coracoclavicular (CC) distance, in keeping with a Rockwood Grade III injury. (b) Coronal and (c) sagittal fat-suppressed T2-W MR images confirm disruption of the acromioclavicular ligaments and acromioclavicular joint capsule (arrows), and of the CC ligament (arrowheads).
Post-traumatic sequelae
Post-traumatic sequelae include late-onset osteoarthritis and CC ligamentous ossification.(2,8) Post-traumatic distal clavicular osteolysis occurs 6–8 weeks after injury and is self-limiting. Radiographs and MR imaging show gradual resorption of the distal end of the clavicle and subarticular marrow oedema (
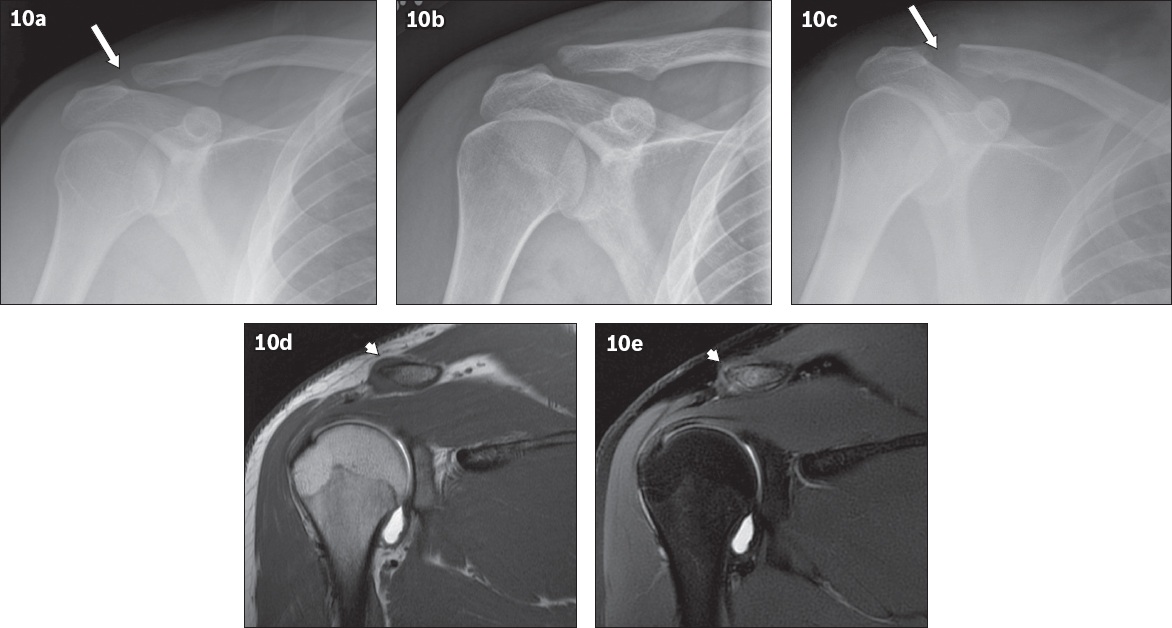
Fig. 10
Post-traumatic distal clavicular osteolysis. (a) Initial frontal radiograph of a 21-year-old man with progressive right shoulder pain and a history of weight-lifting shows equivocal acromioclavicular joint (ACJ) widening (arrow). (b) Radiograph taken one month later owing to persistent pain shows irregularity and osteolysis of the lateral clavicular cortex with slight ACJ widening. (c) Follow-up radiograph after eight months shows progressive distal clavicular osteolysis with interval increase in ACJ widening (arrow). Coronal (d) T1-W and (e) fat-suppressed T2-W MR arthrographic images show post-traumatic osteolysis of the distal end of the clavicle, with T1-hypointense and T2-hyperintense bone marrow signal, and associated ACJ capsular thickening (arrowheads).
Osteoarthritis
Osteoarthritis is the most common non-traumatic disorder of the ACJ. Repeated microtrauma results in chondral wearing and articular disc degeneration. It is common in weightlifters, basketball players and swimmers.(4) Anteroposterior and Zanca radiographic views show articular marginal osteophytes and sclerosis, subchondral cysts and joint space narrowing (
Fig. 11
Acromioclavicular joint (ACJ) osteoarthritis. (a) Frontal shoulder radiograph of a 70-year-old woman with left shoulder pain shows osteoarthritic changes of the ACJ with joint space narrowing, acromial-sided subchondral cysts and peri-articular osteophytes. (b) US image shows corresponding capsular hypertrophy (arrows) with articular disc degeneration (asterisk).
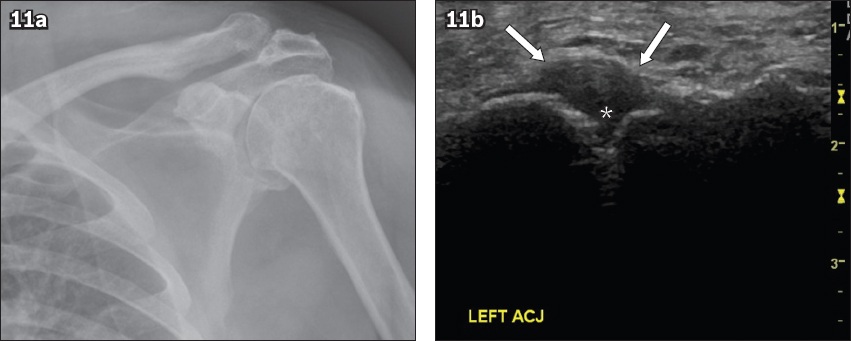
US-guided ACJ injection using an admixture of short- or long-acting local anaesthetic and corticosteroid may be performed for symptomatic pain relief. Caudal osteophytes and capsular hypertrophy are predictive of favourable response to intra-articular injection.(4) Rotator cuff tears combined with ACJ degeneration can rarely present as cystic swelling overlying the ACJ. This swelling is due to glenohumeral joint fluid tracking into the ACJ through a chronic supraspinatus tear and further extending into the subcutaneous plane (
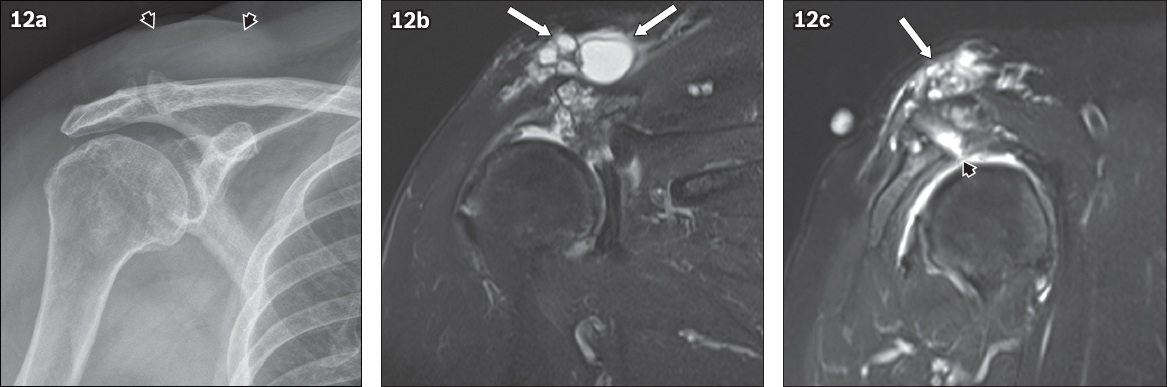
Fig. 12
Geyser sign in acromioclavicular joint (ACJ) osteoarthritis. (a) Frontal radiograph of a 56-year-old woman presenting with swelling over the right shoulder shows ACJ osteoarthritis and acromiohumeral narrowing due to severe rotator cuff arthropathy, with a large soft tissue swelling over the superior and medial aspect of the ACJ (black arrowheads). (b) Coronal and (c) sagittal STIR (short tau inversion recovery) MR images show a large multiloculated cystic lesion (arrows) located adjacent to the superior aspect of the ACJ. This cystic lesion communicates with the glenohumeral joint via the ACJ and a full-thickness tear of the supraspinatus tendon, best seen on the sagittal image (black arrowhead). This is typical of the geyser sign.
Rheumatoid arthritis
Simultaneous involvement of the glenohumeral and AC joints is common in rheumatoid arthritis (RA). The pathophysiology is primarily due to formation of an inflammatory synovial pannus causing destruction of the bare areas of joint cartilage and articular bony margins, tendoligamentous structures and capsule. Ankylosis, deformities and secondary osteoarthritis are end-stage sequelae.(10,11)
Imaging features resemble those at other synovial joints. US and contrast-enhanced MR imaging are the preferred modalities in early RA for delineating the pannus, articular marginal erosions, joint and bursal fluid. Acute pannus is hypervascular and T2-hyperintense, whereas chronic pannus is hypovascular and hypointense on T1-W and T2-W sequences, resembling fibrous tissue.(11) In early RA, periarticular osteopenia may be the only finding on radiographs. Erosive changes at the acromial articular surface and distal clavicle are radiographic features of subacute to chronic RA, with resultant apparent ACJ widening (
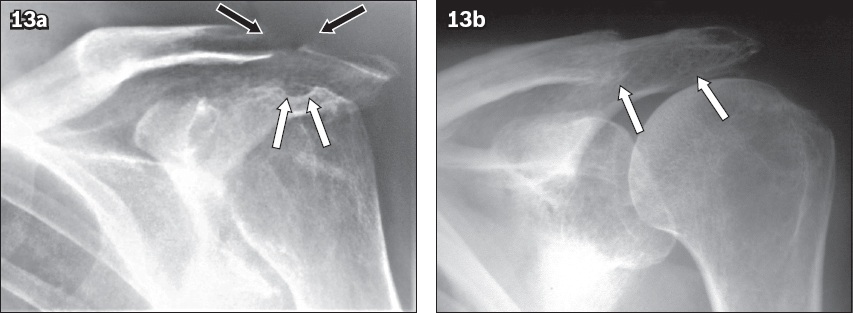
Fig. 13
Rheumatoid arthritis. (a) Frontal left shoulder radiograph of a 55-year-old woman with known rheumatoid arthritis shows a widened acromioclavicular joint (ACJ) owing to erosive changes and tapered resorption of the distal end of the clavicle and medial acromion (black arrows). Note the erosions at the humeral head (white arrows) and arthritic changes at the glenohumeral joint. (b) Frontal left shoulder radiograph of a 66-year-old woman with known rheumatoid arthritis shows a grossly widened ACJ with erosive resorption of the distal end of the clavicle and the medial aspect of the acromion (arrows).
Crystalloid arthritis
Gout occurs owing to deposition of monosodium urate (MSU) crystals in synovial and periarticular tissues, causing both acute and chronic synovitis and monoarthritis. The chronic phase is characterised by formation of intra- and periarticular tophi, leading to destructive arthropathy. Chronic gout produces the classic radiographic findings of ‘punched-out’ periarticular erosions with overhanging margins. The end stage of disease is marked by loss of joint space and osseous mineralisation.(5)
The shoulder is an uncommon site for gout. Nonetheless, gout is still a consideration in ACJ monoarthritis, especially in patients with background renal failure.(5) Radiographs may not show the classic overhanging gouty erosions until the late stages, and it is important to have a high index of clinical suspicion. Laboratory detection of negatively birefringent MSU crystals through US-guided joint aspiration remains the diagnostic gold standard for gout.(5,12) Non-specific features of synovial thickening and effusions may be seen on US and MR imaging in other inflammatory (e.g. RA, pseudogout) and infective arthropathies. MR imaging is more sensitive than conventional radiographs for detecting erosions and tophi (
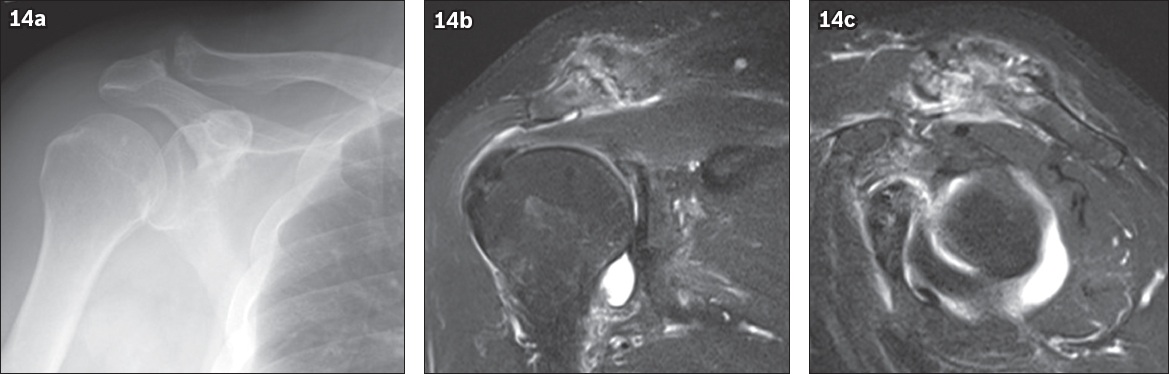
Fig. 14
Gout. (a) Frontal right shoulder radiograph of a 67-year-old man with known gout presenting with pain shows articular marginal sclerosis and well-defined juxta-articular erosions at the acromioclavicular joint. (b) Coronal and (c) sagittal fat-suppressed T2-W MR images show active inflammation of the entire joint with reactive periarticular synovitis, subarticular marrow oedema, and juxta-articular erosions in the acromion and distal clavicle. The full disease extent is much better depicted on MR images compared to radiographs.
Calcium pyrophosphate deposition disease is caused by deposition of calcium pyrophosphate crystals in the joints and periarticular tissues, leading to either acute inflammatory monoarthritis/pseudogout or chronic polyarticular arthropathy resembling osteoarthritis.(13) The shoulder (glenohumeral and AC joints) is commonly affected, and ACJ synovitis has been associated more with pseudogout than with gout.(14) Pseudogout must be suspected with radiographic changes of disproportionate and rapidly progressive osteoarthritis-like changes at the ACJ. Ancillary features include chondrocalcinosis of the articular disc, large subchondral geodes and soft tissue calcifications. The role of other modalities is limited to US-guided joint aspiration of the calcium pyrophosphate crystals. Septic arthritis and gout remain the main differentials.(13)
Septic arthritis
ACJ sepsis requires a high index of suspicion because of its clinical similarity to glenohumeral joint sepsis and susceptibility to rapid destruction due to the small size of the joint. Contiguous and haematogenous spread are the common routes of infection. Staphylococcus and granulomatous infections are common causes.(15) ACJ sepsis often cannot be readily differentiated from inflammatory or crystalloid arthropathies based on imaging alone. Radiographs and US images are not diagnostic and may show non-specific erosions, effusion and synovitis. MR imaging findings of synovial enhancement, marrow and soft tissue oedema, articular marginal erosions, accompanying clavicular osteomyelitis and rim-enhancing collections are useful features in the clinical context of sepsis (
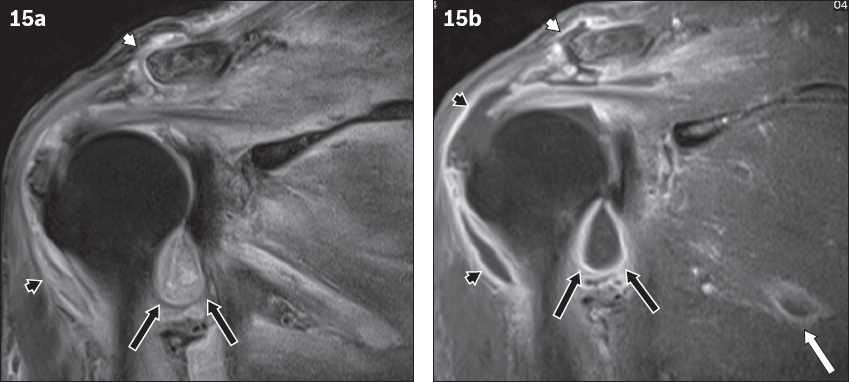
Fig. 15
Septic arthritis. Coronal (a) fat-suppressed T2-W and (b) contrast-enhanced fat-suppressed T1-W MR images of a 40-year-old woman with complaints of pain and erythema over the right shoulder show a rim-enhancing effusion in the right acromioclavicular joint (white arrowheads) with adjacent subarticular bone changes compatible with septic arthritis. There is concurrent glenohumeral septic arthritis (black arrows), subdeltoid infective bursitis (black arrowheads) and pyomyositis (white arrow).
Seronegative spondyloarthropathies
The seronegative spondyloarthropathies (SpAs) comprise ankylosing spondylitis (AS), reactive (Reiter) arthritis, psoriatic arthropathy and enteropathic arthritis. The spine and sacroiliac joints remain the predominant sites of involvement in all SpAs. Oligoarticular and asymmetric peripheral joint arthritis and enthesitis is common in the shoulder and hip joints.(16) The most frequently involved peripheral joint in AS is the shoulder girdle, with enthesitis, synovitis and bursitis being prominent around the anterolateral clavicle and ACJ.
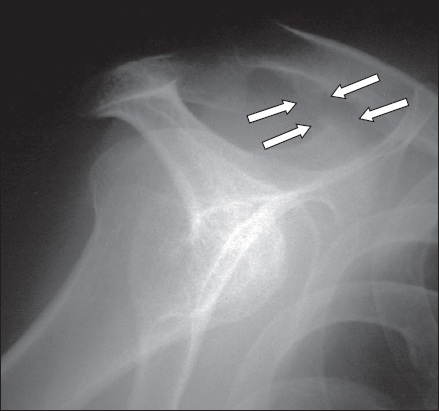
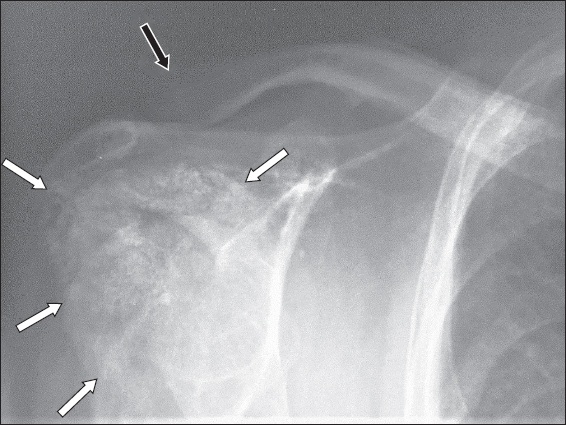
Imaging helps to identify these changes at the attachments of the deltoid to anterior clavicle and acromion, CC ligament from the coracoid process to the undersurface of the clavicle and rotator cuff to the greater tuberosity.(16) Enthesopathic radiographic findings include erosions, osteitis, ‘whiskering’ margins and ossifications at the CC ligamentous attachments (
Fig. 16
Ankylosing spondylitis. Scapular-Y radiograph of the right shoulder of a 48-year-old man with known ankylosing spondylitis shows enthesopathic changes in the form of ossification at the coracoclavicular ligamentous attachments to the superior coracoid process and undersurface of the clavicle, giving a ‘whiskered’ appearance (arrows).
Hyperparathyroidism
Both primary and secondary hyperparathyroidism commonly affect the ACJ. Radiographic findings at the lateral end of the clavicle include generalised osteopenia, distal clavicular subchondral/subperiosteal resorption, subligamentous bony resorption along the clavicular attachment of CC ligament and apparent widening of the ACJ (
Fig. 17
Hyperparathyroidism. Frontal radiograph of the right shoulder of a 45-year-old man with hyperparathyroidism secondary to renal osteodystrophy shows generalised osteopenia, distal clavicular resorption (black arrow) and florid dystrophic calcifications around the shoulder joint (white arrows).
CONCLUSION
The ACJ is a small joint that can be affected by a varied range of pathologies. Specific imaging features of traumatic, infective or inflammatory conditions in the appropriate clinical scenario are useful to characterise the pathological condition in the majority of the cases. Radiographs and US remain simple first-line imaging investigations. MR imaging is best reserved for complex inflammatory/infective/crystalloid arthritis with equivocal clinicoradiographical findings.
SMJ-63-139.pdf


