Abstract
Jejunal artery aneurysms are rare, with only six cases reported in the literature to date. Endovascular embolisation of the jejunal artery is rarely performed. Herein, we report the case of a 57-year-old man who successfully underwent endovascular embolisation for bleeding caecal diverticulosis, during which a 9-mm fusiform jejunal artery aneurysm was incidentally diagnosed. Subsequently, the jejunal aneurysm was successfully embolised using Vortex coils.
INTRODUCTION
Endovascular embolisation of the jejunal artery is not a common procedure due to the rarity of its clinical indications. Coupled with the fact that jejunal arterial branches have one or few arcades, there is, theoretically, a risk for bowel ischaemia following embolisation. To date, there are only six case reports of jejunal artery aneurysms published in the literature, five of which underwent endovascular embolisation.(1-6) We present a case of successful embolisation of a 9-mm jejunal artery aneurysm, which was found incidentally, and a brief review of the literature.
CASE REPORT
We present the case of a 57-year-old non-smoker with a significant past medical history of colon diverticulosis, which was first diagnosed in April 2009 after he presented with haematochezia. Colonoscopy performed then had revealed florid caecal, ascending hepatic flexure and sigmoid diverticulosis. He was readmitted in July 2013 with a two-day history of 14 episodes of haematochezia. It was similar to his previous 2009 presentation. The patient did not have any symptoms of intestinal obstruction or ischaemic bowel, nor did he report any constitutional or anaemic symptoms. He had no family history of inflammatory bowel disease.
On physical examination, the patient was alert, afebrile, normotensive (blood pressure: 113/64) and not tachycardic (heart rate: 89 bpm). His abdomen was soft and non-tender, with no sign of peritonitis. Digital rectal examination revealed fresh blood stains but no melaena or mass. Proctoscopy was negative for haemorrhoids and rectal ulcers. Full blood count revealed normocytic, normochromic anaemia, with haemoglobin level at 8.0 g/dL. Coagulation profile, liver function tests and cardiac enzymes were all normal. Plain chest and abdominal radiography did not reveal any bowel obstruction or viscus perforation. After resuscitation and transfusion with 3 units of packed red blood cells, his haemoglobin level improved to 9.4 g/dL.
Colonoscopy performed the next day after bowel preparation, demonstrated pan-colonic diverticulosis with altered blood staining the left colon. However, there was no evidence of any active bleed. Intubation of the terminal ileum did not suggest bleeding proximally from the small intestine.
Although haemodynamically stable, the patient had three further episodes of haematochezia, with haemoglobin level dropping to 7.5 g/dL. Computed tomography (CT) mesenteric angiography revealed bleeding colonic diverticulosis, with active contrast extravasations at the caecum and proximal ascending colon. The patient then underwent successful endovascular embolisation of the bleeding caecal vasa recta with two 3-mm Vortex coils and one 2-mm Helical coil.
During the procedure, there was an incidental finding of a 9-mm fusiform jejunal artery aneurysm (
Fig. 1
Pre-embolisation CT mesenteric angiogram shows a 9-mm fusiform jejunal artery aneurysm (arrow).
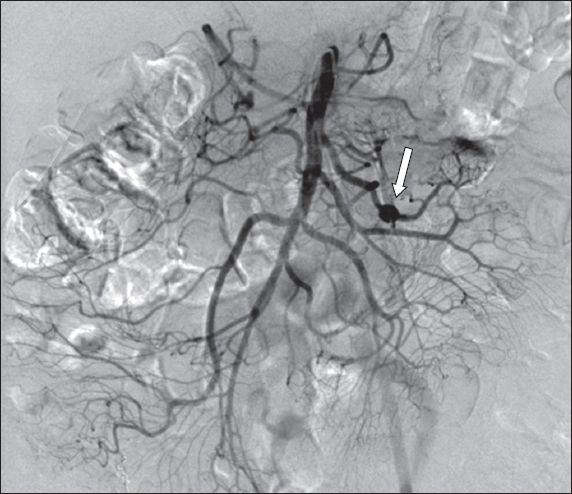
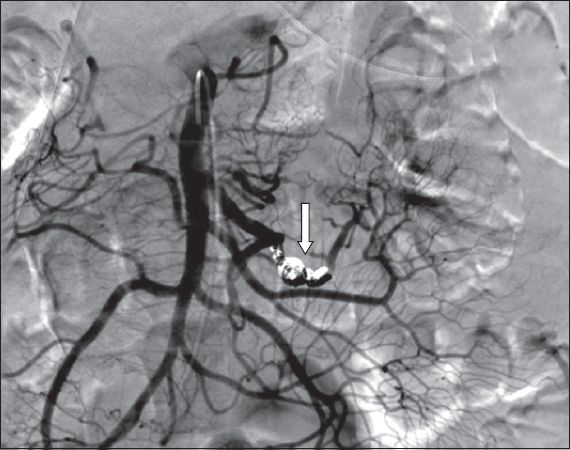
Fig. 2
Post-embolisation CT mesenteric angiogram shows complete occlusion of the jejunal branch, with no filling of the aneurysmal sac (arrow). Distal bowel was well perfused via a jejunal collateral network.
The patient had an uneventful post-procedure recovery and was discharged four days later with no further bleeding episodes or ischaemic complications. At review one month after discharge, the patient was well, and had no significant complaints and normal haemoglobin levels.
DISCUSSION
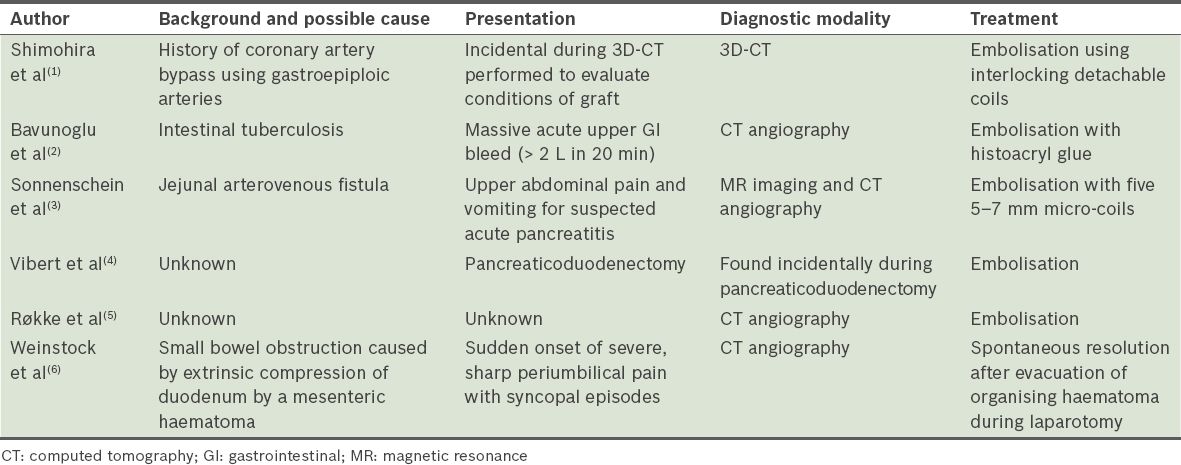
Jejunal artery aneurysms are rarely seen. There are only six such cases reported in the literature (
Table I
Published case reports of jejunal aneurysms or pseudoaneurysms.
Traditionally, treatment of splanchnic artery aneurysms has been open surgical intervention due to their late presentation of aneurysmal ruptures.(7-9) However, with the widespread use of CT angiography, there is increased detection of asymptomatic splanchnic artery aneurysms, in which treatment by angio-embolisation has been shown to be effective as a first-line treatment with few complications and low recurrence rates.(2,5,7-8,11-15) First described in 1974, angiographic diagnosis and treatment of gastrointestinal haemorrhage has since progressed significantly with advances in microcatheter technology, digital fluoroscopy and increased experience of interventional radiologists. Numerous reports have documented its safety and high rates of success of over 90%.(11) However, these successes have mainly been limited to larger vessels supplying the colon.(11-13) Treatment outcomes of embolisation of small bowel vessels are currently unclear, although our literature review documented success in all five attempted endovascular embolisation within six case reports (
In conclusion, the growing literature documenting successful embolisation of jejunal artery with low incidences of bowel ischaemia and recurrence, coupled with the increasing expertise of intervention radiology and vascular surgery, suggests that endovascular intervention for aneurysms of the jejunal artery is gaining credence as a safe treatment for jejunal artery aneurysms.


