Dear Sir,
Takotsubo cardiomyopathy (TC) is an uncommon, underdiagnosed condition that mimics an acute myocardial infarction (AMI). It is known to be precipitated by emotional or physical stressors, particularly following stress from major surgery. Myasthenic crisis, another rare presentation, occurs when neuromuscular respiratory weakness warrants invasive airway support. In the past decade, several published case reports have found associations between these two conditions, predominantly affecting women. We herein report on a case of TC with concomitant myasthenic crisis. This case is unique due to the atypical presentation with throat tightness as the predominant symptom. We outline the diagnostic pitfalls as well as the principles of management in this patient.
A 59-year-old Chinese woman had a one-month history of recently diagnosed seropositive generalised myasthenia gravis (MG) that was being treated with prednisolone and pyridostigmine. The patient presented acutely with two days of throat tightness, swallowing difficulty, proximal weakness and orthopnoea. No symptoms of chest pain or tightness were noted. On examination, she was alert, non-tachypnoeic and spoke in full sentences. Her vital signs were stable on arrival. Cardiovascular and respiratory examinations were unremarkable. Neurological examination revealed bilateral ptosis and proximal weakness with normal tone and reflexes. There was suspicion of an MG flare in view of her symptoms; an arterial blood gas test revealed normal results and excluded the diagnosis of respiratory failure. Electrocardiography (ECG) was also done to rule out acute coronary syndrome.
ECG revealed ST elevations in the anterior leads V1–V4 and lateral leads I and aVL, with reciprocal depressions in the inferior leads II and aVF (
Fig. 1
ECG shows ST elevations in the anterior leads V1–V4 and lateral leads I and aVL, with reciprocal depressions in the inferior leads II and aVF.
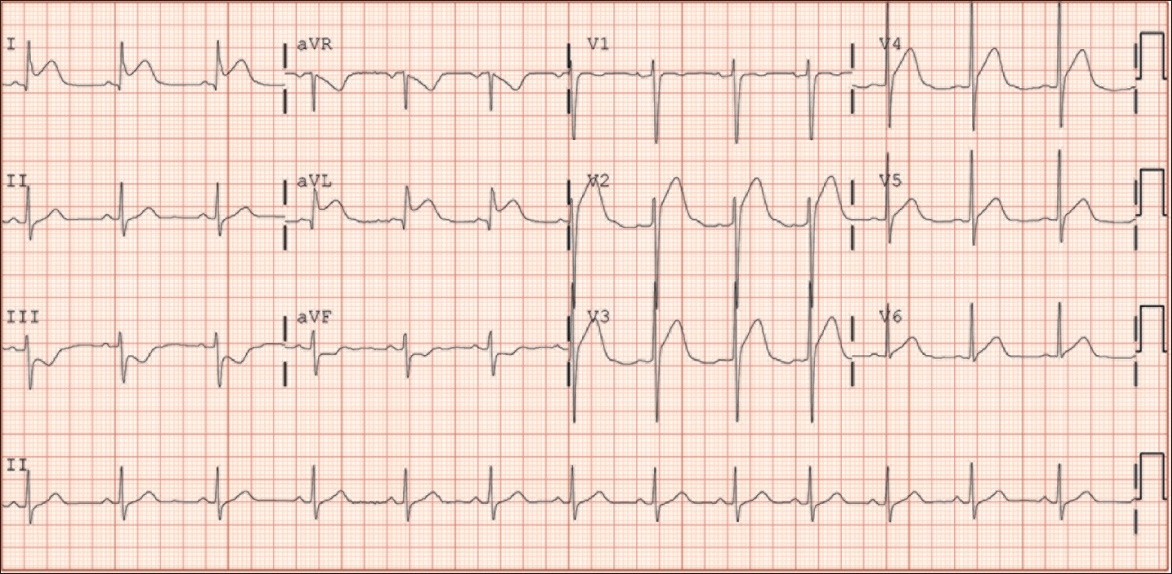
Fig. 2
Coronary angiogram shows non-obstructive disease in the left anterior descending artery.

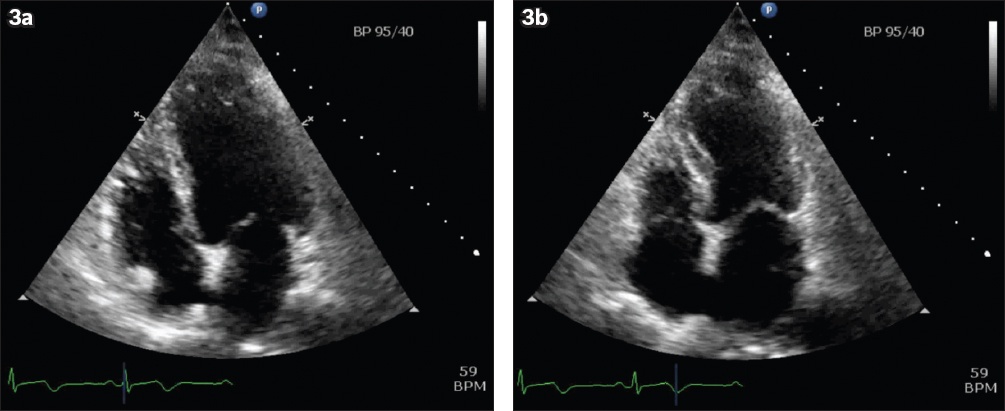
The patient suddenly developed severe respiratory distress before a left ventriculogram could be performed for confirmation. Acute myasthenic crisis was suspected. The decision was made to intubate the patient in the catheterisation lab. A bedside transthoracic echocardiogram showed reduced ejection fraction of 25% and apical to mid-ventricular segment ballooning, with only basal segments contracting. This was in keeping with TC.
A formal echocardiogram performed the next day confirmed the findings of the bedside echocardiogram (Figs.
Fig. 3
ECG in four-chamber view shows (a) normal ventricular cavity contour at end-diastole and (b) apical to mid-ventricular segment ballooning at end-systole.
In the past decade, several case reports have noted an association between myasthenic crisis and TC. A search on PubMed Central revealed at least seven cases in women and three cases in men. Notably, a 2015 Chinese publication reported a similar case in a patient with similar demographic characteristics.(1) However, this presentation of TC without overt chest pain or dyspnoea is unique among the other reported cases.
Myasthenic crisis is a complication that is known to occur in 10%–20% of patients with MG.(2) It is characterised by neuromuscular respiratory failure requiring the need for invasive airway management. Common precipitants include concurrent infections, recent surgery and immunosuppressive therapies, but it can also be part of active disease progression.(3) Based on our patient’s history, her throat tightness and swallowing difficulty were likely due to progressive bulbar weakness, with no obvious precipitant identified. Her complaint of orthopnoea preceding her presentation to the emergency department could suggest diaphragmatic weakness seen in impending myasthenic crisis; however, she was not dyspnoeic at presentation. Of note, typical signs of acute respiratory distress such as the use of accessory muscles may not be obvious in myasthenic crisis, as they may be masked by generalised weakness. A report reviewing 63 episodes of myasthenic crisis showed that they began with generalised weakness, bulbar symptoms and weakness of respiratory muscles in 76%, 19% and 5% of cases, respectively.(3) A systematic review assessing cardiac manifestations in MG reported that complications included TC, giant cell myocarditis and rhythm abnormalities.(4)
TC was first described in 1990 by Sato et al, who used ‘tako-tsubo’ to describe the ‘octopus pot’ appearance of the left ventricle on imaging studies, caused by apical dilation.(5) Pathognomonic findings include characteristic reversible left ventricular anteroapical dyskinesia without significant coronary artery disease. The Mayo Clinic’s diagnosis of TC includes: (a) transient left ventricular dysfunction; (b) absence of angiographic obstructive coronary artery disease or acute plaque rupture; (c) ECG abnormalities with ST elevations, or modest troponin elevation; and (d) absence of pheochromocytoma. TC occurs in 1%–2% of patients with troponin-positive STEMI, particularly in postmenopausal women.(6) The mechanism for TC has been postulated to be an excessive release of catecholamines, causing impaired cardiac function despite normal myocardial perfusion. It is said that events leading up to the myasthenic crisis bring about significant physiological stress, causing a catecholamine surge that precipitates TC.
In the aforementioned case, the patient’s clinical presentation to the emergency department was not a strong mimic of an AMI, as there was an absence of chest pain or overt dyspnoea. The patient’s history was also atypical of an AMI. Thus, the ECG finding of classical STEMI and the raised serum troponin levels were peculiar. A majority of TC presentations occur with severe retrosternal chest pain: a systematic review by the international Takotsubo registry in 2015 showed that the predominant symptom on admission was chest pain (75.9%), followed by dyspnoea (46.9%) and syncope (7.7%).(7) While TC is renowned to be a mimic of AMI, it is noteworthy that some patients may not present with the classical chest pain symptoms or with dyspnoea, as in the case of our patient. With the ubiquitous availability of portable ultrasonography in emergency departments, we can perhaps perform rapid and noninvasive consideration of TC early in the management of patients with a similar profile. However, we acknowledge the limitations of an acute setting, as the use of ultrasonography is operator dependent, and the need to reduce the door-to-balloon time is a time limitation.
As TC is usually a transient disorder, management primarily focuses on addressing the cause of the stressor as well as providing supportive therapy. Occasionally, TC can be complicated by cardiogenic shock requiring intensive therapy, as seen in 10% of patients.(7) In our case where myasthenic crisis was the stressor, management comprised a close assessment of respiratory function, rapid therapies and immunomodulators. For our patient, intravenous immunoglobulin, pyridostigmine and the immunomodulating therapies of prednisolone and azathioprine were started. She was subsequently extubated one day later and discharged well after 12 days.
To conclude, we would like to point out the need for clinicians to be vigilant to potential cardiac complications during myasthenic crisis. This awareness should prompt investigation with ultrasonography and ECG even in the absence of chest pain or dyspnoea.
Yours sincerely,


