Robin, your patient for 30 years, visited your clinic with his wife Mary. You sensed that he was hesitant about sharing something. Upon further probing, he opened with “It’s really nothing…” and went on to describe a soft buzzing sound in his ears at night that seemed to be worsening over the past few years. Mary added that he sometimes failed to respond to her when she spoke to him from another part of their flat. She also noticed that he had completely stopped listening to his favourite collections of classical music in the past year.
WHAT IS TINNITUS?
Tinnitus is a perception of ringing, buzzing or other noises in one or both ears in the absence of an external source.(1) For the purposes of management, it is useful to first categorise tinnitus into pulsatile and non-pulsatile types. Non-pulsatile tinnitus is more common and can take on various qualities such as buzzing, ringing, crackling, humming or a cicada-like sound.
The pathogenesis of non-pulsatile tinnitus remains speculative. Current hypotheses revolve around the concept of neural aberrancy in the cochlea, auditory nerve or along central auditory pathways. As tinnitus is frequently accompanied by hearing loss, the clinical approach to such tinnitus is similar to that for hearing loss. Other notable associated symptoms include dizziness, aural fullness, aural discharge and otalgia.
Pulsatile tinnitus, which is less frequently encountered, can be classified into pulse synchronous and non-pulse synchronous types. The former arises largely from vascular aetiologies, while the latter is associated with middle ear or palatal muscle myoclonus.
HOW RELEVANT IS THIS TO MY PRACTICE?
A 2016 systematic review found that the prevalence of tinnitus in the selected studies, using a common definition, ranged from 11.9% to 30.3% globally.(2) Large population studies found increased prevalence with increasing age, peaking between 60 and 69 years of age.(3,4) Males appear to be more affected than females.(3) Local data from Singapore is scant. A study on noise-exposed workers showed a prevalence of 23.3%.(4) It was also reported that the prevalence of hearing loss in Singapore military conscripts prior to enlistment was found to be 36.7 per 1,000.(5)
Effects of tinnitus on an individual’s well-being include insomnia, cognitive effects, anxiety and psychological distress.(6) A local study in 2010 showed that tinnitus patients who hear multiple sounds tend to have a poorer quality of life (QOL), as measured by the Tinnitus Handicap Inventory.(7) The reasons for the drop in QOL cited in this series were a lack of control over tinnitus, frustration and stress. Interestingly, middle-aged patients aged 40–50 years are most bothered by their tinnitus.(2) It is believed that although tinnitus is more common in older patients, having competing health issues reduces the relative burden of tinnitus on their QOL.
Tinnitus carries economic consequences as well. It can reduce productivity and, together with hearing loss, result in significant disability and loss of income.(8-10)
WHAT CAUSES TINNITUS?
The differential diagnoses of tinnitus are illustrated in
Fig. 1
Flowchart shows the approach to tinnitus. ENT: ear, nose and throat; H&N: head & neck; TM: tympanic membrane; TMJ: temporomandibular joint
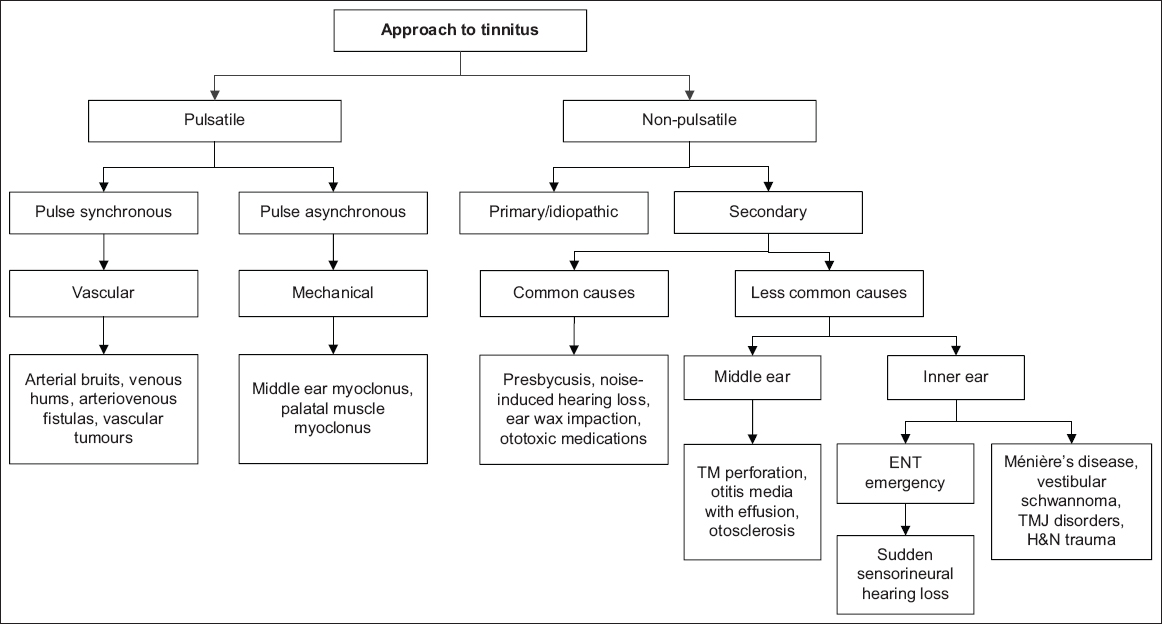
Non-pulsatile tinnitus
There are primary and secondary forms of non-pulsatile tinnitus. Primary tinnitus is idiopathic and may or may not be associated with sensorineural hearing loss (SNHL). Secondary tinnitus accompanies various external, middle and inner ear pathologies. Common differentials to consider include presbycusis, noise-induced hearing loss, ototoxic medications, ear wax impaction, middle ear pathologies, sudden sensorineural hearing loss, Ménière’s disease, vestibular schwannoma and other disorders.
Presbycusis
This is also known as age-related hearing loss and occurs in the elderly. It is believed to be caused by an accumulation of insults to the inner ear (e.g. noise, ototoxicity), on a background of genetic predisposition. Typically, the onset and progression of tinnitus and hearing loss are gradual, with high frequencies affected first.
Noise-induced hearing loss
Noise exposure is another major cause of SNHL and tinnitus. The tinnitus often precedes subjective hearing loss and serves as an early indicator of cochlear hair cell dysfunction.(11) Heavy equipment, environmental exposure or portable music devices that are played loudly for long periods of time are common sources of loud noises. Tinnitus from brief exposure, such as attending a loud concert, usually resolves. However, tinnitus from long-term or high-intensity exposure can be permanent. It is therefore important for physicians to actively seek these sources of exposure, as notification, workplace modification and appropriate protection can retard the progress of hearing loss.
Ototoxic medications
Several classes of drugs may cause or worsen tinnitus. Tinnitus may be the first symptom of ototoxicity and precede significant hearing loss and/or giddiness. The type of medication and dose prescribed determine the reversibility of ototoxicity and tinnitus. As such, eliciting a proper drug history and stopping the offending agent can save the patient from more severe ototoxicity. Such medications include antibiotics (e.g. aminoglycosides, vancomycin, macrolides), chemotherapeutic agents (e.g. cisplatin), diuretics (e.g. furosemide), aspirin and quinine.
Ear wax impaction
Patients with impacted ear wax that occludes the external auditory canal can present with tinnitus, conductive hearing loss and aural fullness. Symptoms usually resolve with clearance of the wax.
Middle ear pathologies
Middle ear pathologies such as tympanic membrane perforation, otitis media with effusion, and otosclerosis can also present with tinnitus. Most of these can be treated effectively with surgery. In the local context, adults should be screened for nasopharyngeal carcinoma when they present with otitis media with effusion.
Sudden sensorineural hearing loss
Sudden SNHL presents with a sudden drop in hearing that occurs within 72 hours. It is important to note that most patients complain of ear blockage rather than pure hearing loss, and thus it is important to think of this diagnosis when there is no obvious cause of ear blockage (e.g. ear wax, pus, debris). It is frequently associated with tinnitus in the affected ear. When there is accompanying vertigo, the syndrome is known as acute labyrinthitis. Most of these cases are idiopathic, with a small percentage due to vestibular schwannoma. These patients should be started on oral steroids early and referred to an otolaryngologist immediately to document their hearing loss and for possible specialised treatment such as intratympanic steroid injection.
Ménière’s disease
Ménière’s disease is a disorder of the inner ear characterised by recurrent episodic vestibular symptoms associated with SNHL, tinnitus and aural fullness.(12) There is a consistent temporal relationship between these symptoms, and each episode lasts 20 minutes to hours.
Vestibular schwannoma
Vestibular schwannoma is a benign tumour of the vestibular nerves. It is confined to the internal auditory canal and/or cerebellopontine angle. Compression of the adjacent cochlear nerve results in unilateral tinnitus and asymmetrical hearing loss. Dizziness is not as pronounced, as these tumours are slow-growing and allow for vestibular compensation. Older patients with vestibular schwannoma appear to suffer from more disabling tinnitus.(13)
Other disorders
Problems with the temporomandibular joint (TMJ) have been associated with tinnitus, but the exact mechanism is unknown. The tinnitus may improve when patients respond favourably to treatment for symptoms of TMJ dysfunction and craniocervical disease.(14) Blunt head and neck trauma can also affect peripheral and central auditory pathways. Such injuries can cause tinnitus and non-specific dizziness.
Pulsatile tinnitus
Pulse synchronous
Pulse synchronous pulsatile tinnitus is often vascular in aetiology. Some common differentials to consider are arterial bruits, intracranial vascular malformations, vascular tumours and venous hums.
Arterial bruits
Turbulent flow through atherosclerotic vessels in the neck, temporal bone and the cranium produces a bruit. Such patients complain of pulsatile tinnitus in one or both ears, but it is typically louder on the side of the pathology. They also usually have no other otologic complaints such as aural fullness or hearing loss, and their tinnitus is loudest in quiet environments.
Intracranial vascular malformations
Congenital arteriovenous malformations are rarely associated with tinnitus, while the acquired-type arteriovenous fistula from head trauma or surgery is more symptomatic, ipsilateral to the fistula. Large dural arteriovenous fistula can cause devastating intracranial haemorrhages, and early detection is important.
Vascular tumours
Tympanojugular glomus tumours are the most common tumours of the middle ear. They arise from paraganglia cells over the jugular bulb or promontory. An important cause of pulsatile tinnitus, they present as a pulsating red mass in the middle ear on otoscopy. Although benign, they are locally aggressive. Management involves watchful waiting, surgery or radiotherapy.
Venous hums
Venous hums might be heard in patients with idiopathic intracranial hypertension or those with anomalies in their intracranial venous systems, including abnormally high placement of the jugular bulb or diverticulum of the sigmoid sinus. It is often described by patients as a soft, low-pitched hum that stops with a change of head position or compression at the base of the neck.(15,16)
Non-pulse synchronous
Non-pulse synchronous pulsatile tinnitus is commonly due to neuromuscular disorders such as middle ear myoclonus and palatal myoclonus. Myoclonus of the muscles of the middle ear (tensor tympani and stapedius muscles) or palate can be idiopathic or secondary to neuromuscular disorders such as multiple sclerosis. Such myoclonus is usually diagnosed from history, as patients are frequently asymptomatic at the time of consultation.
WHAT CAN I DO IN MY PRACTICE?
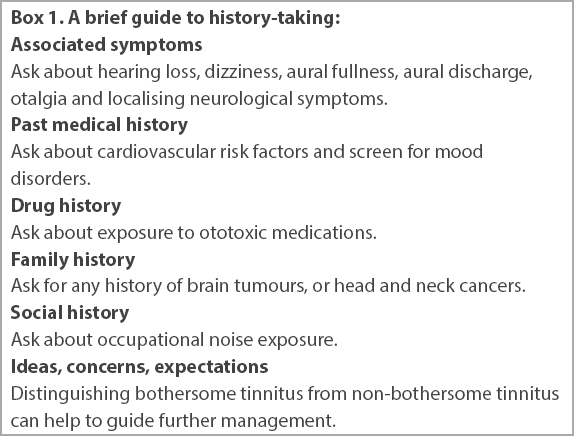
Physicians should determine the laterality, onset, temporal pattern and characteristics of the tinnitus by taking the history of the presenting complaint.
Box 1
A brief guide to history-taking:
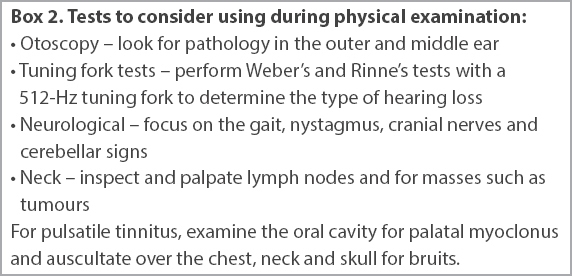
Box 2
Tests to consider using during physical examination:
Management
Initial management should be focused on resolving underlying causes. This includes ear syringing to clear ear wax, cessation of ototoxic medication and avoidance of exposure to loud noise. Patients should then be asked to maintain a healthy lifestyle with regular exercise and proper sleep, as cardiovascular health and stress levels can determine the severity of tinnitus. As most patients are most bothered by their tinnitus in quiet environments, they should be advised on the use of ambient noise from televisions, radios and tinnitus smartphone applications to ‘mask’ their tinnitus in such environments.
WHEN SHOULD I REFER TO A SPECIALIST?
Referral to an otolaryngologist should be considered in the following scenarios:
Any significant underlying cause is suspected from the clinical evaluation
All cases of unilateral tinnitus, especially if accompanied by hearing loss, dizziness and other neurological deficits, while sudden hearing loss should be referred urgently to an otolaryngologist
All pulsatile tinnitus
Any persistent (> 6 months) or bothersome tinnitus(1)
An audiogram and a tympanogram are the first-line investigations in specialist practice. Other investigations such as radiological imaging and flexible nasopharyngoscopy are only ordered if deemed necessary. Magnetic resonance imaging of the internal acoustic canal is performed when patients present with unilateral symptoms, especially if accompanied by asymmetrical SNHL on the audiogram.
Similarly, management is first directed at any underlying cause. Further management then aims to reduce the impact of tinnitus on QOL. Bothersome tinnitus can be managed through a formal rehabilitation programme and with hearing aids.(1) Tinnitus rehabilitation programmes involve a combination of education, counselling and sound therapy. This aims to reduce perception of the tinnitus and reduce its impact on the physical, social and mental well-being of patients. Hearing aids are an effective option for patients with both hearing loss and tinnitus. The perception of tinnitus is reduced, presumably through a reduction of neural aberrancy in peripheral and central auditory pathways.
The use of medications, such as antidepressants and anticonvulsants, and supplements (such as Ginkgo biloba, melatonin and zinc) has no proven efficacy and thus is not recommended in general.(1) However, antidepressants and anticonvulsants have roles in the management of concomitant mood disorders and specific types of tinnitus.
TAKE HOME MESSAGES
-
Tinnitus is a perception of sound in one or both ears in the absence of an external source, and has a prevalence of 11.9%–30.3% globally.
-
There are two types of tinnitus: pulsatile and non-pulsatile types, with the latter being more common.
-
Tinnitus can be accompanied by dizziness, aural fullness, aural discharge and otalgia.
-
Tinnitus may result in insomnia, cognitive effects, anxiety, psychological distress and lower QOL.
-
Common causes of non-pulsatile tinnitus include impacted ear wax, presbycusis, noise-induced hearing loss and ototoxicity.
-
Sudden SNHL presents with a sudden drop in hearing that occurs within 72 hours and frequently presents with tinnitus in the affected ear. This requires early medical assessment.
-
Initial management for tinnitus should focus on the identified underlying causes.
-
Most patients with tinnitus are bothered by it in quiet environments, and they can be advised to use ambient noise from televisions, radios and tinnitus smartphone applications to ‘mask’ their tinnitus.
-
A referral to an otolaryngologist is indicated if there are significant underlying causes suspected from the clinical evaluation, unilateral tinnitus, sudden hearing loss, pulsatile tinnitus, and any persistent or bothersome tinnitus.
You reviewed Robin three months later, after he had been fitted with a hearing aid. He thanked you for recommending him to get a hearing aid evaluation when he first visited you. It had helped him to enjoy his music once again, and he was also less disturbed by the buzzing sound now.
SMJ-61-452.pdf


