Abstract
INTRODUCTION
In volar wrist surgery, the traditional longitudinal incision leaves a scar that may be considered cosmetically unpleasant. Recent studies suggest that transverse wrist incisions result in more aesthetically pleasing scars that are well hidden in the wrist crease. The aim of our study was to explore the public’s perceptions of longitudinal versus transverse wrist scars.
METHODS
A prospective survey was conducted among the general public. Inclusion criteria were patients aged over 18 years with no prior surgery to the wrist. Survey questions assessed included: (a) longitudinal or transverse scar preference; (b) reasons for preference; and (c) demographic information.
RESULTS
There were 107 respondents from the general public. More respondents preferred longitudinal scars. Top three reasons for longitudinal scar preference were: (a) perceived damage to wrist structures by a transverse incision; (b) better cosmesis; and (c) scar from the transverse incision appearing like a self-inflicted injury. Top three reasons for transverse scar preference were: (a) easily concealed by accessories; (b) less noticeable; and (c) better cosmesis. Respondents aged 60 years and above were most concerned about possible damage to wrist structures; younger respondents were most concerned that transverse scars appeared like self-inflicted injuries.
CONCLUSION
Respondents from the general public preferred a longitudinal scar to a transverse one. Younger respondents were most concerned about how the transverse scar appeared like a self-inflicted injury while older respondents were most concerned with perceived functional implications of the incisions.
INTRODUCTION
Scar appearance after a surgical procedure is important to patients; a majority of patients undergoing surgery want smaller and less visible scars. This is an especially important consideration for hand surgery, as hands play a pivotal role in human interaction, communication and expression.(1) Surgical scars on the hand or wrist may attract attention and patients tend to be concerned about the appearance of their hands.(2) Also, patient satisfaction with scar outcome is found to correlate better with scar-related psychosocial distress, as compared to a clinician’s perception of scar severity.(3)
In recent years, there has been an increasing trend towards minimally invasive surgical techniques.(4) One example is the minimally invasive percutaneous plate osteosynthesis technique for distal radius fractures,(5,6) which uses a transverse wrist incision. The procedure was found to have similar functional outcomes as the traditional longitudinal approach. However, these studies excluded fractures that were open, multifragmentary, intra-articular, involved neurovascular compromise, had concomitant upper extremity injury or involved systemic multiorgan trauma.(6-8) For fractures that are amenable to fixation with a transverse approach, the main benefit is that it allows the scar to blend in with the wrist crease and is less noticeable, unlike the longitudinal scar from the traditional Henry approach.(7)
Endoscopic carpal tunnel release is performed using a transverse volar wrist crease incision, with varying degrees of patient satisfaction based both on appearance of the scar as well as postoperative pain when compared to the longitudinal open carpal tunnel approach.(9) Ganglion excision at the wrist and tendon harvesting may also be done using transverse incisions. On the other hand, the longitudinal incision is advocated over the transverse incision for De Quervain’s disease because of fewer complications, including fewer hypertrophic scars.(10,11)
However, wrist scar appearances are open to different interpretation by patients and there are likely to be unexplored reasons why patients would not prefer the transverse wrist scar. It is important to explore such concerns, as the patients’ first impression of the scar could influence their or the surgeons’ decision between a transverse and longitudinal approach if the surgery could be done safely by both approaches.
To explore the first impressions of wrist scars, our study aimed to determine which wrist scar orientation was more desirable to the community, what their reasons were for choosing each option and how demographics might influence choices.
METHODS
The survey was conducted through face-to-face interviews using a fixed interview questionnaire. Institutional ethics review board approval was obtained for the study.
Study respondents were aged over 18 years, and had no previous surgery to the wrist or no current indication for wrist surgery. Respondents were asked to base their responses on the idea of having a scar on their wrist, rather than rating an actual scar. Respondents were selected via convenience sampling.
The questions and options included in the survey for the general public are shown in the Appendix. Our study survey was conducted in English or Mandarin, depending on the respondent’s fluency. The survey was designed to determine: (a) the proportion of respondents who preferred the transverse scar when compared to the longitudinal scar; (b) reasons for their preference; and (c) the correlation of this preference to demographics. Respondents from the general public were patients from the orthopaedic surgery clinic on follow-up for an unrelated problem. In the first part of the survey, respondents were asked to state if a transverse or longitudinal wrist scar was preferred. Information regarding the procedural risk of each approach was not mentioned because the choice was to be based on first impressions rather than consideration of functional outcomes. The respondents also each provided a reason, which was recorded ad verbum, that would be analysed qualitatively. Similar reasons were subsequently recategorised under various headings. For example, those who mentioned ‘the longitudinal scar follows the axis of the arm and therefore looks better’ and ‘the longitudinal scar looks nicer in my opinion’ would be reclassified under the reasoning ‘better cosmesis’. Lastly, demographic data was gathered, including age, gender and ethnicity of respondents.
The median and one-sample chi-square tests were used to analyse the respondents’ scar preferences. Their reasons for the preferences were collected and categorised.
RESULTS
107 respondents from the community fit our inclusion criteria. Median age of the cohort was 55 ± 16 years. Among the respondents, 42% were male and 58% were female. In terms of ethnicity, 78% of respondents were Chinese, 13% were Malay and 9% were Indian (
Table I
Demographics of general public respondents (n = 107).
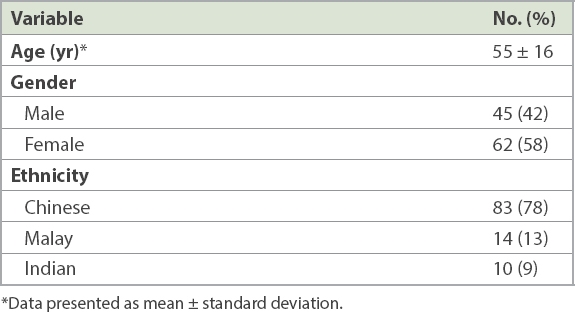
Fig. 1
Chart shows reasons given by the general public for their preference of incision orientation.
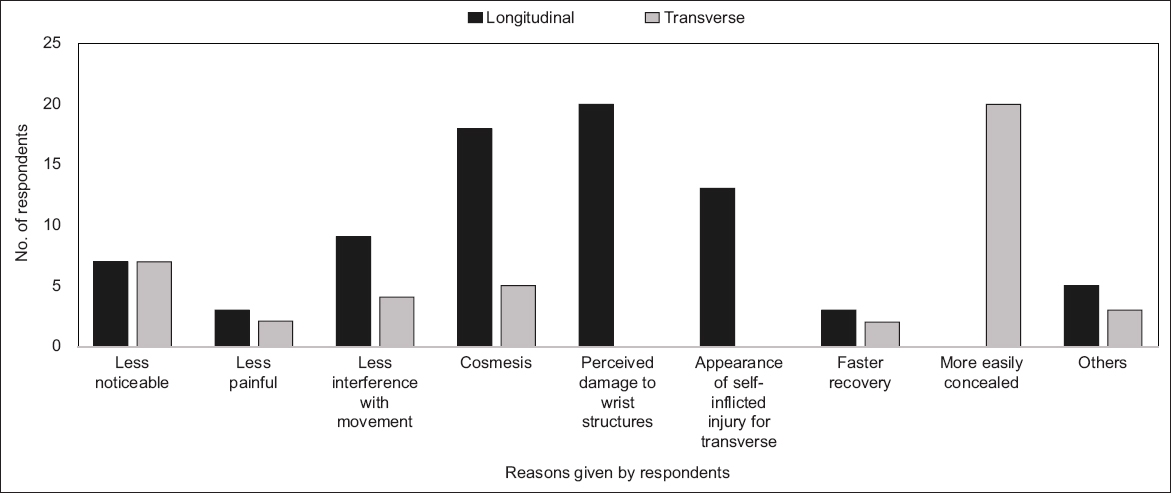
The main reasons given for the preference for longitudinal scars included: (a) perception that transverse incisions would cause damage to wrist structures, such as veins and tendons (24.4%); (b) better cosmesis (23.1%); and (c) the scar from a transverse incision mimicking a self-inflicted injury (16.6%).
The top reason given for the choice of transverse scar was that it would be more easily concealed by wrist accessories, such as watches (46.5%). Other reasons were that the transverse scar was less noticeable (16.3%) and had better cosmesis (11.6%).
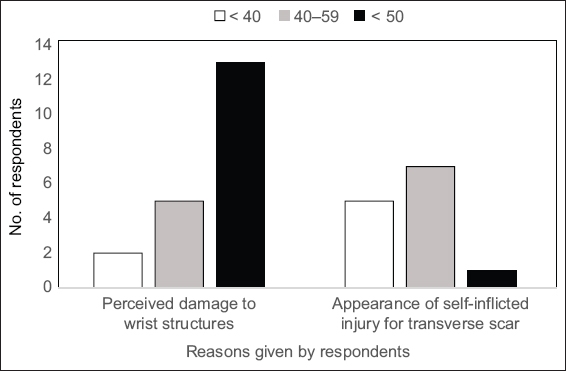
Among respondents aged 60 years and above, perceived wrist damage was the main reason for choosing the longitudinal scar; for those who were younger, avoiding the appearance of a self-inflicted injury was the top reason (
Fig. 2
Chart shows preference for longitudinal incisions with respect to respondent age groups (years).
DISCUSSION
Contrary to our expectations, more of the general public preferred a longitudinal scar (63%, p = 0.00905), with nearly a quarter of respondents citing better cosmesis as a reason for the preference. Many who chose the longitudinal scar also believed that a transverse incision might damage tendons, veins and arteries in the wrist, suggesting that patients may have preconceived notions of how incisions would affect function following surgery. These findings also suggest that it might be appropriate to address such concerns prior to surgery.
We also underestimated the significance of social stigma that would be associated with a transverse wrist scar; surgeons may similarly overlook this aspect. We suggest addressing and alleviating these concerns of patients during preoperative counselling by showing them photographs of healed surgical scars. Although transverse scars may not be preferred by the majority, transverse incisions hold merit for patients who would seek to hide the scar using wristwatches or other accessories.
Older respondents were more concerned about perceived wrist damage by the transverse incision, while younger respondents were more concerned about the social stigma associated with the scar. This influences how we target preoperative counselling for patients of different age groups, with increased focus on functional aspects of the incision or surgery with older patients and cosmesis for younger patients, thereby enabling them to make a more informed decision on the approach to choose and improve concordance between the different age groups.
Prior to the survey, we expected that most participants would be able to choose a preferred incision scar based on aesthetics. However, even after being probed on aesthetic considerations, most (81%) respondents were inclined to consider the functional outcomes of each incision type rather than focus on scar appearance. We are aware that in volar wrist surgeries, incision aesthetics should not be the sole consideration but must be considered in tandem with the surgeon’s familiarity with the surgical procedure and professional opinion as to the suitability of the incision for the surgery.
Minimally invasive surgery is a growing trend. A recent study by Naito et al explored the possibility of distal radius fixations with a mere 10-mm incision for a volar locking plate.(12) Most surgeons are more familiar with the traditional longitudinal approach, and our results showed that patients were not averse to such incisions. However, perceptions of scar aesthetics vary with individual choice and show marked interpersonal variability, as seen from our survey of first impressions of volar wrist scars. Therefore, should the surgeon have the expertise in both approaches and the surgery be amenable to either approach, the orientation of the surgical scar could be discussed preoperatively with the patient before a decision on the surgical approach is taken.
SUPPLEMENTARY MATERIAL
SMJ-61-548-Appendix.pdfACKNOWLEDGEMENTS
We would like to acknowledge the valuable feedback and input received from the surgeons at Hand and Microsurgery Section, Department of Orthopaedic Surgery, Tan Tock Seng Hospital, Singapore, while conducting this study.


