Abstract
Tuberculosis (TB) is a major health issue in the Philippines. TB-Care was introduced in 2011 to tackle pulmonary TB among the urban poor in Payatas, Quezon City, Philippines. We evaluated the efficacy of TB-Care in increasing treatment success and compliance rates. This retrospective case series reviewed 44 patients with pulmonary TB enrolled in TB-Care from 2013 to 2014. Diagnosis and treatment of pulmonary TB was made in accordance with World Health Organization guidelines. Treatment outcomes included cure, completed treatment, successfully treated, failed treatment and transferred to another facility. 14 (73.7%) out of 19 patients tested were bacteriologically cured. The average 100% compliance rate was 90.8% over six months. The programme successfully treated 39 (88.6%) patients. This was comparable to the overall national treatment success rate of 90% for Philippines and 79% for Singapore, with higher compliance rates than were previously reported in this community.
THE PROJECT
Tuberculosis (TB) is a major health issue in the Philippines. In 2010, it was the sixth leading cause of death, accounting for 5.1% of total deaths in the country.(1) The prevalence of TB among the urban poor in the Metro Manila area is twice that of the prevalence among the general population.(1) A significant population of the urban poor live in Payatas, Quezon City, the Philippines, where one of the largest waste disposal facilities in Manila is located.
The TB-Care programme was introduced in 2011 by a group of medical students from Yong Loo Lin School of Medicine, National University of Singapore, Singapore. It was organised in partnership with Acts29, a non-governmental organisation, to tackle the challenges of treating TB among the urban poor in the Philippines. TB-Care aims to provide services that complement the National Tuberculosis Control Programme (NTP) in the Philippines. The NTP provides services and guidelines for the diagnosis and treatment of TB, with directly observed therapy (DOT) as its primary strategy. The programme targets a case detection rate of 85%, cure rate of 85% and treatment success rate of 90%.(2)
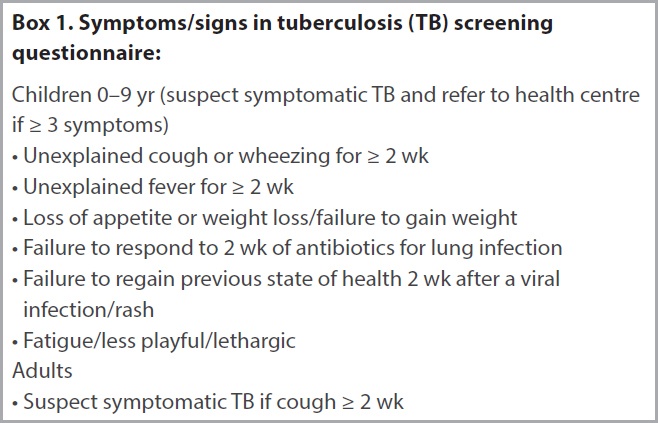
We evaluated the efficacy of TB-Care in increasing treatment success and medication compliance rates among patients with pulmonary TB in Payatas, Quezon City, Philippines. This retrospective case series reviewed all patients with pulmonary TB enrolled in TB-Care from 2013 to 2014. Patients were screened via administration of a questionnaire for TB symptoms (
Box 1
Symptoms/signs in tuberculosis (TB) screening questionnaire
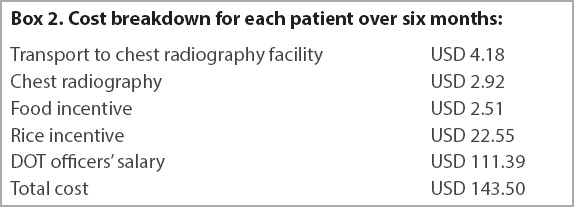
Two locals from Payatas were employed as DOT officers for the TB-Care programme. Both worked as waste pickers previously and were pulmonary TB patients who had been successfully treated with DOT. Once diagnosed with pulmonary TB, patients would undergo a counselling session with the DOT officers, and were given pamphlets and educated on TB and treatment. Patients were started on a treatment regimen prescribed by the clinician. Medications were administered in front of the DOT officers. When a patient missed two doses of medications or an appointment, the DOT officers would conduct a house visit to investigate the reason for non-compliance and counsel the patients on the importance of compliance. Patients were required to attend weekly lectures. During follow-up appointments, food (e.g. biscuits and rice) was distributed to the patients as an incentive to compensate for their loss of income from time off work. Costs of consultation, investigations and transport were borne by the TB-Care programme (
Box 2
Cost breakdown for each patient over six months
OUTCOMES
A total of 45 patients were enrolled from 2013 to 2014. One patient was excluded from the study as a large proportion of data was missing from his medical records. Among the 44 remaining patients, 40 (90.9%) patients were newly diagnosed and 4 (9.1%) were relapse cases. Owing to the limited resources available, we did not have data on comorbidities such as human immunodeficiency virus infection or diabetes mellitus. There were also no resources for TB drug susceptibility testing. There were 42 (95.5%) adults and 2 (4.5%) paediatric patients. 32 (72.7%) of the patients were male and 12 (27.3%) female, giving a male-to-female ratio of 2.7:1. 14 (73.7%) out of 19 patients tested were bacteriologically cured. Excluding those who were cured, 25 (83.3%) of the 30 remaining patients completed treatment, with an overall treatment success rate of 88.6%. None failed treatment, while 2 (4.5%) out of 44 patients transferred to another facility; 3 (6.8%) out of 44 patients died (
Fig. 1
Flowchart shows treatment outcomes for the patients.
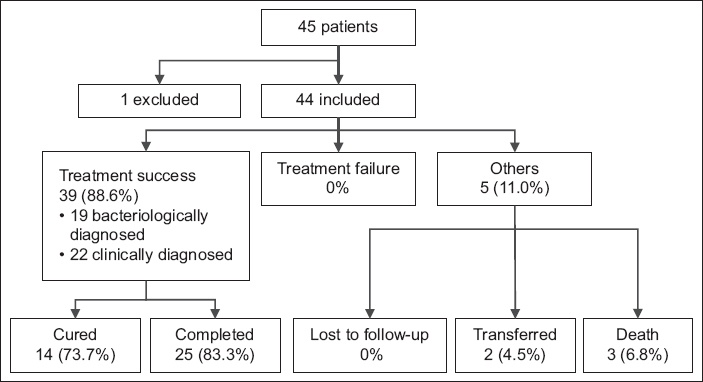
Fig. 2
Graph shows the compliance rates of patients in TB-Care programme.
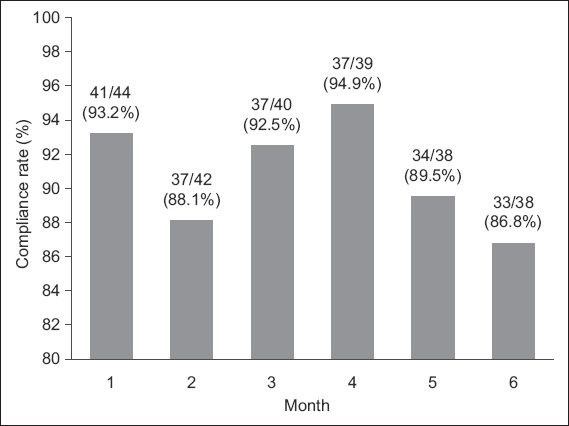
88.6% of our study population were successfully treated for TB. This is comparable to the overall national treatment success rate in 2013 of 90% for Philippines and 77% for Singapore.(4) It should be noted that the 90% stated in the NTP surveillance report reflects the status of the whole country and does not take into account differences in the poorer regions. Within Quezon City, the cure rate is 67.4%–71.9%,(5) which is comparable to the 73.7% cure rate for the present study. In our study, the average compliance rate was 90.8% over six months. This exceeds the compliance rate of 70%–72% in Quezon City.(5) In comparison to other independent TB DOT programmes in rural communities, our treatment success rate of 88.6% was comparable to those in Nigeria,(6) Thailand(7) and Tanzania,(8) which were 85.45%, 75.5% and 66.5%, and even to developed countries such as Singapore(9) with a success rate of 79%.(4)
The NTP has been successful in making DOT accessible to the general population, achieving treatment success rates of 90%.(4) However, due to poverty, the people in Payatas face unique challenges that affect compliance, including hidden costs such as income lost during follow-up appointments when patients are not able to work. Additionally, NTP does not cover the cost of the chest radiography. TB-Care may be able to minimise these challenges, as it provides financial aid for chest radiography and transportation. Food given out during follow-up appointments would make up for the loss of income from time off work. The monthly rice incentive, in addition to providing motivation for compliance, provides nutritional supplementation for the patients.
These initiatives were developed after extensive consultation with the local non-governmental organisation and locals in the community. Patient performance-based incentive schemes have been shown to work in both developed and developing countries.(10) In Singapore, a ‘DOT and Shop‘ scheme demonstrated that providing grocery vouchers to low-income patients as an incentive improved treatment completion rates.(11) Our DOT officers, being previous TB patients who had experienced DOT themselves, had more credibility and rapport among the community.
CONCLUSION
Implementing DOT in an urban poor community is challenging. TB-Care achieved a treatment success rate of 88.6%, which is comparable to national treatment programmes in other Southeast Asian countries. TB-Care achieved a significantly higher compliance rate than in previous reports.(4) This pilot programme by Singaporeans in partnership with Filipinos shows promising results using simple and cost-effective methods and patient empowerment. It addresses hidden costs and provides socioemotional support to patients and could be considered in other low-resource settings.


