Abstract
INTRODUCTION
Accurate staging of patients with pancreatic cancer is important to avoid unnecessary operations. The aim of this study was to prospectively assess the impact of magnetic resonance (MR) imaging on preoperative staging of liver in patients with findings of resectable pancreatic cancer on computed tomography (CT).
METHODS
All patients who presented to a tertiary referral centre with pancreatic cancer between April 2012 and December 2013 were included in the study. Patients with findings of resectable disease on CT underwent further liver diffusion-weighted MR imaging, using a hepatocyte-specific contrast agent.
RESULTS
A total of 583 patients with pancreatic cancer were referred. 69 (11.8%) had resectable disease on CT. Of these 69 patients, 16 (23.2%) had liver metastases on MR imaging, while 6 (8.7%) had indeterminate lesions. Of the 16 patients with positive MR imaging findings of liver metastases, 11 died of pancreatic cancer, with a mean survival time of nine months (95% confidence interval [CI] 5.22–14.05). The mean survival time of the 47 patients with negative MR imaging findings was 16 months (95% CI 14.33–18.10; p = 0.001). Subsequently, 22 of these patients underwent surgery, and only 1 (4.5%) patient was found to have liver metastasis at surgery.
CONCLUSION
The results of the present study indicate that MR imaging improves the staging of disease in patients with resectable pancreatic cancer.
INTRODUCTION
Pancreatic cancer has an incidence rate of 13.6 per 100,000 in the United Kingdom.(1) Most patients with pancreatic cancer have advanced disease at the time of diagnosis, and their overall five-year survival rate is less than 5%, although this rate is estimated to rise to 10%–20% after curative surgery.(2-7) Curative and palliative operations are associated with an average inpatient stay of two weeks, a mortality rate of up to 5% and morbidity rates of 20%–50%.(8-10) Patient recovery is often slow and accompanied by further intervention. As a result, hospital and societal costs are high. Therefore, accurate patient staging is critical in order to avoid unnecessary operations.
Magnetic resonance (MR) imaging, when used with a hepatocyte-specific contrast agent, has increased sensitivity and specificity compared to computed tomography (CT).(11) Therefore, MR imaging is now routinely used for disease staging in patients with colorectal or other operable liver diseases who are suitable for liver resection. The reported sensitivity of MR imaging in detecting liver metastasis is 81%–92%, compared to 70%–87% for multidetector CT (MDCT).(12,13) No guideline exists on separate and specific staging of the liver in the setting of pancreatic cancer, although international guidelines recommend staging using contrast-enhanced MDCT while reserving MR imaging for indeterminate liver lesions encountered on CT.(14,15) The aim of this study was to prospectively assess the impact of liver MR imaging on the preoperative staging of patients with findings of resectable pancreatic cancer on CT.
METHODS
All patients referred to a regional centre for evaluation and treatment of suspected pancreatic cancer between April 2012 and December 2013 were included in this study. Investigations performed included CT (performed in the portal venous phase, 64-slice MDCT) of the chest, abdomen and pelvis, and endoscopic ultrasonography (EUS) with fine-needle aspiration biopsy of the pancreatic mass and suspicious adjacent lymph nodes.
The imaging, pathologic and clinical findings were discussed at weekly multidisciplinary meetings attended by consultant surgeons, radiologists, pathologists and oncologists with a special interest in pancreatic cancer. Patients with pathologically confirmed pancreatic cancer deemed resectable on CT and EUS proceeded to MR imaging of the liver prior to surgery or neoadjuvant chemotherapy. The decision on resectability was based on established criteria (American Hepato-Pancreato-Biliary Association/Society of Surgical Oncology/Society for Surgery of the Alimentary Tract).(16,17) Institutional Review Board approval was sought but not deemed necessary, as we were already routinely using MR imaging to stage patients with metastatic colorectal cancer who were being assessed for liver resection in our department. As part of the staging process, all patients undergoing operation for resectable pancreatic cancer had undergone prior laparoscopy to exclude peritoneal metastasis.
Patients were examined using a Magnatom® Avanto 1.5-T superconducting MR system (Siemens Healthcare Global, Erlangen, Germany) with a body matrix coil. The protocol included a T1-weighted dual fast gradient-recalled echo sequence, T2-weighted fast spin-echo (FSE) sequence with spectral fat suppression, two diffusion-weighted (DW) single shot echo-planar sequences and a transverse breath-hold spoiled gradient-recalled echo (dynamic gadolinium-enhanced) sequence, before and after dynamic injection of either gadoxetate disodium (Primovist™, Bayer, Germany) 0.1 mL/kg body weight or gadobenate dimeglumine (Multihance®, Bracco, Princeton, NJ, USA) 0.2 mL/kg body weight. Hepatic arterial dominant, portal venous, equilibrium and hepatobiliary phase sequences were performed. A 1-mL test bolus of contrast material was used to determine the time to peak arterial enhancement of the hepatic arterial phase. The portal venous and equilibrium phases were performed at 70 and 180 seconds after contrast administration. The hepatobiliary phase was performed at 20 minutes (gadoxetate disodium) or 60 minutes (gadobenate dimeglumine) after contrast administration, depending on the contrast material used.
All images were evaluated using the Picture Archiving and Communication System version 10.1 (Carestream Health, Rochester, NY, USA). Reporting radiologists were institution-attending physicians with an interest in abdominal radiology and experience in MR imaging of the liver.
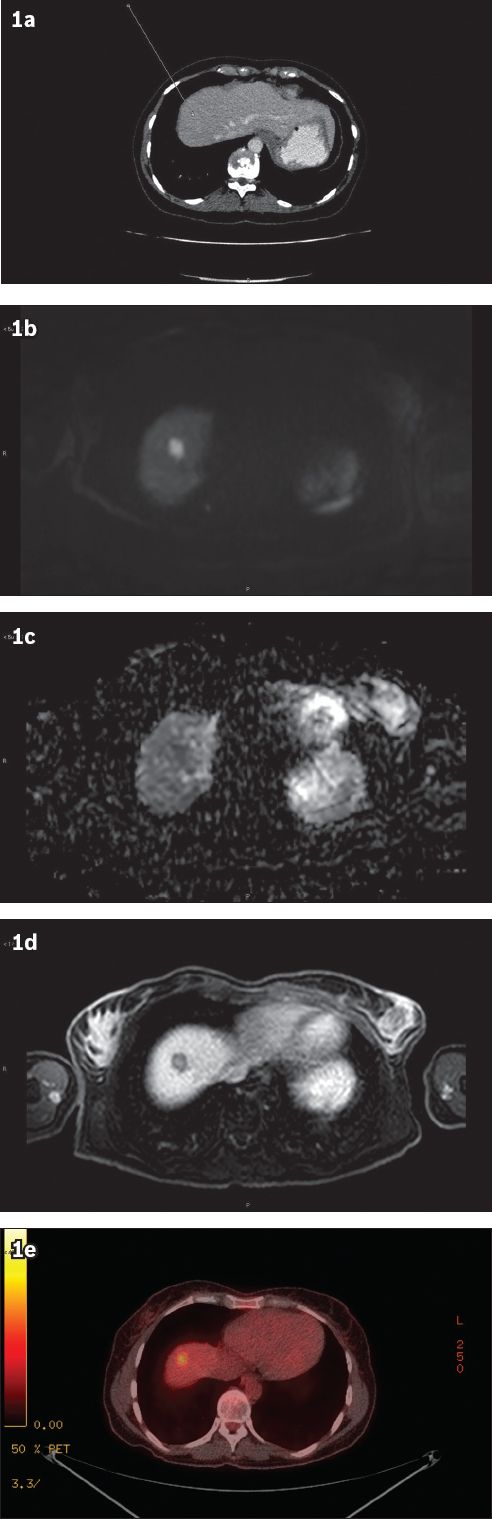
A lesion was considered metastatic if it was: (a) mildly to moderately hyperintense at a b-value of 20 sec/mm2 and remained hyperintense at a b-value of 800 sec/mm2; (b) moderately or strongly hyperintense (but less than the signal of fluid) to the surrounding liver parenchyma on T2-weighted FSE imaging; (c) found to demonstrate peripheral enhancement on dynamic gadolinium-enhanced T1-weighted imaging; and (d) hypointense to the surrounding liver parenchyma on excretory/hepatobiliary phase T1-weighted sequences. Imaging results are shown in
Fig. 1
(a) CT image typically shows the absence of liver metastasis. (b) Diffusion-weighted MR image; (c) apparent diffusion coefficient map; and (d) hepatobiliary phase MR image using a hepatocyte-specific contrast agent show the presence of liver metastasis in the same patient. (e) PET-CT image shows liver metastasis that demonstrates avid fluorodeoxyglucose uptake.
A lesion was considered benign if it fulfilled the classic features of a cyst, haemangioma or focal nodular hyperplasia on T2-weighted FSE, DW imaging (DWI) and dynamic gadolinium-enhanced T1-weighted imaging. Any lesion that did not correspond to the above criteria was considered indeterminate.(18) All images were reviewed by one of two experienced consultant radiologists with special interest in gastrointestinal and pancreatic imaging. Duration of survival was expressed as a mean or median with interquartile range (IQR) or 95% confidence interval (CI). The estimated survival time was calculated using the Kaplan-Meier estimator. Comparison between groups with positive and negative MR imaging findings was made using log-rank (Mantel-Cox) test. All statistical analyses were performed using PASW Statistics version 18.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
Between April 2012 and December 2013, 583 patients were referred for further management of probable pancreatic cancer. 69 (11.8%) patients (45 men, 24 women) were diagnosed with resectable pancreatic cancer on CT. Their median age was 64 (range 31–79) years. A flowchart illustrating how patients were diagnosed is shown in
Fig. 2
Flowchart shows how patients were diagnosed.
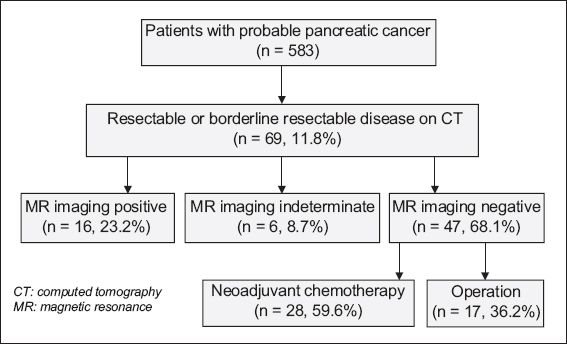
Three of the six patients with indeterminate lesions showed progression in keeping with metastatic deposits on interval MR imaging; one of these three patients died of disease. Of the remaining three patients who did not show disease progression on MR imaging, one patient underwent laparoscopic wedge resection of the 4-mm indeterminate liver lesion, which confirmed pancreatic metastasis, while two patients underwent pancreaticoduodenectomy, which revealed no obvious liver disease on surgery.
Of the 47 patients who had no evidence of liver metastasis on MR imaging, 17 were found to have resectable disease on imaging and underwent surgery with curative intent. Another 28 patients who had resectable disease with potential for positive margin underwent neoadjuvant chemotherapy; five of these patients had proceeded to surgery to date. The remaining two patients were deemed unfit for operation or chemotherapy. Out of the 22 planned pancreaticoduodenectomies, 1 (4.5%) was converted to palliative bypass due to the presence of a small (5 mm) subcapsular metastatic deposit in segment II of the liver, not demonstrated on MR imaging. None of the patients died postoperatively and 9 (40.9%) underwent R1 resection.
At follow-up, there were six postoperative recurrences. The patterns of recurrence were as follows: local (n = 2); pulmonary (n = 2); peritoneal (n = 1); and liver (n = 1). Time to recurrence was 3–13 (median nine) months. The patient with recurrence of liver metastasis (three months after surgery) had normal MR imaging at diagnosis and underwent six months of neoadjuvant chemotherapy, but did not have repeat MR imaging performed preoperatively.
Four of the 28 patients who received neoadjuvant chemotherapy demonstrated disease progression; two patients developed liver metastases at six and seven months, one had local disease progression and another died of chemotherapy-associated toxicity. Mean survival time for patients who were positive for liver metastases on MR imaging was nine months (95% CI 5.22–14.05) as compared to 16 months (95% CI 14.33–18.10) for those who were negative on MR imaging (p = 0.001,
Table I
Mean and median survival times in patients tested for liver metastasis on magnetic resonance imaging.
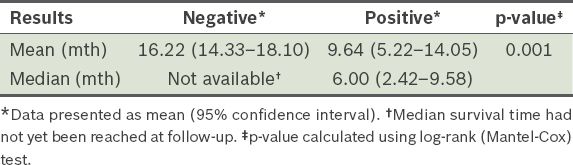
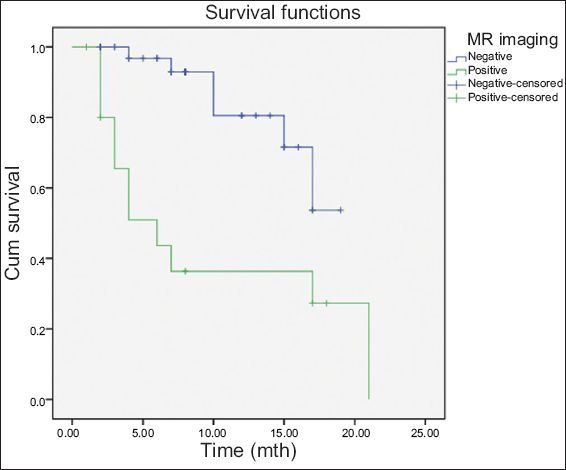
Fig. 3
Graph shows Kaplan-Meier survival curve of patients with negative and positive results for metastases on liver magnetic resonance (MR) imaging.
DISCUSSION
This prospective study showed that up to a quarter of patients with resectable pancreatic cancer on CT were positive for liver metastasis on MR imaging. The impact of this study was its potential to prevent unnecessary operations in these patients, thereby avoiding the associated morbidity and mortality. Of the patients who had an attempted curative resection, only 1 (4.5%) was found to be unresectable due to liver metastases on surgery.
Surgery offers the only chance of a cure for patients with pancreatic cancer. Margin-negative resection, tumour size and lymph node status have been accepted as significant determinants of postoperative survival following surgery.(2) Nevertheless, it is generally considered inappropriate to offer surgery to patients with metastatic disease at the outset. However, the role of neoadjuvant chemotherapy/radiotherapy is currently being evaluated, in an effort to downstage disease and achieve a better oncological outcome than previously demonstrated for oesophageal and rectal cancers.(19)
The role of cross-sectional imaging, mainly CT, is primarily to detect pancreatic cancer and, more importantly, identify the presence of distant metastasis. While aggressive pancreatic cancer may metastasise to the peritoneal cavity, lungs, pleura, and bone and adrenal glands, the most common site of metastasis is the liver.(20) Staging of pancreatic tumour size, local vascular involvement and lymph node metastasis is better evaluated on endoscopic ultrasonography with fine-needle aspiration biopsy than CT or MR imaging.(21) However, there is mounting evidence in the literature of the superior sensitivity of MR imaging in detecting and characterising liver lesions compared with CT, particularly when combined with the use of a specific hepatobiliary contrast agent and DWI.(22) While most of the data relates to colorectal cancer liver metastasis, MR imaging has been shown to be equally useful with other malignancies.(18)
This study supports the findings from previous studies that suggested increased detection of liver metastases in patients with pancreatic cancer on MR imaging.(23,24) Holzapfel et al reported a sensitivity of 53.3% on MDCT and 86.7% on DWI in detecting liver metastasis, with a specificity of 80.9% and 93.2%, respectively.(23) They also found that MR imaging of the liver would have changed the therapeutic management for 4 (12.9%) of the 31 patients in their study when compared to MDCT.(23) Motosugi et al reported the superior sensitivity of gadoxetic acid-enhanced MR imaging (92%–94%) compared to CT (74%–76%) in detecting liver metastasis in 54 patients with pancreatic cancer.(24) Although we did not perform liver MR imaging on all referred patients diagnosed with pancreatic cancer, in this select group of patients with resectable disease on CT, MR imaging has a sensitivity of 76.2% and specificity of 95.8%, with a positive and negative predictive value of 88.9% (95% CI 67.2–95.9) and 90.2% (95% CI 79.0–95.4), respectively.
The cost to health services and society when performing unnecessary operations needs to be considered. In a recent comprehensive study, Ljungman et al(25) looked at the cost utility of curative surgical treatment for pancreatic carcinoma; the average treatment cost of curative resection for pancreatic carcinoma was reported to be EUR 39,145 and the estimated cost per quality-adjusted life-year was around EUR 34,636. While similar local figures are not available, the overall cost for a palliative procedure, operating room time and hospital stay is likely to be similar. Most surgeons set aside operation time for curative pancreaticoduodenectomy despite the fact that 30%–40% of such procedures are palliative. Considering that the cost of additional MR imaging (about EUR 210) is a fraction of the cost of an operation, this puts in perspective the benefit of staging patients with pancreatic cancer using MR imaging before surgery.(26,27)
Despite advances in knowledge of pancreatic cancer over the last decades, its outcome remains poor. Unlike the majority of cancers, the relative survival rate of pancreatic cancer has improved very little since the early 1970s.(28) It remains unclear whether the most important prognostic determinant is a biologically aggressive tumour or early tumour progression that continues unrecognised beyond limited-stage disease (metastatic phenotype). More recent considerations have implied that future efforts should be focused on procedures that effectively predict resectability and outcome. A multicentre study on prospective diagnostic accuracy and clinical value of PET/CT in suspected pancreatic malignancy (PET Panc study) has completed its recruitment, and the results are awaited.(29)
One of the limitations of the present study is the lack of pathological confirmation of liver metastasis in patients with negative CT and positive MR imaging findings. However, a diagnosis of liver metastasis on MR imaging is an established imaging criteria, coupled with subsequent follow-up imaging to confirm disease progression. Furthermore, the survival time of patients with findings of liver metastases on MR imaging was also significantly reduced compared to those who had normal MR imaging findings; this is again consistent with our findings. Another potential criticism of this study is the delay to operation caused by additional imaging. Nonetheless, according to surgical and oncological colleagues, the median time of two weeks between CT and MR imaging is an acceptable interval for increased diagnostic certainty. Some critics may also consider the lack of multiphase CT to be a potentially confounding factor. This is not so, as the incidence of hypervascular liver metastases from pancreatic cancer is rare and published guidelines support portal venous phase CT for the detection of liver metastases.(14,15)
In conclusion, the present study has demonstrated that liver MR imaging with DWI using hepatocyte-specific contrast upstages patients who have findings of resectable pancreatic cancer on CT and adds valuable information to the diagnostic process, thus allowing clinicians to determine the most appropriate treatment for patients. Nevertheless, the findings of this study need to be confirmed by multicentre assessments and comparisons with other staging modalities such as PET/CT.


