Dear Sir,
Edwardsiella tarda (E. tarda), a member of the family Enterobacteriaceae, is a prominent tropical (and subtropical) aquatic pathogen. Pathogenic cases of E. tarda infection in humans are not well-defined and, to the best of our knowledge, there is no published literature on the duration of its survival inside humans. We herein report an unusual case of E. tarda-associated chronic osteomyelitis (OM) in an elderly Chinese man in Singapore who had worked as a fisherman in Indonesian seas for 15 years and later as a fishmonger in a local wet market.
The patient, a retiree who was 79 years of age, presented to us with two chronic discharging sinuses on his right medial knee surface. Further history taking revealed that he had longstanding left knee pain and swelling, with more marked pain, swelling and redness over the past six months. This had prompted his online purchase of a silicone cupping device, a form of traditional Chinese medicine, which he had applied religiously for 30 minutes a day over the affected area. The skin was initially intact, but two months ago, skin breakdown occurred and the discharging sinuses eventually appeared, with intermittent pus discharge. The patient had then consulted a general practitioner. However, the wound did not improve despite regular wound dressing and oral co-amoxiclav for the past two weeks. He thus decided to seek treatment at our tertiary hospital.
The patient was otherwise well and had experienced no constitutional symptoms or significant weight loss over the past six months, and no fever, chills, rigours or night sweats throughout. His past medical history was significant for atrial fibrillation on apixaban 2.5 mg twice daily, peripheral vascular disease, and dual-vessel disease status post percutaneous coronary intervention one year ago. He had no diabetes mellitus, hypertension or hyperlipidaemia. He did not consume any raw fish or foods, did not keep any pets, had no exposure to brackish waters, did not swim and had not travelled outside of Singapore in recent years.
On physical examination, two sinuses were visualised on the right medial knee surface (
Fig. 1
Photograph shows the appearance of the patient’s wound at presentation, with two sinuses visualised.

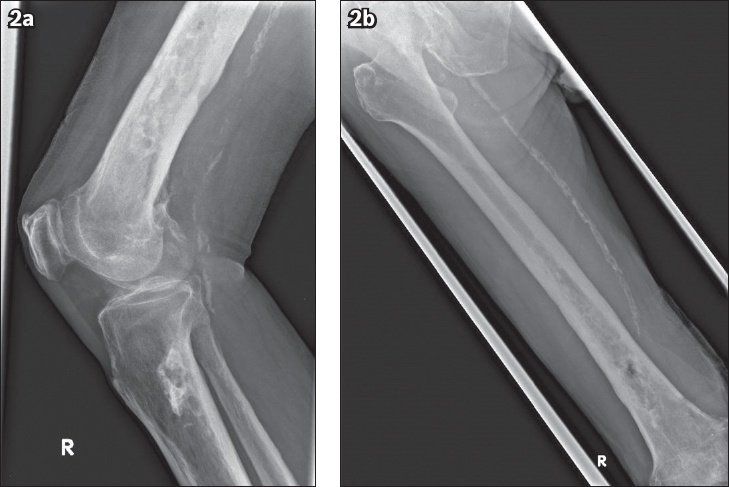
Laboratory studies revealed normochromic, normocytic anaemia with a haemoglobin level of 10.6 g/dL. Total white blood cell count was not raised at 8.00 × 109 cells/L. C-reactive protein was elevated at 29.6 mg/L, erythrocyte sedimentation rate was 107 mm/hour, and two sets of peripheral aerobic and anaerobic blood cultures showed no bacterial growth after 72 hours. The patient’s renal panel and electrolytes (calcium, magnesium and phosphate) were within normal limits. The chest was clear on plain radiographs. Radiographs of the right femur, tibia and fibula (
Fig. 2
Plain radiographs show the right (a) knee joint and (b) femur.
A heterogeneous marrow signal was revealed on T1- and T2-weighted MR imaging (
Fig. 3
MR image of the right thigh shows findings consistent with chronic osteomyelitis of the right femur, including multiple cloacae.
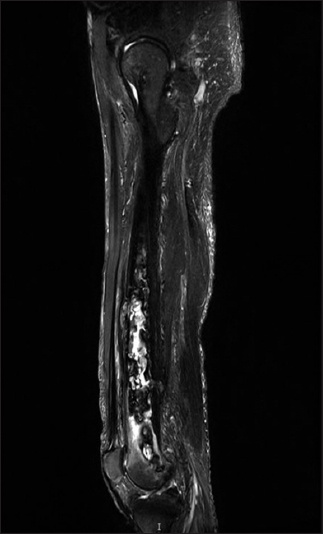
Overall, the findings were consistent with chronic OM of the right femur, with sequestra and multiple cloacae seen. There was inflammation of the adjacent vastus intermedius muscle and an abscess collection extending from the posterior cloaca to the vastus intermedius muscle medially and the subcutaneous tissues inferior-medially before discharging to the dermis at the medial aspect of the distal femur. Based on the findings, our patient was diagnosed with chronic OM involving his right femur, tibia and fibula. The formation of sequestrum typically marks the beginning of chronic OM. Externally, the presence of a draining sinus tract is the hallmark of chronic OM.(1)
After discussion, the patient consented to surgery and underwent right distal femur debridement and bone curettage. Intraoperatively, a chronic discharging sinus was visualised over his right medial knee, without involvement of the knee joint. The bone marrow in the distal femur had a grotty appearance, and the cloacae in the distal femur contained brownish necrotic tissue. Specimens taken from the sinus tract and bone were sent for culture and histology. The Gene-Xpert test was negative for tuberculosis. Both sinus and bone tissue cultures grew pan-sensitive E. tarda, suggesting that this was the likely causative agent. The histopathology report of the intraoperative specimen found sections showing cortical bone with adipocytic marrow tissue. There were multiple fragments of degenerate collagenous stroma, and scattered embedded dead and viable bony spicules, chronic inflammatory aggregates, cholesterol clefts and old haemorrhage were noted. No malignancy was seen. These features were in keeping with chronic OM. As E. tarda is commonly found in marine and freshwater fishes,(2) we questioned our patient further and discovered that he had previously worked as a fisherman in Indonesian seas for 15 years and had also been a fishmonger in a local wet market for 2–3 years from the 1980s to early 1990s.
In terms of management, after surgical debridement, a peripherally inserted central catheter line was placed and the patient received four weeks of intravenous ceftriaxone through the outpatient parenteral antibiotic therapy clinic. He experienced good resolution of symptoms and downtrending inflammatory markers, and remained well and afebrile.
E. tarda infection in humans most frequently presents as gastroenteritis. Extra-intestinal manifestations are rare but include soft tissue infections, OM(3) and bacteraemia.(4) Our patient worked closely with fish as a fisherman and later as a fishmonger, hence it is likely that he had been infected through direct contact with these reservoirs. It is possible that the infection remained chronic in his bones all these years, as E. tarda is known to be able to survive intracellularly and avoid phagocytic killing with the help of the Type III secretion system, which suppresses cellular apoptosis.(5) To our knowledge, there is no literature on the duration of its survival in humans. Although these are commonly identified and reported as E. tarda, there is ambiguity in differentiating between isolates from fish and those from humans (with the new proposed Edwardsiella piscicida and Edwardsiella anguillarum species) and possible misclassification as the same species (i.e. E. tarda).(6) Nevertheless, this case report adds to the current limited understanding of Edwardsiella infections in humans and potentially represents the first observational evidence that Edwardsiella may persist within human tissues for a prolonged period of time. Clinicians should be aware of this possibility and further research is warranted.
Yours sincerely,
Acknowledgements
We thank Prof Leung Ka Yin, Guangdong Technion-Israel Institute of Technology, China, and Prof Mok Yu-Keung Henry, National University of Singapore, Singapore, for providing helpful guidance and insights into the microbiology of


