Mrs Wong brought her seven-month-old son, Malcolm, to your family clinic for symptoms of diarrhoea over the past week. There was no associated fever, vomiting or bloody stools. Malcolm’s activity levels and behaviour were not affected. Examination revealed a cheerful, well-thrived boy with normal abdominal examination findings. There was mild perianal erythema without any fissures or tags. Mrs Wong was very anxious and wanted further investigations and medications for her son’s illness. She was also unsure about how to hydrate and feed Malcolm during this period.
WHAT IS DIARRHOEA?
Diarrhoea is defined by the World Health Organization (WHO) as passage of three or more loose or liquid stools per day or more frequent passage than is normal for the individual. Based on the duration of the presentation, it can be acute or chronic. When symptoms last for more than 2–4 weeks, the diarrhoea is termed as persistent or chronic.(1)
HOW RELEVANT IS THIS TO MY PRACTICE?
Acute diarrhoea in the paediatric age group is one of the most common presentations in the primary care setting. Globally, it is the fifth leading cause of death in children under the age of five years, rotavirus being the leading aetiology in this age group.(2) In countries where rotavirus vaccination is routine, norovirus is the leading cause.(3) Most cases of diarrhoea can be diagnosed clinically and rarely need any laboratory investigations. Presentation with acute watery, non-bloody diarrhoea indicates a viral aetiology, whereas diarrhoea with bloody stools and high-grade fever indicates bacterial infection.(4) Some surgical conditions such as appendicitis and intussusception may also present with loose stools. Family physicians should be able to assess and appreciate the extent of dehydration in children with diarrhoea, as failure to recognise it could lead to severe dehydration, electrolyte imbalance, renal failure and even death. For children with mild to moderate dehydration, oral rehydration therapy remains the mainstay of treatment.(5)
In this article, we present a practical approach to a child with diarrhoea and attempt to answer some of the common questions encountered in routine general practice.
WHAT CAN I DO IN MY PRACTICE?
Clinical approach
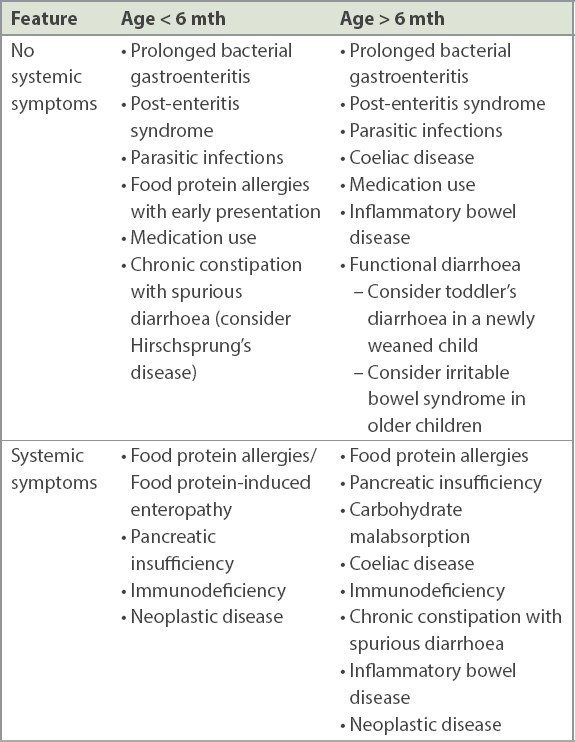
The clinical approach involves, firstly, segregating the cases into acute and chronic diarrhoea. Most childhood diarrhoeal diseases form a continuum, with the majority resolving within the first week of illness.(6) Chronic diarrhoea refers to persistence of loose stools for at least 14 days(1) and would entail a more complex approach that involves an age-specific dichotomisation of disease. For example, infants and toddlers could possibly have issues related to malabsorption or persistent intestinal infections, whereas causes such as inflammatory bowel disease (IBD) or irritable bowel syndrome are considered in adolescents. These cases usually warrant referral to a tertiary care centre.
A detailed history and systematic physical examination remain the key foundation in the diagnostic evaluation of any child presenting with diarrhoea.(4)
History
The following questions are important for evaluating the possible causes of diarrhoea:
- Patient’s age
- Background medical history and familial predispositions (e.g. IBD)
- Nature of stools and duration (separating acute from chronic diarrhoea)
- Recent illnesses
- Associated symptoms including: (a) abdominal symptoms such as vomiting, abdominal pain or distension, bloody or mucoid stools, history of previous constipation; (b) dietary review such as recent change, weaning, discontinuation of breast milk or formula, bottle hygiene, addition of new foods, exposure to unsanitary or raw food products; (c) constitutional symptoms such as fever, loss of appetite or weight, concomitant rash, oral ulcers and joint pains; and (d) symptoms related to hydration status, such as percentage of usual volume managed orally, oliguria, lethargy
- Contact history including exposure to unsanitary conditions, day-care attendance and sick contacts
- Drugs or remedies taken and immunisations
- Travel history
Physical examination
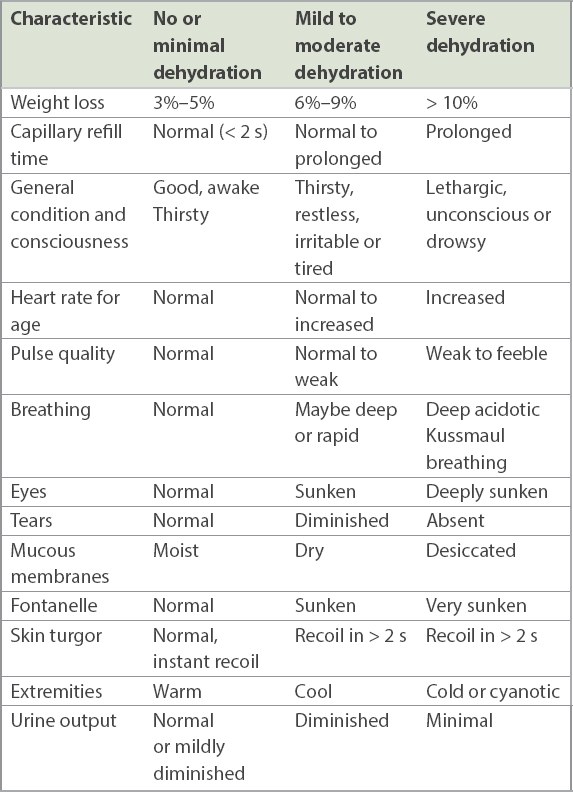
A complete examination always includes a general inspection of the health status of the child as well as his/her vital signs and growth parameters. Review recent weight values, if available, to check for any significant weight loss. Pay close attention to signs of dehydration such as restlessness, lethargy, altered mentation, skin turgor and capillary reperfusion time (
- Abdominal examination: look for any tenderness, rebound, organomegaly or masses
- Stool examination: if possible, review the stools or pictures of recent stools, looking out for fresh or stale blood, mucoid stools or steatorrhea, food particles
- Signs of malnourishment such as muscle wasting, ascites or oedema
- Stigmata of chronic disease
WHAT ARE THE MAIN CAUSES?
Causes should be dichotomised into acute and chronic diarrhoea (
Fig. 1
Flowchart shows approach to aetiology of diarrhoea based on chronicity. CMPA: cow milk protein allergy; GE: gastroenteritis
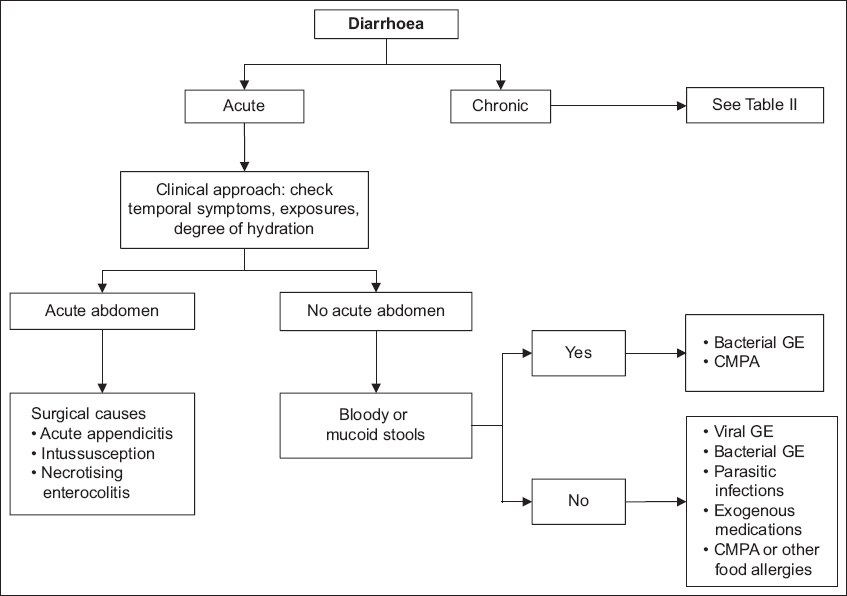
Table II
Causes of persistent or chronic diarrhoea by age group.
Acute diarrhoea
Infectious aetiologies
Rotavirus, norovirus and adenovirus are the most common pathogens for cases in children aged under five years, with viral pathogens accounting for up to 90% of diarrhoeal cases. Leading bacterial pathogens include Escherichia coli and non-typhoidal Salmonella, followed by Shigella and Vibrio parahaemolyticus.(5,8) Bacterial and viral gastroenteritis cannot be definitively distinguished on clinical grounds alone; however, bloody mucoid diarrhoea and high fever are likely to be associated with bacterial pathogens. Management is largely similar for both pathologies in a well, non-toxic child. These illnesses are usually self-limiting. Efforts should be made to identify red flags and signs of moderate to severe disease that require appropriate treatment in the tertiary centre.
Infections such as giardiasis typically present with an acute watery diarrhoea, abdominal pain, abdominal distension and, if persistent, can result in weight loss or faltering growth. A stool test would help to confirm the diagnosis.
Non-infectious aetiologies
Diarrhoea may be a non-specific symptom of an acute surgical abdomen such as in appendicitis, necrotising enterocolitis or intussusception, particularly in younger children. Careful examination for signs of toxicity and acute abdomen would allow diagnosis of these conditions and warrant immediate referral to the emergency department.
Diarrhoea may be seen after antibiotic use, attributable to alterations in intestinal gut flora caused by the antimicrobial agent. A thorough history of use of antibiotics, laxatives or traditional medications with adequate advice and cessation of the triggering medication may be sufficient to address the issue.
Chronic diarrhoea
We propose that it would be prudent to approach cases of chronic diarrhoea based on age, as the causes vary widely according to age group (
Re-infection or co-infection may result in gastroenteritis beyond two weeks’ duration. Often, there is concomitant damage to the intestinal mucosa, causing post-enteritis syndrome. On its own, parasitic infections can run a chronic course, resulting in persistent diarrhoea.
Post-enteritis syndrome is attributed to food sensitisation and secondary disaccharidase deficiency. Reinfection with another enteric pathogen is possible. Elimination diets may be useful.
Non-infectious aetiologies in infants aged below six months include cow’s milk or soy milk protein allergy and food protein-induced enterocolitis syndrome (FPIES). Food allergies may cause chronic diarrhoea through a non-immunoglobulin E-mediated mechanism. Although persistent diarrhoea is common, with increased education and resources, these patients may also present acutely to the primary care physician, especially if there has been a recent change in milk feeds. Depending on the severity of the syndrome, they could present in the first few months of life with diarrhoea, bloody stools or failure to thrive. Primary care physicians should be equipped with knowledge on handling such cases and appropriate anticipatory advice for parents. Elimination of cow’s milk from a breastfeeding mother’s diet or a trial of hydrolysed feed may be both diagnostic and therapeutic.
Gluten enteropathy or coeliac disease typically occurs in Caucasians but is increasingly seen in Singapore’s diverse population. It presents in children aged between six months and three years who are being weaned, owing to the addition of the following grains: barley, rye, oats and wheat. They present with chronic symptoms such as alternating diarrhoea with constipation, abdominal distension and faltering growth; however, gluten enteropathy can also present non-specifically with frequent loose stools in an otherwise well child. A trial of elimination of gluten can aid in diagnosis. Children with autoimmune disorders such as Type 1 diabetes mellitus are at increased risk. All suspected cases should be referred to a tertiary centre for further testing and management.
Cases with pancreatic insufficiency such as children with cystic fibrosis or Shwachman-Diamond disease have a classic presentation of steatorrhoea, flatulence and growth retardation.
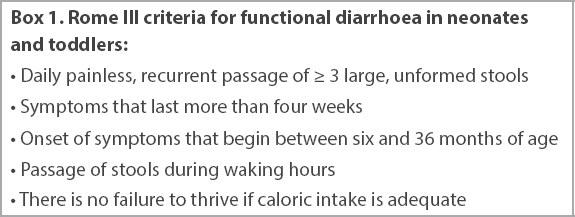
The term ‘toddler’s diarrhoea’ was coined for a syndrome in which toddlers develop functional diarrhoea with frequent passage of loose stools on a daily basis but have adequate growth and a normal examination. There is usually an absence of stool passage at night. It is a diagnosis of exclusion, but the Rome III criteria may be useful for diagnosis (
Box 1
Rome III criteria for functional diarrhoea in neonates and toddlers:
Causes of diarrhoea in infants aged more than six months include IBD, irritable bowel syndrome or other rare causes that overlap between age groups, such as hyperthyroidism, immunodeficiency or neoplastic diseases.
IBD is a disease wherein inflammation of the intestines and colon can lead to persistent symptoms. There may be other systemic symptoms including weight loss, reduced weight gain and abdominal pain. Extra-intestinal manifestations include rash, arthralgias, oral ulcers or perianal disease. Colonoscopy and biopsy are needed for definitive diagnosis. All cases should be referred to a paediatrician.
Irritable bowel syndrome is a non-specific functional diarrhoea that occurs in teenage patients, who present as a well child with normal growth parameters. History usually describes alternating diarrhoea and constipation, and physical examination is always normal. This is a diagnosis of exclusion.
Hyperthyroidism should be considered in a child with other features of hyperthyroidism such as resting tachycardia, excessive sweating, hyperactivity or weight loss. Immunodeficiency (primary or secondary) such as HIV, severe combined immunodeficiency or common variable immunodeficiency should be considered. Neoplastic diseases such as spurious diarrhoea due to chronic constipation (i.e. encopresis) can be diagnosed easily with an adequate history and physical examination.
WHAT INVESTIGATIONS SHOULD BE UNDERTAKEN?
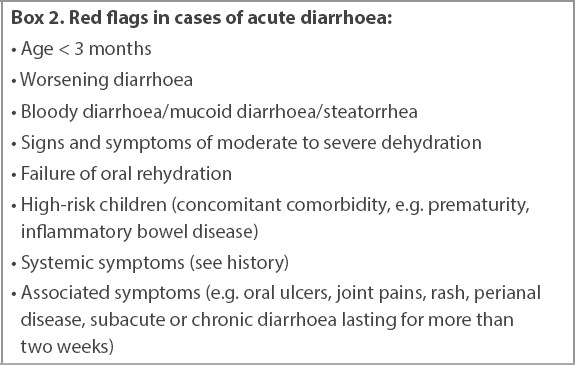
Investigations are warranted in cases of subacute or chronic diarrhoea, diarrhoea with associated red flag features (
Box 2
Red flags in cases of acute diarrhoea:
Blood investigations
The choice of blood tests is directed based on clinical suspicion after appropriate assessment of the patient. For example, in dehydration, checking glucose levels, full blood count and renal panel would be most appropriate, whereas in cases of chronic disease with inflammatory features, a blood count and inflammatory markers, and concurrent stool testing would be more suitable.
In a full blood count, look out for anaemia and thrombocytosis, which would indicate an ongoing chronic inflammatory process. A raised white cell count and neutrophilia suggest a bacterial aetiology, whereas cytopenias are relevant in cases of immunodeficiencies (primary or secondary), viral aetiologies or immune-mediated conditions.
Renal panel and glucose levels are indicated in cases of moderate to severe dehydration, to observe for hypo- or hypernatremia, hypokalaemia, hypoglycaemia, metabolic acidosis or raised urea and creatinine levels.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level are inflammatory markers that may be raised in cases of chronic diarrhoea. CRP level is usually higher than ESR for infective causes, while a higher degree of ESR derangement compared to CRP may prompt the suspicion of IBD or other inflammatory pathologies.
Stool investigations
Stool microscopy, culture and antigen-based modalities are time consuming, poorly sensitive and not available for all pathogens.(4) Therefore, investigations involving diagnostic testing of stool are not routinely recommended, as demonstration of the pathogen is likely to be clinically irrelevant to both diagnosis and management. Accurate clinical assessment remains the mainstay for management decisions.(4,8)
However, stool testing may be considered for patients with chronic diarrhoea of more than two weeks’ duration to direct antimicrobial therapy. Stools may be sent for culture and microscopic evaluation of ova, cysts and parasites. Stool rotavirus testing is not routinely recommended for uncomplicated cases of acute diarrhoea; however, it may be useful in the inpatient setting to predict the duration of symptoms and to prognosticate patients as well as for parental counselling.
Further evaluation based on clinical suspicion can be undertaken at the specialist level, as follows:
- Coeliac disease screen: anti transglutaminase antibody, anti-endomysial antibody and total serum immunoglobulin A, followed by confirmatory intestinal biopsy
- Testing for pancreatic exocrine function: amylase, lipase, faecal elastase
- Testing for food allergies through skin prick or patch testing
- Faecal calprotectin indicating an inflammatory intestinal process
- Faecal occult blood
- Endoscopy and biopsy
WHAT ARE THE PRINCIPLES OF MANAGEMENT IN PRIMARY CARE?
Oral rehydration
Most acute diarrhoeal illnesses are self-limiting, and the goal of therapy is to prevent dehydration. Unless there are signs of a surgical abdomen, for which an immediate referral to an emergency department is required, patients should be allowed to drink orally.
Box 3
Advice for parents of children with acute gastroenteritis:
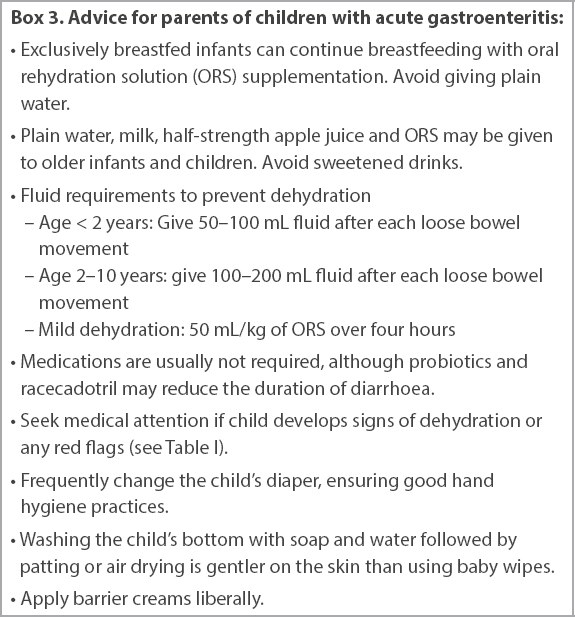
Most fluids that children normally take can be continued to prevent dehydration. Infants who breastfeed should continue to do so, although oral rehydration solution (ORS) may be used as supplementation between feeds. Plain water should not be given to babies below six months of age, and there is no need to dilute the milk preparation or change to a lactose-free brand for formula-fed infants. Plain water, milk and half-strength apple juice can safely be given to older infants and children together with ORS, although some children may find the latter unpalatable. Children should be encouraged to eat. There are no specific foods to avoid while recovering from gastroenteritis, but fluids with high sugar content, such as commercial carbonated beverages and fruit juices or sweetened tea should be avoided, as they can cause osmotic diarrhoea.(1)
As a guide to prevent dehydration, in addition to giving the children as much fluid as they desire until the diarrhoea stops, after each loose bowel movement, children younger than two years should be made to drink 50–100 mL of fluid, and those aged between two and ten years should be made to drink 100–200 mL of fluid.(1) Children should also be encouraged to continue their regular diet, although small frequent feedings may be better tolerated.
Children showing signs of mild dehydration can be given oral rehydration therapy (ORT), which consists of giving 50 mL/kg of ORS over four hours, in small divided doses.
Children with moderate or severe dehydration should be referred to the emergency department. ORT may also be given to children with moderate dehydration at a target of 100 mL/kg over four hours, but this is better performed in the emergency department where they can be placed under observation for a longer period, and a decision can be made to admit them if they fail to drink sufficient fluid.
Pharmacological agents
Certain strains of probiotics, namely Lactobacillus GG, Saccharomyces boulardii and Lactobacillus reuteri SD2112, have been shown to reduce the duration of diarrhoeal illnesses by almost one day. Although the clinical benefit is small, probiotics are considered safe and hence are still recommended. (12,13)
Racecadotril is an antisecretory agent that has been shown to be effective in reducing secretory diarrhoea, including that caused by rotavirus. It has been shown to reduce the duration of diarrhoea as well as the mean stool output and can reduce hospital admissions. Racecadotril is well tolerated and has fewer side effects than loperamide.(13,14)
The anti-motility agent loperamide, an opioid-receptor agonist, is contraindicated in children less than two years of age and not recommended in the management of acute gastroenteritis in children in general. While it may have some efficacy in reducing the duration of diarrhoea, it also has a higher incidence of adverse effects, including ileus and sedation, compared to other available treatments.(13,14)
Diosmectite is an adsorbent that can reduce the duration of diarrhoea and cumulative stool output. Other adsorbents are not recommended.(13)
The majority of well children who develop diarrhoea do not require antibiotics. Antibiotics should only be used to treat hospitalised children, or those who attend childcare who are confirmed to have Campylobacter or Shigella, as this can reduce transmission. On the other hand, shedding of Salmonella is prolonged after antibiotic use.(13)
Children aged more than six months from developing countries where zinc deficiency is common will benefit from zinc supplementation during diarrhoeal illnesses. However, for developed countries such as Singapore, where zinc deficiency is rare, there is no additional benefit of giving zinc.(13)
Anti-emetics are not routinely recommended in children with acute gastroenteritis, owing to the risk of side effects. Ondansetron and domperidone may have possible cardiac effects, and while ondansetron may reduce vomiting, it may increase stool output. Other anti-emetics such as metoclopramide, dexamethasone and dimenhydrinate have adverse effects and have not been shown to reduce vomiting.(13)
Prevention of infectious diarrhoea
Diarrhoeal illnesses are very contagious, and good hygiene is vital in preventing the spread of these diseases. Caregivers should wash their hands after each diaper change and before food preparation. Good bottle hygiene using a steriliser is important for infants aged below 12 months. Rotavirus vaccination is also effective in reducing the severity of rotavirus infections and preventing hospital admissions.(13) The vaccines, which are administered in a two- or three-dose series, can reduce the risk of severe infections by over 80%,(8) and there is no increased risk of intussusception if they are administered within the recommended ages as per the manufacturer’s instructions. Faecal shedding of the rotavirus antigen may occur after vaccination, although there is no data regarding the transmissibility of rotavirus from the vaccine antigen; nevertheless, good hand hygiene is important.
Use of special milk formulas
There is usually no need to change milk formulas for children with age, although changing to a lactose-free formula or soy milk formula for several days can be considered when post-enteritis syndrome develops.
If cow milk protein allergy (CMPA) is suspected, milk products should be eliminated from the mother’s diet if she breastfeeds her infant. An extensively hydrolysed formula (such as Similac Alimentum or Alfare) should be chosen if the infant is not exclusively breastfed, and should be continued for six months, until the infant is at least 9–12 months of age. Goat and soy milk should be avoided, as they have been shown to have significant cross-reactivity with cow’s milk. For severe CMPA with failure to thrive, significant bloody stools causing anaemia, or features of FPIES, the patient must be referred to a specialist and any food challenges must be performed in the hospital.(15)
Caring for the child’s perineum
Erythema and excoriation of the perianal and surrounding areas can occur owing to diarrhoeal illnesses, and these can be distressing for the patient. Diarrhoea irritates the skin, and diapers should be changed frequently. During a diaper change, avoid using baby wipes or toilet paper in a wiping motion; instead, wash with gentle soap and water, and pat dry or air dry. Barrier creams such as those containing zinc oxide should be liberally applied.
TAKE HOME MESSAGES
-
Diarrhoea is defined by the WHO as passage of three or more loose or liquid stools per day, or more frequent passage than is normal for the individual.
-
Most cases of acute diarrhoea are infective in nature, but some may be due to surgical causes (e.g. intussusception or appendicitis), particularly in young children.
-
Most cases of acute, non-bloody diarrhoea do not require investigations. Indications for investigations include ill-appearing patients, bloody diarrhoea, persistent diarrhoea, significant travel or exposure history and features of a surgical abdomen.
-
Post-infectious enteritis may occur after acute viral gastroenteritis and is usually mild and self-limiting.
-
The mainstay of treatment is rehydration. Probiotics may shorten the duration of infectious diarrhoea.
-
Antibiotics should not be routinely used for children with acute diarrhoea. Anti-motility agents and anti-emetics should not be given for acute diarrhoea owing to the risk of side effects.
You informed Mrs Wong that her baby was having acute diarrhoea, most likely due to a viral cause. The baby was not dehydrated and appeared to be well. You said that any other tests and investigations would not be necessary or helpful at this point. Antibiotics were also not recommended, as viral diarrhoea is expected to resolve on its own within a few days. She was advised to continue breastfeeding the baby, with no need to dilute the milk or arrange any special formula milk. An oral rehydration solution was prescribed to be given in between feeds and after every episode of loose stools. You also advised Mrs Wong to avoid giving her baby sweet fruit juices and carbonated drinks, as they could worsen the diarrhoea. For the irritation around the baby’s buttocks, you advised her to change the baby’s diapers frequently, wash the area gently with soap and water, and let it air dry instead of using wet wipes. You also prescribed a barrier cream. As the diarrhoea was very infectious, you asked her to maintain strict hand washing before any food preparation and after changing diapers, and to maintain good hygiene at home. Mrs Wong was very pleased that all her questions had been answered and her fears allayed.
SMJ-62-629.pdf