Abstract
INTRODUCTION
Singapore has one of the world’s most rapidly ageing populations. Osteoporosis is associated with significant morbidity and mortality from hip fractures in the elderly. This pilot study aims to evaluate the knowledge, attitude and practice of osteoporosis among Singaporean women aged ≥ 65 years, and assess barriers to osteoporosis screening.
METHODS
We conducted a cross-sectional survey of 99 English-speaking women aged ≥ 65 years at two SingHealth polyclinics by convenience sampling. The validated Osteoporosis Prevention and Awareness Tool was used to assess their knowledge about osteoporosis prevention and awareness and perceived barriers to osteoporosis screening. Osteoporosis health education was provided, and bone mineral density (BMD) screening was offered to all participants.
RESULTS
The response rate was 91.6%. The majority of the participants (54.5%) had low knowledge of osteoporosis, and only 12.1% had high knowledge scores. Higher education levels were associated with higher knowledge scores (p = 0.018). Although participants with higher knowledge scores were more willing to undergo osteoporosis screening, these findings did not reach statistical significance (p = 0.067). The top reasons for declining BMD testing were misconceptions that lifestyle management is sufficient to prevent osteoporosis, poor awareness and knowledge of the disease, and the perceived high cost of BMD testing.
CONCLUSION
Interventions should focus on osteoporosis education and, eventually, BMD screening for less-educated patients. Health education should rectify common misconceptions of the disease, increase awareness of osteoporosis and improve screening rates.
INTRODUCTION
The proportion of Singapore residents aged ≥ 65 years has increased from 8.8% in 2009 to 14.4% in 2019.(1) The incidence of hip fractures in Singapore has also increased because of its ageing population.(2) Hip fractures in the elderly are often fragility fractures secondary to undiagnosed osteoporosis. Bone remodelling is affected by the activity of bone formation by osteoblasts and bone resorption by osteoclasts. Ageing tilts this balance towards osteoclast activity and leads to a decrease in bone mass and weakening microarchitecture, resulting in osteoporosis and a higher risk of fragility fractures. Osteoporosis – in combination with other factors associated with ageing such as nutrition, physical activity, comorbid medical conditions and drugs – increases the risk of falls and fragility fractures.(3) A fragility fracture is defined as a fracture that occurs with minimal trauma, such as a fall from one’s standing height or lower with no other identifiable major forces.(4) Among osteoporosis-related fragility fractures, hip fractures and vertebral fractures have the highest socioeconomic burden on society and lead to significant morbidity and mortality. Hip fractures are associated with increased risk of mortality within the first few years after the injury(5) and can be a significant economic burden from acute inpatient management of hip fractures, rehabilitation after hospitalisation and additional fractures if osteoporosis is untreated.(6) Higher mortality from hip fractures is noted in patients from lower socioeconomic status, elderly individuals with other medical conditions, delayed operations, those not taking anti-osteoporosis drugs after the fracture and those with more severe fractures. With an increasingly ageing population and increasing incidence of hip fractures, timely screening for osteoporosis and appropriate, early treatment will reduce the risk of a fracture and fracture-related mortality and economic burden.
Although osteoporosis leads to deterioration in quality of life and quality-adjusted life-year, which improve with treatment, osteoporosis is unfortunately underdiagnosed and undertreated in Asia. Some of the reasons cited for underdiagnosis include inadequate dual-energy X-ray absorptiometry (DEXA) machines, lack of awareness among the public and professionals, the asymptomatic nature of osteoporosis, inaccessibility to care and high cost of diagnostics. Approximately 30% of the doctors were not aware of the guidelines for bone mineral density (BMD) testing, and less than 30% of doctors would perform BMD when faced with patients with fractures.(7) A population-based survey of women aged ≥ 45 years in Singapore demonstrated that only 58% of the sample had heard of osteoporosis; these women tended to be younger, better educated, have regular exercise, or are single.(8)
Various countries and societies such as the National Osteoporosis Foundation,(9) United States Preventive Services Task Force,(10) and International Society for Clinical Densitometry (Asia Pacific consensus)(11) have recommended a population-wide strategy for women aged ≥ 65 years to undergo BMD screening using DEXA. Higher-risk populations below the recommended age can be identified using pre-screening tools such as the Osteoporosis Self-assessment Tool for Asians (OSTA)(12) or the Fracture Risk Assessment Tool (FRAX) developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases at the University of Sheffield.(13)
Osteoporosis awareness, diagnosis and management are important for early diagnosis and prevention of hip fractures and the associated morbidity, mortality and economic burden of treatment. In this pilot study, we evaluated the knowledge, attitudes and practices towards osteoporosis of Singaporean women aged ≥ 65 years and how these are associated with willingness to screen for osteoporosis. We also assessed perceived barriers to undergoing osteoporosis screening in this population. Many factors contribute to the poor osteoporosis screening rate in our population. We hypothesised that lack of awareness and understanding of osteoporosis is a significant factor leading to low screening rates. In our study, we aimed to explore some of these factors so that targeted interventions can be designed to improve osteoporosis screening rates.
METHODS
We conducted a cross-sectional survey of 99 English-speaking women aged ≥ 65 years at two SingHealth Polyclinics in Singapore, Polyclinic A and Polyclinic B. Polyclinics in Singapore are government subsidised primary care clinics. Women at the two polyclinics were selected by convenience sampling from the clinic waiting areas. Participants were recruited if they met the following inclusion criteria: female gender, aged ≥ 65 years, ability to read English, having mental capacity and having the ability to provide informed consent. Those who had any cognitive impairment with a score ≤ 7 on the Abbreviated Mental Test or those who were unable to read English were excluded from the study. The participants were offered a quiet space to complete the questionnaire. The study investigators were available to provide simple clarification if the participants had questions while doing the questionnaire, without prompting them with the answers.
The validated Osteoporosis Prevention and Awareness Tool (OPAAT)(14) was used with permission from the authors to assess participants’ knowledge and awareness about osteoporosis. A validated questionnaire was only available in English and had 30 questions assessing knowledge about osteoporosis pathophysiology, prevention and consequences of untreated disease. Surveys were graded as 1 point for each correct answer and 0 point for incorrect answers or if the participant chose the ‘don’t know’ option. Score cut-offs were based on the original paper. A score of ≥ 24 out of 30 on the OPAAT was considered good knowledge and a score of 19–23 was considered average knowledge. A score of < 19 was considered low knowledge.
Post-secondary education was considered as higher education in our results. Patient barriers to osteoporosis screening were evaluated. Osteoporosis health education was provided, and BMD screening was offered to all participants. Information from the questionnaires was de-identified and transcribed into REDCap for ease of data analysis and assessed for completion. Data was analysed using chi-square analysis in IBM SPSS Statistics version 25.0 (IBM Corp, Armonk, NY, USA). A p-value < 0.05 was considered statistically significant.
RESULTS
A total of 157 women were approached, of whom 119 met the eligibility criteria. Those who did not meet the criteria did not fulfil the age requirement and had limited English language skills. 108 women agreed to participate in the study, and 99 women completed the survey (response rate 91.6%).
The majority of the participants were Chinese and married, with a median age of 70 years. The majority of the participants had completed secondary education and were retired or housewives (
Table I
Key demographics of participants (n = 99).
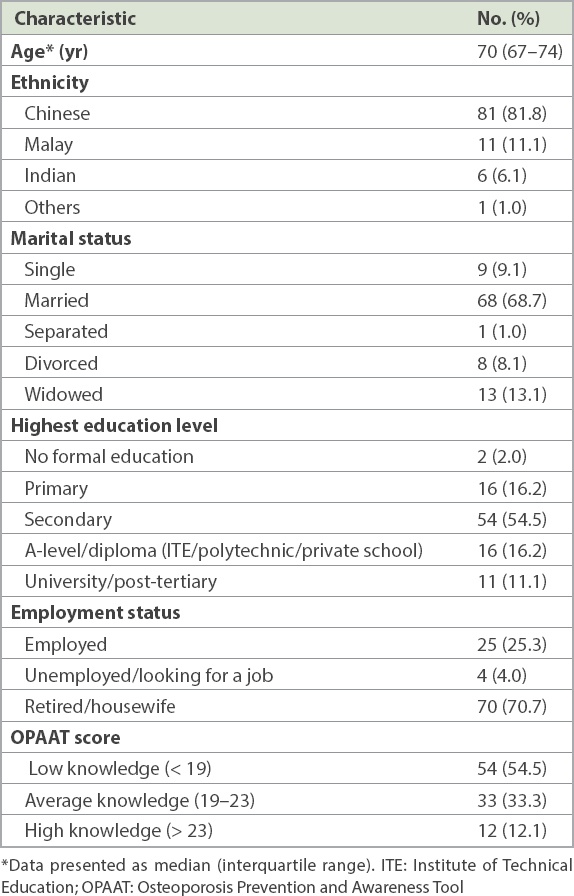
The majority of the participants (54.5%) had a low knowledge score of ≤ 18, and only 12.1% had high knowledge scores of ≥ 24. The mean score was 17.6 ± 4.9, and the median score was 18 (interquartile range 14.5–21.0). The distribution of the scores and breakdown by responses are seen in Tables
Table II
Breakdown of OPAAT scores by question, with correct answers in parenthesis.

Table III
Correlation between education levels and knowledge of osteoporosis using the OPAAT.
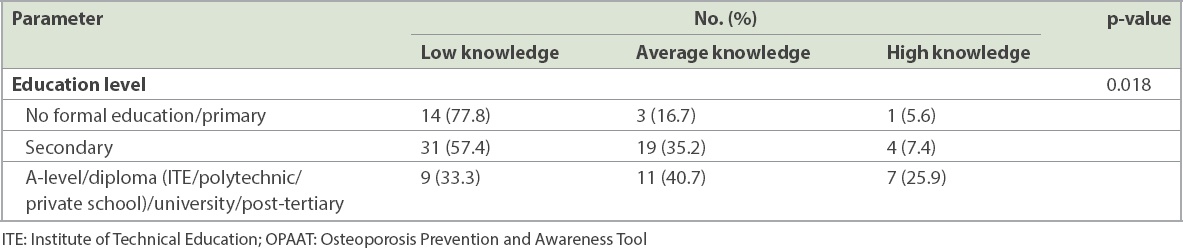
Table IV
Correlation between willingness to undergo BMD screening and knowledge of osteoporosis using the OPAAT.
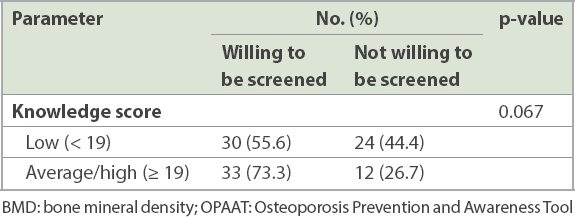
42.4% of the participants had already undergone BMD screening. Among those who had never had BMD screening, 47.4% were willing to undergo screening, and 43.9% were agreeable to schedule it on the same day. The top reasons for declining BMD were misconceptions that lifestyle management (regular exercise and calcium intake) is sufficient to prevent osteoporosis, poor awareness and knowledge of the disease, and the perceived high cost of BMD screening. Other concerns cited include polypharmacy and risk of medication side effects. Similar concerns have been cited for poor adherence to osteoporosis treatment,(16) including time-consuming follow-up appointments, medication costs and side effects, and the perceived lack of importance of osteoporosis treatment.
Incidentally, participants at Polyclinic A were more likely to have previously done BMD screening, compared to those at Polyclinic B (60% vs. 21%, p < 0.001). Education levels and knowledge scores were further evaluated by site to determine any difference in the populations that may support the higher screening rates noted at Polyclinic A. Although participants from Polyclinic A had higher education levels (p < 0.001), there was no significant difference in their knowledge of osteoporosis (p = 0.174).
DISCUSSION
We found that higher education levels corresponded to better knowledge of osteoporosis. The local population appeared to have better knowledge of lifestyle measures to prevent osteoporosis, falls prevention and some complications of osteoporosis. However, participants showed a poorer understanding of the disease’s pathophysiology and confused the symptoms with those of osteoarthritis.
Although it is suggestive that better osteoporosis knowledge corresponded to willingness to undergo osteoporosis screening, the results did not achieve statistical significance in this pilot study. The common barriers to BMD screening cited by the participants also suggested a lack of understanding of the disease and the screening process, affecting the screening rates. A larger-scale study or an educational intervention study(17) would be useful to look for a statistically significant correlation between osteoporosis knowledge and screening rates in our population.
Incidentally, participants from Polyclinic A had a significantly higher rate of osteoporosis screening. However, there was no significant difference in their knowledge of osteoporosis. Beyond the scope of this study, a follow-up study can be considered to explore what motivated the participants from Polyclinic A to undergo osteoporosis screening.
A limitation of our study is that the questionnaire was only available in the English language, which may have created a bias in population selection for this study. Some participants may have had more difficulty comprehending the material, but this should have been addressed by having the study investigator being available to provide simple clarification if the participants had any questions. Follow-up studies are indicated to explore screening rates, knowledge of osteoporosis and barriers to screening in the non-English speaking and less-educated population, which may be more representative of the general population in Singapore.
Another limitation was that some of the participants took longer to complete the survey or were unable to complete the survey if they were called to attend the doctor’s consultation, and the study investigator was unable to follow up with them after the consultation was complete.
Future studies may also investigate the impact of factors, such as OSTA score, FRAX score, existing functional status, physical activity level, and distance from home to public amenities and parks, on osteoporosis knowledge and willingness to undergo BMD screening.
In conclusion, osteoporosis and resultant fragility fractures have significant implications for the quality of life of our elderly patients and result in a significant economic burden on the healthcare system. The less-educated population also lacks osteoporosis knowledge, which leads to misconceptions about osteoporosis and the need for osteoporosis screening. Health education should rectify these common misconceptions of the disease, increase awareness of osteoporosis and improve screening rates.
ACKNOWLEDGEMENTS
We would like to appreciate Winnie Sea Sui Gek, Usha Sankari and Eileen Koh Yi Ling of the SingHealth Duke-NUS Family Medicine Academic Clinical Programme for their roles in study administration, data management and analysis for this study.


