Abstract
Basic Cardiac Life Support (BCLS) or cardiopulmonary resuscitation (CPR) refers to the skills required (without use of equipment) in the resuscitation of cardiac arrest individuals. On recognising cardiac arrest, chest compressions should be initiated. Good quality compressions are with arms extended, elbows locked, shoulders directly over the casualty’s chest and heel of the palm on the lower half of the sternum. The rescuer pushes hard and fast, compressing 4–6 cm deep for adults at 100–120 compressions per minute with complete chest recoil. Two quick mouth-to-mouth ventilations (each 400–600 mL tidal volume) should be delivered after every 30 chest compressions. Chest compression-only CPR is recommended for lay rescuers, dispatcher-assisted CPR and those unable or unwilling to give ventilations. CPR should be stopped when the casualty wakes up, an emergency team takes over casualty care or if an automated external defibrillator prompts for analysis of heart rhythm or delivery of shock.
INTRODUCTION
Basic Cardiac Life Support (BCLS) refers to the recognition of sudden cardiac arrest, calling for help, supporting the circulation, maintaining the airway and supporting breathing without the use of equipment other than personal protective devices. This is also commonly referred to as cardiopulmonary resuscitation (CPR). This skill could be used by a layperson or a healthcare provider in both out-of-hospital and in-hospital settings.
The majority of sudden cardiac arrests occur in the community (i.e. out-of-hospital). The success of the chain of survival depends on the first-responder layperson. The goal of CPR training is to ensure that participants ‘can do’ and ‘will do’ CPR when the need arises. CPR guidelines must be not only scientific, but also simple to follow. Simplification will improve skills retention, decrease the fear of imperfect CPR performance and increase willingness to perform CPR.
In 2015, the International Liaison Committee on Resuscitation (ILCOR) reviewed and updated the consensus document on the science based on the latest developments in research. The International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations (CoSTR) was published in the journals Circulation(1,2) and Resuscitation,(3,4) in October 2015. The various resuscitation councils then formulated their own guidelines based on the 2015 international CoSTR. The American Heart Association (AHA) and European Resuscitation Council (ERC) have published their own guidelines(5,6) on the same issue as the CoSTR document. The following document spells out the Singapore guidelines, as drawn up by the National Resuscitation Council (NRC) Singapore.
HIGHLIGHTS OF CHANGES IN BCLS GUIDELINES SINCE 2010
Recognition of cardiac arrest
Studies have shown that gasping is common (up to 40% of cases) in the immediate phase when casualties sustain sudden cardiac arrest. During the first few minutes of sudden cardiac arrest, the presence of gasping is associated with increased survival. Laypersons or healthcare providers should be taught to recognise gasping as cardiac arrest and not normal breathing, and to begin CPR immediately. Dispatchers should be trained to interrogate callers to elicit the presence of non-responsiveness and absence of normal breathing (including recognition of gasping).(1,2,7)
Pulse check is a difficult technique for both laypersons and healthcare providers to master,(8) and should not be taught to laypersons (recommended in the 2006 and 2011 NRC guidelines).(9,10) Training centres that wish to teach healthcare workers the pulse check as an additional tool for determination of cardiac arrest, to decide whether to start CPR, should use manikins that are able to simulate the presence or absence of a pulse. The healthcare provider should take no more than ten seconds to check for the presence or absence of normal breathing and pulse. If there is no normal breathing or definite absence of a pulse within this time period, the healthcare provider should presume cardiac arrest and start chest compressions.
Technique of chest compression
The landmark for chest compression remains as the centre of the chest (which is at the lower half of the sternum). Studies have shown that use of the inter-nipple line as a landmark to signify the lower half of the sternum for the hand position is not reliable.(11,12) One study showed that there were shorter pauses between ventilations and compressions if the rescuer was taught to ‘place the heel of the hand’ on the lower half of the casualty’s breastbone (and was shown the location), as compared to the conventional method of locating the landmark for chest compression one finger breadth above the xiphoid process by tracing the lower margin of the casualty’s rib cage.(13) In 2011, the NRC BCLS committee decided to retain the conventional method (i.e. locating the xiphoid process by tracing the lower margin of the casualty’s rib cage;
Fig. 1
Landmark for chest compression.

A local study reported a high incidence of compression over the epigastrium among participants during a six-month post-training test.(15) Participants who compressed at the incorrect position on the sternum compressed at a significantly lower average depth than those who compressed at the correct position. Participants who were taught the use of the two-finger method for locating the landmark for chest compression had a significantly higher rate of compressions at the epigastrium.
In the 2016 NRC BCLS guidelines, it is recommended that the rescuer should be taught and shown the location of the landmark for chest compression – lower half of the sternum and centre of the chest on the manikin.(13)
Studies done in both out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest situations showed that rescuers do not compress the chest hard and fast enough, and have frequent interruptions of chest compressions.(15,16) In the 2010 CoSTR, the recommended rate of chest compression was changed for both adults and children, from 100 per minute to at least 100 per minute. The depth of chest compressions was changed from 4–5 cm to at least 5 cm (AHA) or 5–6 cm (ERC) for adults, 5 cm for children and 4 cm for infants.(17,18)
A large study of OHCA adult casualties (n = 9,136) treated by emergency medical service providers found that the maximum survival occurs with a depth interval of 40.3–55.3 mm (peak 45.6 mm).(19) In an observational study of 170 casualties, injuries were reported in 28%, 27% and 49% of casualties who had compression depths of < 5 cm, 5–6 cm and > 6 cm, respectively.(20)
Considering that the body size of Asians is generally smaller than that of people in the West, compression of the chest deeper than 5 cm might not be necessary in Singapore. A study from Japan that investigated the association between the body weight of rescuers and the quality of chest compressions revealed that adequate compression rate and depth among the light body weight group decreased significantly over time as compared to the heavy body weight group. In Asia, a considerable proportion of female doctors or nurses may not be able to compress more than 5 cm in depth due to their small body weight.(21)
Data from a large study (n = 10,371) on adults with OHCA treated by emergency medical service providers found that, after adjustments for chest compression depth, compression rates of 100–120 per minute were associated with greater survival to hospital discharge.(22) The NRC recommends a chest compression depth of about 5 cm (i.e. 4–6 cm) during manual CPR and a chest compression rate of 100–120 per minute.
Chest compression-only CPR
The 2010 AHA and ERC guidelines recommend that all trained rescuers (both healthcare providers and laypersons) should perform conventional CPR (CVC), i.e. chest compression with mouth-to-mouth ventilation.(17,18) This was because a large observational study of OHCA showed that survival was better when CVC, as opposed to chest compression-only CPR (CCC), was provided for paediatric arrests (other than sudden, witnessed collapse of adolescents), asphyxial cardiac arrests in both adults and children (e.g. drowning, drug overdose) and prolonged cardiac arrests (> 15-minute downtime).(23) However, most sudden OHCAs occur in adults and are of cardiac origin.(24,25) 70%–80% of OHCA casualties initially have ventricular fibrillation (VF).(26,27) At the initial phase of sudden cardiac arrest with VF, rescue breaths are not as important as chest compressions, because the oxygen level in the blood remains adequate for the first few minutes after cardiac arrest.(28) In a prospective observational study of bystander-witnessed OHCA casualties with shockable rhythms, those who received CCC had a higher one-month survival rate with favourable neurological outcome than those who received CVC (19.4% vs. 11.2%, p = 0.041).(29) However, the above observational clinical studies were unable to conclude whether lay rescuers should be taught CVC or CCC. Furthermore, we could not ascertain whether bystanders in these OHCA studies received any CPR training, and if so, which CPR training method (CVC or CCC) was received.
Two before-and-after implementation observation studies showed that there was an improved rate of survival in adult OHCA after the implementation of CCC in the community (Arizona, USA and Japan).(26) In Arizona, the survival rate of adult OHCA of cardiac aetiology was 7.8% for those who received CVC, 13.3% for those who received CCC and 5.2% for those who received neither. There was a significant increase in bystander CPR rate, from 28% in 2005 to 40% in 2009, and an increase in the likelihood of bystanders performing CCC vs. CVC (20%–76%).(7)
The 2015 ILCOR recommendations state that chest compressions should be performed for all cardiac arrest casualties and that those who are trained, able and willing to give mouth-to-mouth rescue breaths should do so.(1,2) Bystanders may be trained in CCC for adult OHCA as an alternative to CVC training.(1-4) This recommendation has been reflected in the new AHA and Resuscitation Council of Asia guidelines.(5,30)
A local study showed that during a six-month post-training test, 14.9% of participants who were trained in CCC pretended to do mouth-to-mouth ventilation, only 14.9% were able to perform ≥ 5 effective ventilations (≥ 400 mL), and only 3.7% were able to perform ≥ 10 effective ventilations in five minutes. Most participants who were trained in mouth-to-mouth ventilation were unwilling or unable to perform effective mouth-to-mouth ventilations six months after training. Interrupting chest compression to perform ineffective mouth-to-mouth ventilations is definitely detrimental.(15)
Therefore, the NRC recommends that CPR training for lay rescuers should focus on recognition of cardiac arrest, calling for an ambulance and good-quality manual chest compression, with optional mouth-to-mouth ventilation.
Fig. 2
NRC 2016 Adult Basic Cardiac Life Support one-man cardiopulmonary resuscitation algorithm.
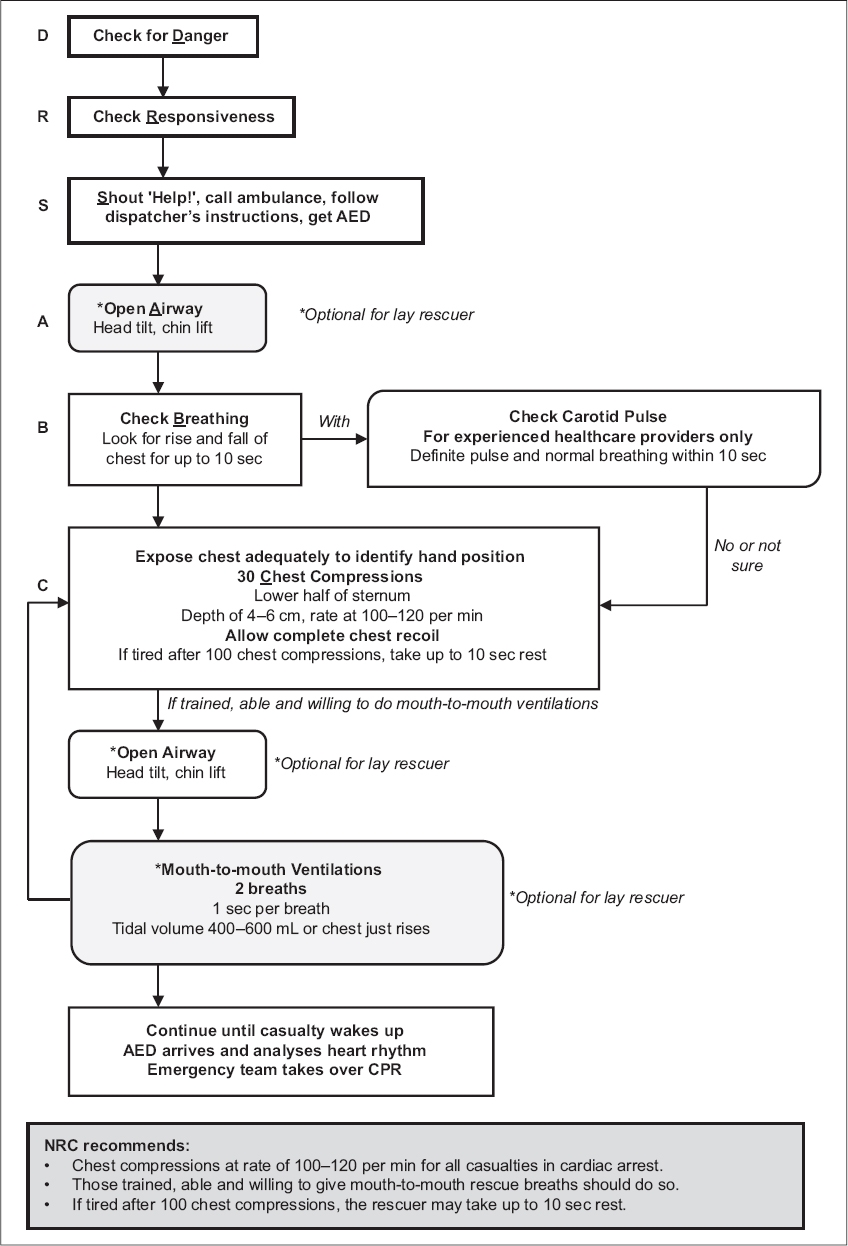
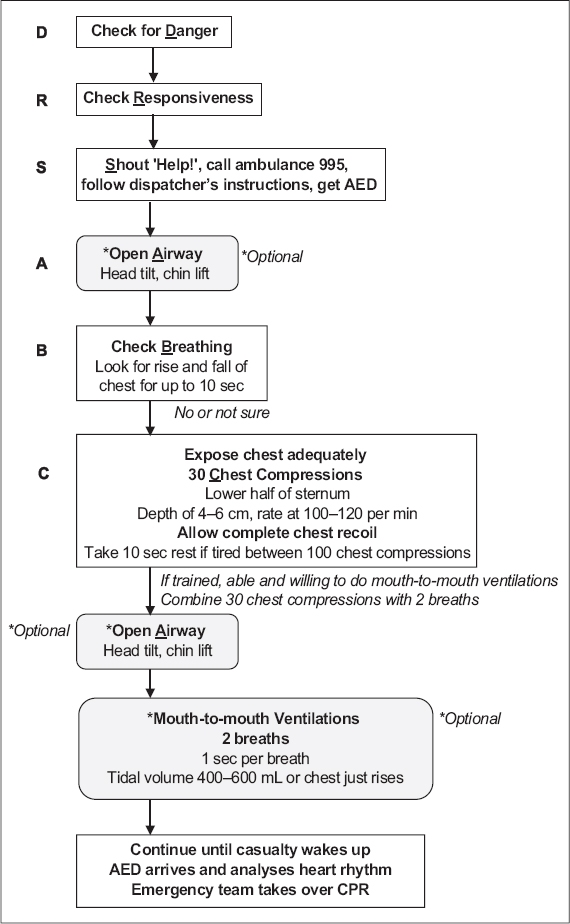
Fig. 3
NRC 2016 Adult Basic Cardiac Life Support one-man cardiopulmonary resuscitation algorithm for the lay rescuer.
Sequence of adult one-man CPR
The recommended sequence of adult one-man CPR for the healthcare provider is as follows:
-
Check for danger: this ensures that the rescuer operates in a safe environment.
-
Check for responsiveness: the rescuer should tap the casualty firmly and ask loudly: ‘Hello! Hello! Are you okay?’
-
If unresponsive: shout for help, call ‘995’ for an ambulance or activate the emergency response system (for in-hospital cardiac arrest), and get an automated external defibrillator (AED) if there is one within a 60-second walking distance. An emergency medical dispatcher can help a lay rescuer recognise a cardiac arrest, and once this is established, the dispatcher should lead the rescuer to begin CPR by providing instructions on how to perform CCC via telephone. Dispatcher-assisted telephone CPR increases the bystander CPR rate and improves the survival rate of cardiac arrest. The emergency medical dispatcher may also be able to locate the nearest AED and summon CPR-trained rescuers in the vicinity.
-
Open airway: head tilt, chin lift.
-
Look, listen and feel for up to ten seconds to check for normal breathing. Gasping is NOT considered normal breathing
-
Checking of pulse, if done, should be left to trained healthcare workers.
-
Checking of normal breathing and pulse should not take more than ten seconds.
-
If unsure of the presence of normal breathing or pulse (for trained healthcare providers only) within ten seconds, start chest compressions.
-
-
Technique of chest compressions
-
Site of compression should be at the centre of the chest and the lower half of the sternum (breastbone).
-
- Ensure adequate exposure of the chest.
- Kneel by the side of the casualty.
- Place the heel of the palm of the other hand on the lower half of the sternum (breastbone) next to the index finger.
- Place the heel of the first hand on top of the second.
- Interlace the fingers of both hands and lift the fingers off the chest wall.
- Straighten both the elbows and lock them into position.
- Position the shoulders directly over the casualty’s chest. Use the body weight to compress the casualty’s breastbone.
-
Depth of chest compression for adults must be at least 4 cm but not more than 6 cm.(15,30,31)
-
The compression rate is 100–120 per minute.
-
Allow complete recoil of the chest wall after each compression. If tired after 100 compressions, take up to 10 seconds of rest.(32)
-
Loud counting of the compressions should be encouraged: 1&2&3&4&5&, 1&2&3&4&10&, 1&2&3&4&15, 1&2&3&4&20, 1&2&3&4&25, 1&2&3&4&30.
-
Perform two ventilations (one second per breath, tidal volume 400–600 mL) after every 30 chest compressions,(18) so that the chest just rises.
-
Check for return of spontaneous circulation.
- The public should continue performing CPR until emergency medical help arrives and takes over, or an available AED prompts the rescuer not to touch the casualty, or the casualty starts moving.
- Healthcare workers who are trained and confident in pulse check should check the pulse after at least five cycles of 30 compressions to two ventilations. Checking of pulse should not take more than ten seconds. If unsure of the presence of a pulse by the end of ten seconds, the rescuer should resume 30 chest compressions to two ventilations (see
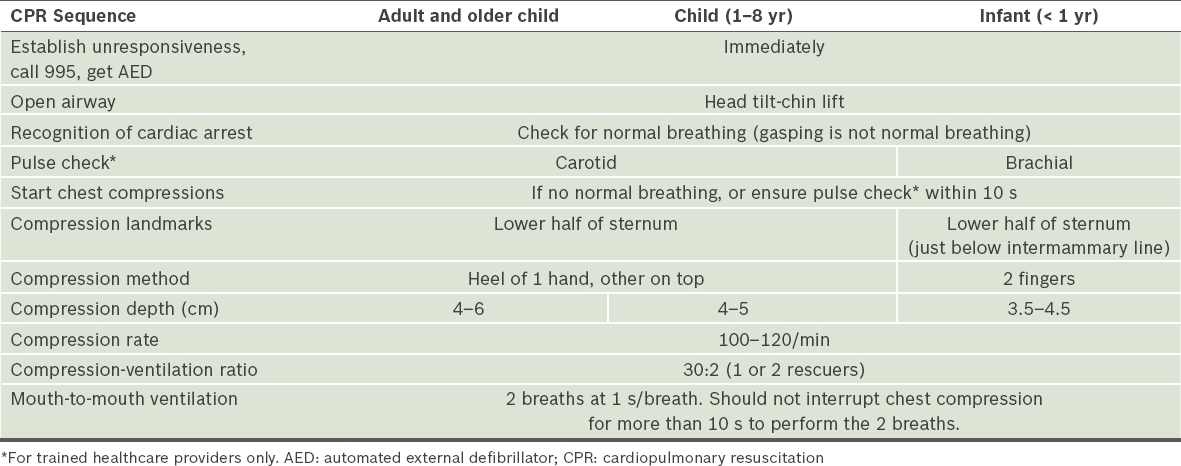
Table I for comparison of CPR sequences across various age groups).
Table I
CPR sequences across age groups.
Two-person CPR
-
If there is more than one trained rescuer, two-person CPR may be more efficient, with one person doing the ventilations and the other the chest compressions.
-
If more than one rescuer is present, they should take turns to perform 30 chest compressions after every two minutes, as fatigue would otherwise set in. One rescuer should focus on chest compressions and the other on ventilations. The changeover should involve minimal interruption of chest compressions (see
Table I for comparison of CPR sequences across various age groups).
Duration of retraining cycle
There is evidence of skills decay within 3–6 months after CPR training, especially mouth-to mouth-ventilations.(31) There is also evidence that frequent training improves CPR skills, responder confidence and willingness to perform CPR. Although the NRC retains the two yearly recertification guidelines for BCLS courses, individuals who are likely to encounter cardiac arrests should consider more frequent retraining.
Relief of foreign body airway obstruction
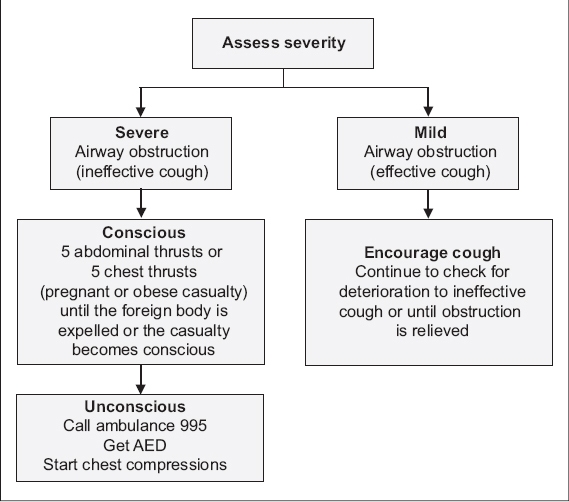
The recommended sequence of actions for relief of foreign body airway obstruction (FBAO) with a responsive casualty is detailed below (
Fig. 4
Adult choking treatment algorithm.
Recognition of FBAO in a person who chokes while eating and clutches his throat:
-
If the casualty is coughing effectively, this means that the airway is mildly obstructed. Do not interfere. Allow the casualty to cough to expel the object himself.
-
In severe airway obstruction, the casualty is unable to speak, breathe or cough effectively, which requires immediate action. The Heimlich manoeuvre, also known as the abdominal thrust, is recommended for the relief of FBAO in responsive adults (more than eight years old) and children (1–8 years old).
-
If the casualty becomes unconscious:
-
Support and position the casualty on his back on a firm flat surface, wherever possible.
- The rescuer should shout for help and activate the emergency ambulance by calling ‘995’.
-
Begin 30 chest compressions immediately.
-
Open the airway with the head tilt-chin lift procedure. The rescuer should look for an object in the mouth and remove it, if found.
-
Check for normal breathing.
-
If breathing is absent, attempt one ventilation.
-
If the chest does not rise, reposition the airway with the head tilt-chin lift procedure.
-
Attempt a second ventilation.
-
Perform 30 chest compressions, repeat the head tilt-chin lift procedure and check for foreign body.
-
Repeat (3d–3h) till help arrives and a healthcare worker takes over, or the casualty starts breathing, coughing, talking or moving.
-
Recovery position
The recovery position is used in the management of casualties who are unresponsive but breathing and have signs of circulation. Several versions of the recovery position exist, each with its own variations. The position adopted should allow free drainage of fluid from the mouth and the upper airway, give stability and enable the casualty to be turned to his side and returned easily and safely onto his back, with due care taken for possible cervical spine injury (
Fig. 5
Photograph shows the recovery position.

Supplementary Material
SMJ-58-353.pdf


