Abstract
INTRODUCTION
Dental caries, which is prevalent in Singapore preschoolers, is a disease that has a major impact on children’s health and places a high cost on the society and health services. Oral health programmes for young children implemented in some parts of the world have been shown to be effective in the prevention of dental caries. We aimed to examine the clinical efficacy of a two-year oral health programme for infants and toddlers in Singapore.
METHODS
90 children and their caregivers participated in the programme, and 64 children, who were 24 months older than the intervention group at the initial visit, were recruited as controls in a quasi-experimental study design. We evaluated the presence of severe early childhood caries (SECC) and d3mfs in the control group at the initial visit and in the intervention group after the completion of the two-year programme.
RESULTS
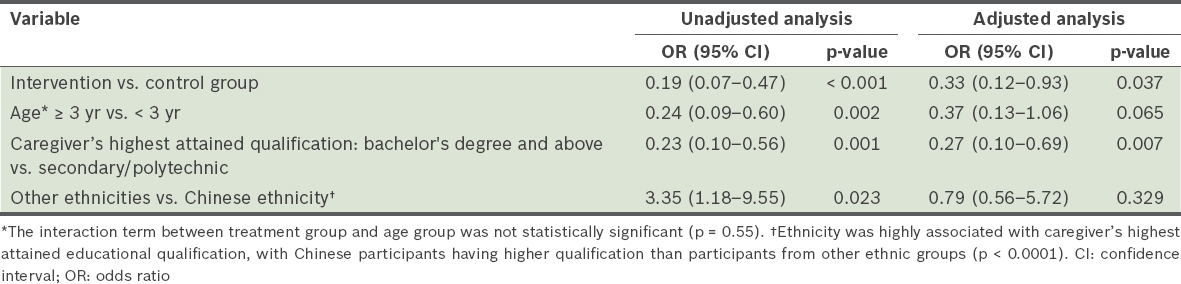
Some children in the intervention (7.8%) and control (31.3%) groups (p < 0.001) had SECC (difference 23.5%, 95% confidence interval 11%–36%). A higher percentage of children in the intervention group had d3mfs = 0 and habits associated with low risk for caries. The odds of SECC in the control group were three times higher than that for the intervention group, and the effect was significant (p = 0.037) after adjustment for other significant risk factors.
CONCLUSION
The preventive oral health programme in Singapore was successful in reducing SECC among infants and toddlers when targeted behaviour modifications were implemented.
INTRODUCTION
Dental caries remains the most common chronic childhood disease affecting children globally.(1-3) Despite being one of the richest countries in the world, with a gross domestic product per capita of SGD 72,711 and a high literacy rate of 96.8%,(4) Singapore continues to struggle with early childhood caries. The implementation of the School Dental Service programme, aimed at preventing and treating dental caries in school-going children (age range 6–18 years), has proven to be extremely successful. Since its inception in 1949, we have seen a significant increase in the number of children (age range 6–11 years) with caries-free dentition, from 27.8% in 1970 to 58.2% in 1994, and a corresponding decline in the incidence of dft (d: decayed, f: filled due to decay, t: primary tooth) and DMFT (D: decayed, M: missing due to decay, F: filled due to decay, T: permanent tooth).(5) The current DMFT value of 0.41 among 12-year-old children puts the country on par with other similar industrialised nations.(6) However, recent studies have indicated a disproportionately high caries prevalence. One study reported a prevalence of 40% among 3–6-year-old children, with a racial and lower socioeconomic status predilection,(7) while another study conducted among 18–48-month-old infants reported a caries prevalence of 48%.(8) Early childhood caries can progress rapidly in deciduous dentition, resulting in pain and infection, affecting a child’s nutritional intake, growth and development, and severely impacting their overall quality of life.(9)
Compounding the issue is the seemingly low oral health awareness among Singaporean parents. Despite the high prevalence of dental caries, only 8% of children aged 3–6 years and 3% of children aged 18–48 months received regular dental care.(7,8) Only 1% of parents were aware of the age one dental visit recommendation by the American Academy of Pediatric Dentistry (AAPD).(8) AAPD recommends that all children should have their first dental visit at no later than one year of age, with a heavy emphasis on preventive messages and anticipatory guidance.(10) A delay in seeking dental care may result in increased severity of disease, leading to more extensive and costly treatments.(11) In addition, general anaesthesia may be required to provide quality dental care for paediatric patients due to behavioural challenges, developmental immaturity and extensive treatment needs. The use of operating theatres for such elective procedures adds on to the cost burden of parents and the society. Early preventive care has the potential to decrease the number of emergency visits and cost of dental care.(11)
Early preventive dental care may be given through a non-invasive infant oral health programme, which includes a comprehensive oral examination, caries risk assessment, preventive services, and anticipatory guidance on diet, non-nutritive habits, growth and development, injury prevention and oral health practices.(10,12) These programmes also maximise exposure to caries-reducing fluoride in a younger population, with fluoride varnish showing excellent effectiveness and safety profile.(13,14) Infant oral health programmes implemented in several parts of the world have been shown to be effective in the prevention of dental caries. Children whose caregivers have attended oral health programmes had lower mean dmfs (d: carious lesion; m: missing due to caries; f: filled due to caries; s: surface) scores,(15,16) lower caries prevalence(17-20) and lower mean carious dental surfaces.(21-23) In addition, children who had early preventive dental care incurred lower dental-related costs compared to those who received care later due to associated restorative costs.(11) On the other hand, there were studies that reported minimal effects on caries reduction;(24,25) which may be culturally related. The implementation of an infant oral health programme has the potential of impacting caries prevalence in the younger population, and perhaps even has long-term effects in older children. However, it requires support from the public health system in terms of collaboration with medical professionals, monetary resources and formal publicity. The objective of this exploratory study was to examine the clinical efficacy of an oral health programme for infants and toddlers in Singapore.
METHODS
A quasi-experimental design was employed for this study. From October 2012 to March 2013, eligible children were recruited from the National Dental Centre Singapore Paediatric Dentistry Clinic, nine primary health outpatient clinics (i.e. polyclinics), and the Singapore General Hospital Baby and Child Clinic. The study received full approval from the SingHealth Centralised Institutional Review Board Singapore (2012/482/D).
Children who were under 18 months of age at recruitment were enrolled in a two-year risk-based preventive oral health programme. At the completion of the two-year programme, outcome measures were evaluated for the intervention group. The quasi-experimental design entailed the recruitment of a matched older control group at their first visit, as it was deemed unethical to provide no intervention in a true prospective control group. Children in the control group were recruited at the same time and outcome measures were taken at enrolment, with no follow-up requirement.
The inclusion criteria for children in the intervention group were: (a) 0–18 months of age; (b) dentate with no congenital condition related to tooth structures; (c) in good health (American Society of Anesthesiologists physical status class I or II) and did not have special healthcare needs; (d) families who could commit to dental visits and planned to reside in Singapore for at least two years; (e) children with no previous dental experience; and (f) signed informed consent by parent or legal guardian. The inclusion criteria for children in the control group were similar, except for the age criterion being 24–42 months. A designated interpreter was provided for each of Singapore’s three major second languages (i.e. Mandarin, Malay and Tamil) if the parent did not speak or read English. Children were excluded if they did not meet the above inclusion criteria or if their parents could not understand any of the four languages.
Each child was assigned to one of four calibrated paediatric dentists. All initial examinations for children in the intervention group were performed in the knee-to-knee position, with a well-directed light source from the dental unit in addition to the room light, using the mouth mirror and gauze to dry the teeth. When necessary, light active restraint by the caregiver was employed. The caries diagnosis was based on visual criteria only. Intraoral radiographs were not taken. Cavitated and precavitated lesions were charted. A demineralised area of enamel with no loss of surface continuity was defined as a precavitated lesion. A cavitated lesion involved a loss of enamel surface continuity. The overall caries risk was assessed using the AAPD caries risk assessment tool for dental providers and based on the clinical judgement of the examiner.(10)
All children received a risk-based preventive programme comprising the following: (a) oral health education about the aetiology of dental caries, caries progression and prevention, and parental oral health; (b) anticipatory guidance on diet, oral health care practices, including tooth brushing and fluoride use, non-nutritional habits, trauma prevention, and growth and development; (c) topical fluoride varnish (5% sodium fluoride; Duraphat®, Colgate, Waltrop, Germany), which was applied on all tooth surfaces for children who were considered at high caries risk;(10) and (d) recommendation for dental review visits.
Children in the intervention group were scheduled for a dental review visit every six months for a period of two years, with the exception of those at high caries risk, who had additional appointments scheduled between their standardised six-month visits. Subsequent dental visits for children in the intervention group involved the same clinical procedure and the same outcome measures were recorded. The major components of the oral health programme were standardised, but the individual content of each component was customised to the child’s history and clinical findings. Children who had treatment needs were referred for dental care. Children who were lost to follow-up or exceeded the window period of one month from the scheduled review visit date were excluded.
Severe early childhood caries (SECC) is defined as any sign of smooth-surface caries in children younger than three years old. For children in the 3–5 years age group, ≥ 1 dmfs in primary maxillary anterior teeth, or dmfs score ≥ 4 (age three years), ≥ 5 (age four years) or ≥ 6 (age five years) surfaces constitutes SECC.(12) The primary outcome measure was the presence of SECC (including precavitated lesions). The secondary outcome measure was the dmfs score. Behavioural changes in dietary habits, oral care practices and oral hygiene status were also compared. Although examiners were not aware of the study groups at the initial visit, blinding was not possible due to the difference in age.
A sample size of 64 patients per group was required to detect a difference of 20% in the proportion of patients with SECC between the two groups (10% vs. 30%) for 80% power at two-sided ± = 0.05. By factoring in a 40% attrition rate from previous studies at this institution, 107 patients and 64 controls were projected for recruitment. For examiner calibration, the intraoral photographs of ten de-identified children were used for inter-examiner agreement among the four dentists who performed the outcome assessments. Dental caries and precavitated lesions were charted. For three patients, cases were re-charted to determine intra-examiner agreement.
Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA). Continuous variables were compared using independent sample t-test and Pearson’s chi-square test, while Fisher’s exact test was used for categorical variables, if appropriate. Comparison of outcomes was done using Mann-Whitney U-test for d3mfs (d3: cavitated carious lesion; m: missing due to caries; f: filled due to caries; s: surface) and Pearson’s chi-square test for the presence of SECC. Odds ratios of the presence of SECC and their 95% confidence intervals (CIs) were calculated from logistic regression analyses. Inter- and intra-examiner agreements were analysed using Kappa statistic.
RESULTS
In all, 107 children were recruited for the intervention group and 64 for the control group. The attrition rate was 15.9% (n = 17), with 90 children in the intervention group completing the study (
Fig. 1
Flowchart of participants shows the key stages of the study. *Three attempts (at different days and times over two weeks) were made to contact the caregiver of each child at the telephone numbers provided at the start of the study. †Children who were lost to follow-up exceeding the window period of one month from the scheduled recall visit date were excluded from the study. d3mfs: decayed, missing and filled tooth surfaces; SECC: severe early childhood caries
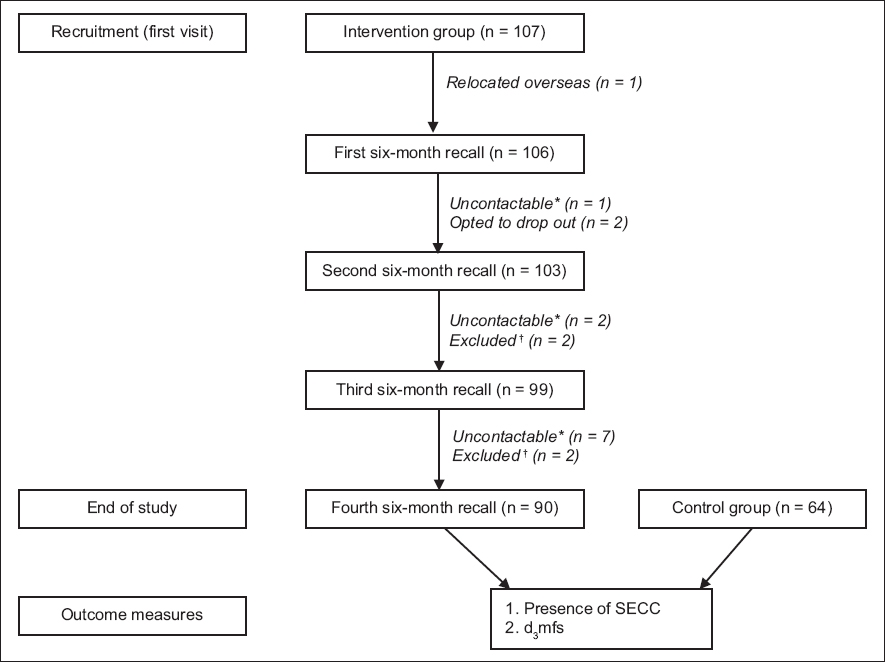
Table I
Demographics of the study population.
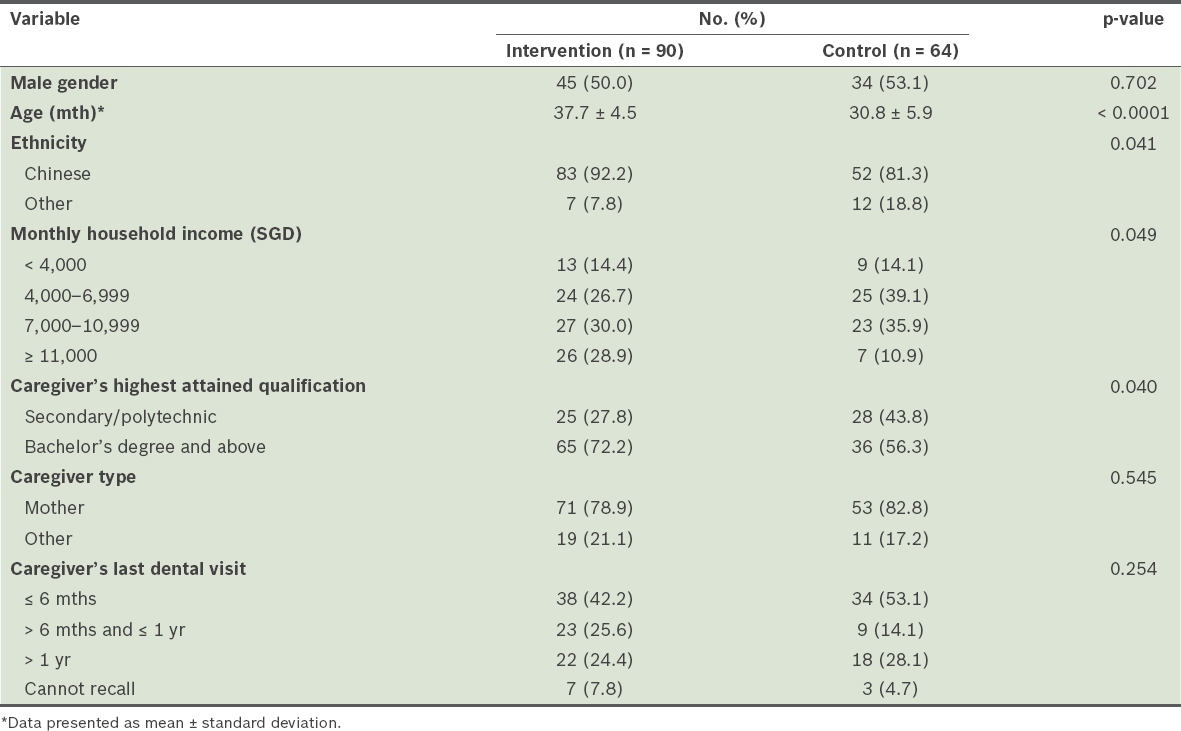
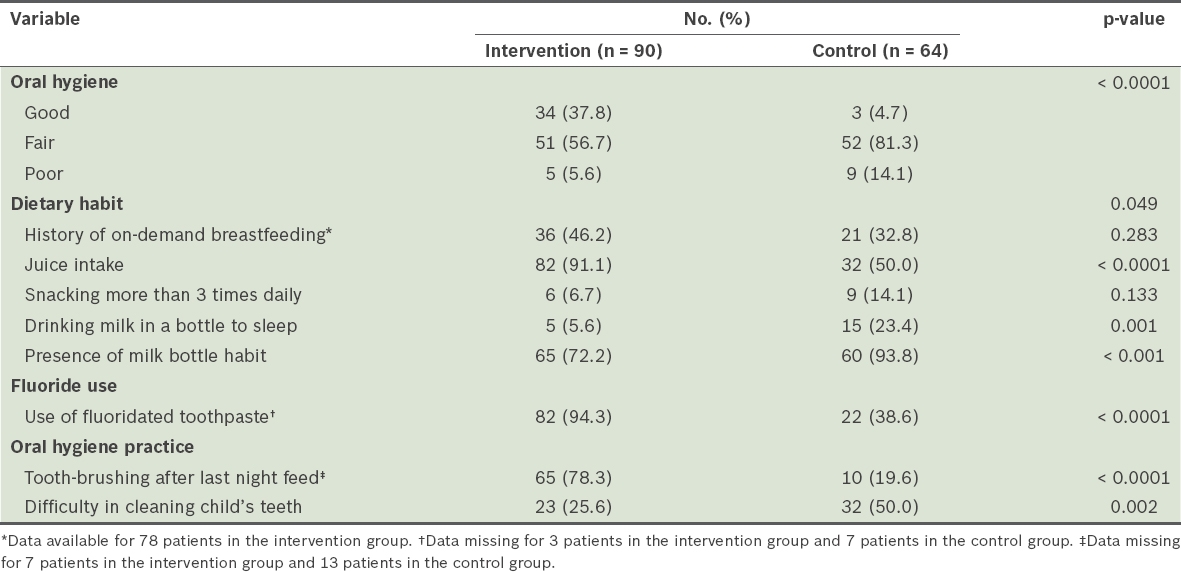
Compared to those in the intervention group, more children in the control group had habits associated with high caries risk, such as the presence of milk bottle habit and drinking milk to sleep (
Table II
Findings on oral hygiene and questionnaire responses.
31.3% of children in the control group had SECC compared to 7.8% in the intervention group (difference of 23.5%, 95% CI 11%–36%;
Table III
Outcome measures of the study.
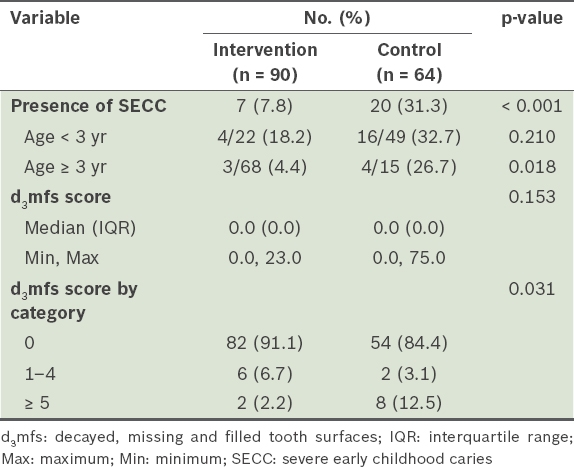
Table IV
Logistic regression analysis of severe early childhood caries.
DISCUSSION
There is a lack of clear evidence of the effectiveness of infant oral health programmes in different populations. In this exploratory study, we demonstrated that targeting infants and toddlers with oral preventive messages has the potential to significantly reduce caries prevalence. A 12-month cohort study of Singaporean preschool children(26) reported a caries incidence of 44%, as compared to our finding of 31.3% in the control group. In contrast, the 24-month caries incidence of 7.8% in our intervention group was significantly lower. Our findings showed that our two-year, customised, risk-based preventive oral health programme was successful in reducing SECC. This echoes the findings of previous studies.(15,17-22) Children who did not see a dentist at an early age were three times more likely to have SECC when compared to those who were enrolled in an infant oral health programme. This reinforces AAPD’s recommendation of the age one dental visit.
The slightly lower prevalence in the control group could be attributed to our study sample having caregivers with higher income and educational level, and a lower percentage of participants of non-Chinese ethnicity. Although the educational level of caregivers and the household income of the families in this study were generally higher than those of studies from other countries, the household demographic in terms of education and income resembled that of the overall Singapore population.(27,28)
The success of the oral health programme was also demonstrated by the maintenance of good oral hygiene practices and fewer high caries risk habits in the intervention group. While milk may be considered less cariogenic than other sugar-containing beverages,(29) formula milk often contains added sugar. In addition, it is a common practice here for caregivers to sweeten milk with sugar or honey to make it more palatable to children. Despite the repeated advice to avoid bottle-feeding during the dental visits, the percentage of children in the intervention group having a bottle-feeding habit remained high at 72.2%. Other studies have shown that not all children who had bottle-feeding habits exhibit SECC and not all children with significant dental caries had high-risk bottle-feeding habits.(30,31) Indeed, 72.2% of our patients in the intervention group continued to use the milk bottle after two years of preventive dental visits, but only 7.8% had SECC. Caregivers could have found it more challenging to get their children to give up the milk bottle compared to brushing the child’s teeth after the last feed. This is noteworthy for oral health providers, who should focus on changing modifiable behaviour that has the greatest impact on preventing caries. For example, 65.6% of caregivers in the control group used non-fluoridated toothpaste for their children. Considering that children’s toothpaste containing the desirable level of fluoride to protect against dental caries is widely available, the low number of children exposed to subtherapeutic levels of fluoride in their dentifrice was unacceptable. The use of toothpaste at the appropriate fluoride level according to caries risk should be emphasised.
Although dental caries is a preventable chronic disease, it remains prevalent in Singapore. Locally, awareness of the early preventive well-child visit is low among caregivers. Only 1% of parents were aware of the age one dental visit recommendation by AAPD.(8) In this study, children who had attended early preventive dental visits had a lower proportion and lower severity of dental caries compared to their peers who had not accessed dental care. Given the success of the early preventive dental visit in Singapore, the next step would be to engage and collaborate with professionals whom young children see on a regular basis. AAPD recommends the first dental visit by age one. At one year old, children typically have more frequent encounters with medical and early childhood professionals compared to dental specialists. The targeted professionals would be early childhood educators, infant care caregivers, paediatricians, primary health caregivers (e.g. general practitioners), family medicine physicians, and nurses in polyclinics who vaccinate infants and toddlers. While physicians and nurses have extensive training in various aspects of paediatrics, training in oral health may be inadequate or missing in the current training curriculum. Increasing oral health awareness in these groups could help identify high-risk children and enable timely referrals to paediatric dentists. This collaboration could potentially reduce the dental caries rate and encourage preventive oral health practices at an early stage, before surgical intervention is necessitated. Future directions may include the incorporation of a section on oral health in the curriculum for Family Medicine and Paediatric Residency, or an oral health assessment on the checklist when children attend medical clinics for their 12-month vaccinations.
We acknowledge several limitations of this study. Firstly, despite efforts to conduct recruitment from different sites in the country, it is likely that caregivers who were more motivated, and presumably had higher education level and household income, would have signed up for the study. Therefore, the results may not be representative of the general Singapore population and must be interpreted with caution. Although the household income for both the intervention and control groups was comparable, only around 14% of each group came from families with household income less than SGD 4,000. Children from the other ethnic groups and those from low-income families were few in this study. A previous study of Singapore children did not find any association between socioeconomic status and poor homecare practices, but noted the association of poor homecare practices with ethnic groups for health behaviours.(26) Despite the sample being skewed toward those of higher socioeconomic circumstance, 39.1% of children had SECC and 24.5% had dentinal caries at the end of our study across the two study groups. This suggests that dental caries is prevalent across all socioeconomic strata.
Secondly, it could be argued that the outcome measures in our study reflect the efficacy of fluoride varnish. Although the effectiveness of fluoride varnish in the prevention of dental caries has been proven,(13,14,32) we felt that the essence of the infant oral health programme was the identification of high-risk children and the appropriate preventive interventions that follow. Thus, we measured the effect of an infant oral health programme with its essential components intact and included the optimal exposure to fluoride, which we found in the study to be woefully inadequate.
Thirdly, there was an age discrepancy of seven months between the two groups as a result of the accumulative delay of review visits. However, the intervention group still showed lower disease level, which emphasised the effectiveness of our intervention. Although the interaction term between the treatment group and age was not statistically significant (p = 0.55), we should have considered measures to better match the two groups so as to control possible confounding variables related to age. This may include stricter dental review visit schedules or recruiting the control group at a time closer to the last dental review visit of the intervention group.
Considering the above limitations, future research should focus on the following areas: (a) the study could be repeated on a larger scale, with a population that is more closely matched to the existing racial compositions in the country, and include families with low socioeconomic status; (b) with the proven efficacy of the oral health programme in this exploratory study, the cost effectiveness of the programme could be evaluated; (c) since the children in the current study were seen by paediatric dentists, there is a need to look at the training of manpower in order for the infant oral health programme to be rolled out at a national level; (d) we should examine access to oral healthcare and target individual barriers to care, such as operational issues involving referrals and follow-ups; and (e) the oral health literacy of caregivers in Singapore and its relation to dental caries in children should be evaluated, as our study findings suggest that caregivers’ educational level may have an impact on overall preventive efforts.
In conclusion, the two-year preventive oral health programme for infants and toddlers was successful in reducing SECC when targeted behaviour modifications, such as reducing the consumption of sweetened milk and increased use of fluoridated toothpaste, were implemented. The result of this exploratory study provides preliminary clinical evidence for the training and allocation of manpower and the distribution of monetary resources for early caries prevention in children. It provides the basis for collaboration with medical and early childhood professionals, as well as the development of an infant oral health programme that can be tailored to the local population.
ACKNOWLEDGEMENTS
The authors would like to thank Ms Shen Guifeng and Ms Nurul Iryani for their administrative assistance; Dr Terry Teo and Dr Tabitha Chng for their assistance with data collection; and Miss Gita Krishnaswamy for providing the initial biostatistics consultation.


