Abstract
A 52-year-old man, who had a background of chronic heart disease and atrial fibrillation, as well as non-compliance with warfarin therapy, presented with a two-week history of worsening upper abdominal pain. Computed tomography mesenteric angiography showed complete embolic occlusion of the coeliac artery with resultant segmental splenic infarction, and thrombus within the left ventricle. A decision was made to proceed with catheter-directed thrombolysis. Subsequent follow-up angiogram at 12 hours showed successful treatment with complete dissolution of the coeliac embolus. The patient’s symptoms resolved during his hospitalisation and he was subsequently discharged well on long-term oral anticoagulation therapy. Isolated acute embolic occlusion of the coeliac axis is a rare occurrence that may result in end-organ infarction. Treatment options include systemic anti-coagulation, mechanical thrombectomy, catheter thrombolysis or open surgery. Catheter-directed thrombolysis therapy is a feasible and effective option for treating acute thromboembolic occlusion of the coeliac artery.
CASE PRESENTATION
A 52-year-old man presented to the emergency department with progressively worsening upper abdominal pain of one week’s duration. He was a heavy smoker with a history of chronic heart disease and atrial fibrillation, but was not compliant with his warfarin therapy. An echocardiogram performed two months before had shown a thrombus in the left ventricular apex and left atrial appendage.
The patient’s vital signs included a heart rate of 122 beats per minute (irregularly irregular), blood pressure of 123/68 mmHg, respiratory rate of 20 breaths per minute and oxygen saturation of 99% on room air. He was afebrile, alert and showed no signs of distress. Pertinent physical findings included a soft abdomen with moderate tenderness elicited in the epigastrium and left hypochondrium. There was no rebound tenderness, guarding or abdominal distension. Bowel sounds were present. The remainder of the physical examination was non-contributory. Bedside-focused ultrasonography showed no evidence of free fluid.
Initial laboratory results showed a mildly raised white blood cell count of 10.4 × 109/L and serum lactate level of 2.4 mmol/L (normal range 0.5–2.2 mmol/L). The patient’s liver function test results were mostly within normal limits (alanine aminotransferase 12 U/L, aspartate aminotransferase 21 U/L, bilirubin 24 µmol/L, alkaline phosphatase 97 U/L), with the exception of mildly raised gamma-glutamyl transpeptidase (GGT) (61 U/L, normal range 7–50 U/L). His international normalised ratio was normal, measuring 1.2.
Contrast-enhanced computed tomography (CT) of the abdomen was performed shortly after the patient was admitted. What do the CT images (Figs.
Fig. 1
Axial CT images in (a) arterial and (b) delayed phases through the upper abdomen.
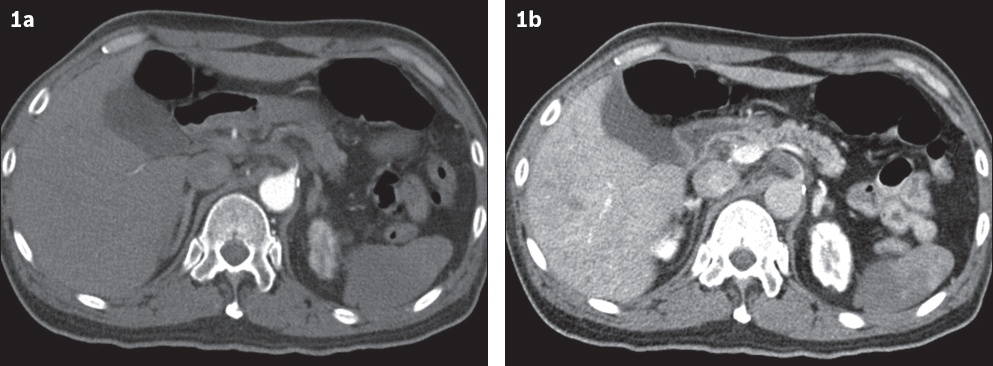
Fig. 2
Axial CT image at the level of the heart.
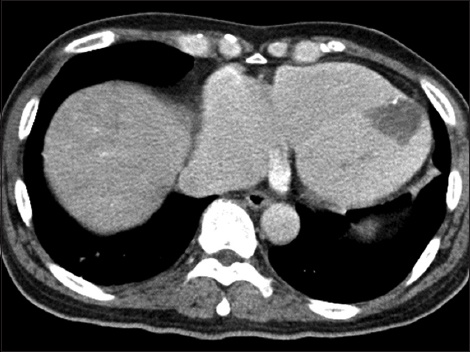
Fig. 3
Axial CT image through the upper abdomen.
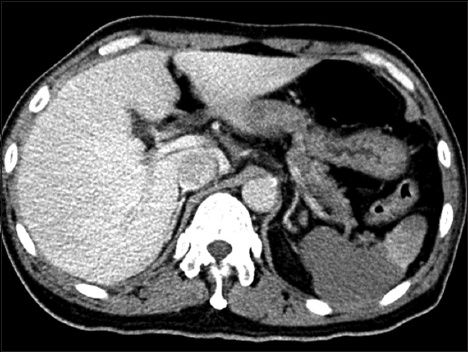
IMAGE INTERPRETATION
Axial CT images in the arterial (
DIAGNOSIS
Acute embolic occlusion of the coeliac artery.
CLINICAL COURSE
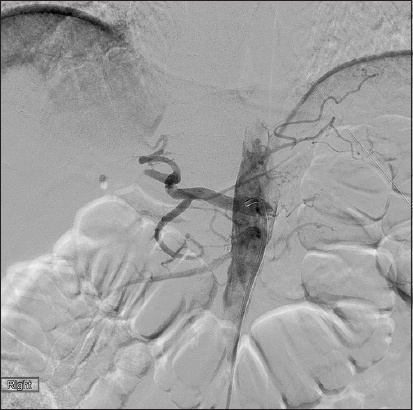
In view of the CT findings and progressively worsening abdominal pain, the decision was made to proceed with endovascular treatment of the coeliac artery after excluding any contraindication to thrombolysis. The right common femoral artery was punctured and an 8 French (Fr) vascular sheath (Terumo Medical Corporation, Tokyo, Japan) was inserted. A 5 Fr Simmons 1 (Terumo Medical Corporation, Tokyo, Japan) was used to cannulate the coeliac artery co-axially through a 7 Fr RDC (Vista Brite Tip; Cordis, Miami, FL, USA) guiding catheter (
Fig. 4
(a) Selective angiogram of the coeliac artery shows a filling defect within, extending into the common hepatic and splenic arteries; distal opacification of the hepatic artery proper occurs via retrograde flow through the superior mesenteric artery and gastroduodenal artery. (b) Angiogram of the coeliac artery shows that the guiding catheter was placed in the ostium of the coeliac artery with the thrombolysis infusion catheter positioned across the occluded segment.

During the course of the thrombolysis infusion, the patient’s abdominal pain had markedly improved, with a downtrending serum lactate level (2.0 U/L) and normalisation of the GGT level (50 U/L). The rest of the liver transaminases remained within normal limits. A subsequent follow-up angiogram at 12 hours (
Fig. 5
Repeat angiogram via the existing thrombolysis infusion catheter (not shown) and guiding catheter at 12 hours shows resolution of the thrombus with re-established flow within the coeliac artery. The splenic artery is not opacified and remains occluded.
In view of the presence of intrahepatic collateral flow in the right hepatic lobe, as well as improving clinical symptoms and lab results, it was thought unnecessary to further treat the migrated clot in the right main hepatic artery. Hence, the rtPA was discontinued, and the infusion and guiding catheters were removed. The groin sheath was removed two days later. The patient remained asymptomatic in the ward and was subsequently discharged on long-term oral anticoagulation therapy. At his clinic review six weeks after discharge, the patient was well with no further abdominal pain, and his liver transaminase and serum lactate levels were normal.
DISCUSSION
Acute coeliac artery occlusion, a rare cause of acute abdominal pain, has high mortality and morbidity when diagnosis and treatment are delayed. Besides cardiac disorders, such as atrial fibrillation, which can result in occlusion of virtually any artery, other causes that have been described in the literature by authors such as Tanaka et al,(1) Trellopoulos et al(2) and Arul et al included:(3) acute pancreatitis; recent upper gastrointestinal surgery; blood dyscrasias (e.g. antiphospholipid syndrome or thrombophilia); structural abnormalities such as compression by the median arcuate ligament; and oral contraceptive drugs. Most of these occlusions remain asymptomatic due to their gradual development as well as the vast collateral circulation from the SMA.(4) However, in cases of acute embolism, visceral and end-organ ischaemia may result in vague symptoms such as persistent abdominal pain, nausea and vomiting.
In cases of splenic infarction, which may occur in various clinical conditions, pain usually resolves gradually without clinical sequelae and surgery is required only when complications such as infection arise.(5) Gastric ischaemia is uncommon, as the stomach draws a rich blood supply from branches of both the coeliac artery and SMA collaterals, although one case report from Kelekis et al described gastric perforation secondary to atherosclerotic occlusion of both vessels.(6) Hepatic ischaemia is also uncommon, as the liver has a dual blood supply from both the hepatic artery and the portal venous system.
Imaging plays a crucial role when evaluating patients with suspected coeliac artery occlusion. Radiographs of the abdomen are usually unremarkable unless there are features of intestinal obstruction or perforation. Mesenteric CT angiography is accurate in depicting acute coeliac artery occlusion and its potential complications. A study of 26 patients showed that biphasic CT with mesenteric CT angiography was 100% specific, but only 73% sensitive in the diagnosis of coeliac artery, SMA and inferior mesenteric artery occlusion.(7) Intraluminal hypodensity within the coeliac artery, with non-enhancement of the distal vessels, would confirm the presence of an occluding thrombus or embolus. CT has the additional benefit of being able to detect anatomical variants such as a replaced right hepatic artery arising from the SMA, which may be crucial when planning for endovascular treatment (
Fig. 6
An elderly patient presented with massive upper gastrointestinal bleeding. (a) On selective cannulation of the coeliac artery, catheter angiogram shows opacification of the common hepatic artery (white arrowhead), splenic artery (black arrowhead) and gastroduodenal artery (white arrow). The right hepatic artery is not seen. (b) After cannulating the superior mesenteric artery (SMA), catheter angiogram shows a replaced right hepatic artery (black arrow) arising from the proximal SMA.
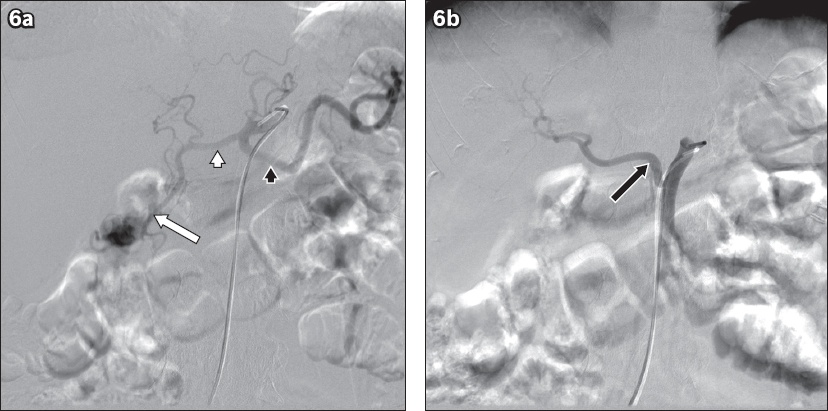
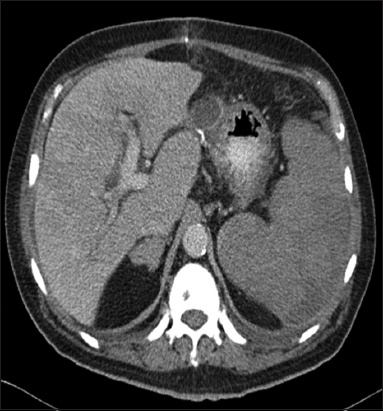
Fig. 7
A middle-aged man presented with upper abdominal pain and sepsis. Axial CT image shows marked enlargement of the liver and spleen with patchy areas of hypoperfusion, suspicious for hepatic and splenic infarction.
Angiography still remains the gold standard in the diagnosis of coeliac artery occlusion.(8) It has the additional benefit of supplying temporal information that allows the assessment of any collateral flow supplied from branches of the SMA. However, this imaging technique may not be suitable for all patients in the acute setting due to possible contraindications to catheter angiography, such as underlying coagulopathy or renal impairment.
Treatment options for acute coeliac artery occlusion vary between different centres. Possible options include endovascular treatment with catheter-directed intra-arterial thrombolysis, mechanical thrombectomy, systemic anticoagulation and open surgery. While endovascular treatment is infrequently described in the literature, it has been shown to have good results with a low incidence of complications, lower morbidity and a high technical success rate.(9)
In summary, isolated acute coeliac artery occlusion is a rare occurrence in patients with atrial fibrillation; when present, it can produce significant symptoms and result in end-organ infarction. Thorough preoperative imaging, including CT angiography, is very useful in assessing vascular involvement of the mesenteric vessels, as well as any potential complications. Catheter-directed intra-arterial thrombolysis is a feasible and effective method of treating acute thromboembolic occlusion of the coeliac artery.
SMJ-58-188.pdf


