Abstract
A 20-year-old National Serviceman presented with left knee pain and swelling after training for his physical fitness test. Lateral knee radiography and magnetic resonance (MR) imaging showed patellar tendon-lateral femoral condyle friction syndrome (PT-LFCFS), on a background of patella alta and patellar malalignment. The patient was treated non-operatively with a course of physiotherapy and given advice on rest and activity modification. PT-LFCFS is a less well-recognised but important cause of anterior knee pain and represents an entity in a spectrum of disorders related to patellofemoral instability. We herein discuss the MR imaging findings specific to and associated with this condition, as well as briefly describing treatment options. In addition, we showcase a range of commonly encountered abnormalities that affect the infrapatellar fat pad and briefly discuss their specific MR imaging findings.
CASE PRESENTATION
A 20-year-old National Serviceman presented with six weeks of left anterior knee pain and swelling after training for his individual physical fitness test. The pain was predominantly over the lateral aspect of his patella and was exacerbated by running and squatting for prolonged periods. There was also occasional clicking in the knee and the sensation of instability. Physical examination revealed tenderness over the lateral joint line and lateral patellar edge. Although there was full range of movement of the knee, pain was elicited at extreme flexion. Patellar grind test and lateral McMurray’s test were positive. What do the radiograph (
Fig. 1
Lateral radiograph of the left knee.

Fig. 2
(a) Axial and (b) sagittal fat-saturated proton density fast spin-echo and (c) axial proton density fast spin-echo MR images of the left knee.
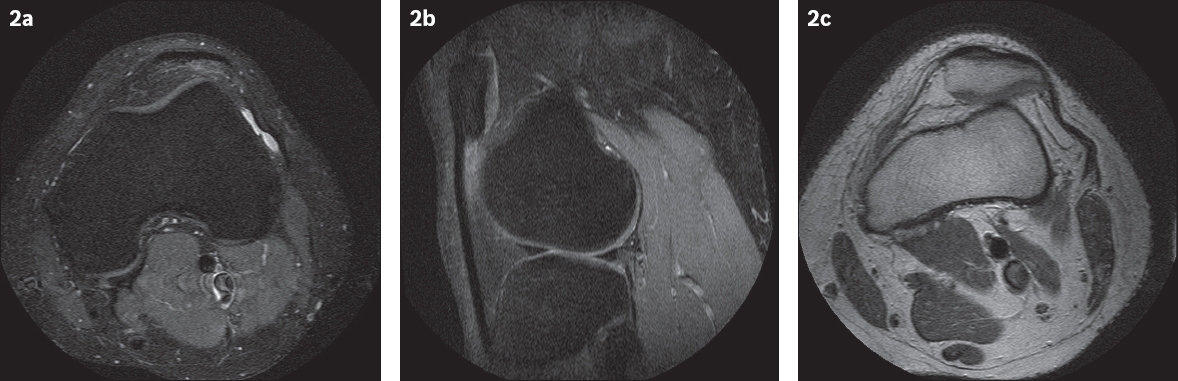
IMAGE INTERPRETATION
Lateral radiograph of the left knee (
DIAGNOSIS
Patellar tendon-lateral femoral condyle friction syndrome (PT-LFCFS) and patella alta.
CLINICAL COURSE
The patient was treated non-operatively with a course of physiotherapy and given advice on rest and activity modification. At his review six months later, there was reduced pain and he was able to run short distances with minimal discomfort.
DISCUSSION
Anterior knee pain is a common complaint among patients referred for MR imaging and remains a challenging problem to evaluate, diagnose and treat. This is in part due to the complex network of structures in the anterior knee compartment and the even more sophisticated system of interaction between them to achieve stable and balanced knee motion. Patellofemoral disorders are among the most frequently described sources of anterior knee pain,(1) but the precise mechanisms and predisposing risk factors that give rise to the development of pain are not yet fully understood.
Patellofemoral pain has been classified by the Lyon school into three well-defined entities(2) that describe a spectrum of disorders and their clinical manifestations relating to patellofemoral joint stability: (a) objective patellar instability (OPI), which is defined by the presence of at least one episode of true patellar dislocation or radiological sequelae and at least one anatomical abnormality confirmed by imaging, such as trochlear dysplasia, patella alta, patella tilt or tibial tubercle-trochlear groove (TT-TG) abnormality; (b) potential patellar instability (PPI), characterised by the presence of subjective patellar pain and/or instability (reflex) with no history of true patellar dislocation and the same anatomical abnormalities as in OPI; and (c) patellar pain syndrome (PPS), in which no major morphological abnormality is found on radiographs. The symptoms are a combination of patellar pain, reflex buckling and, sometimes, pseudolocking.
Transient lateral patellar dislocation and its MR findings have been discussed in a previous case in this Medical Education series.(3) We herein present a complementary case of PT-LFCFS that may fall within the definition of either PPI or PPS. PT-LFCFS is a less-recognised but important cause of patellofemoral arthralgia and an indicator of patellar maltracking and instability.(4) As such, recognition of this entity is important, as it has implications for both diagnosis and treatment.
PT-LFCFS is a form of impingement that occurs at the superolateral aspect of the infrapatellar fat pad between the patella and lateral femoral condyle, resulting in contusion and reactive inflammatory changes within the fat. When present, this manifests on MR imaging as focal increased signal on T2-weighted and fat-saturated images. The term was first used by Chung at el(5) in a retrospective study of 42 patients with chronic anterior and lateral knee pain. Although increasingly reported, this condition remains frequently overlooked and underreported in radiological literature.(6)
The infrapatellar fat pad is an intracapsular but extrasynovial structure that is bound by the patellar tendon anteriorly and the synovial-lined tibiofemoral joint posteriorly, with further posterior extension into the intercondylar notch. The fat pad is attached to the inferior surface of the patella superiorly and extends to the level of the cartilage overlying the anterior aspect of the femoral condyles posterosuperiorly. Inferiorly, it is attached to the periosteum of the tibia and the anterior horns of the medial and lateral menisci. The infrapatellar fat pad serves to increase the surface area of the synovium and facilitates the distribution of lubricant in the joint.(6) It receives its innervation from branches of the femoral, common peroneal and saphenous nerves, and is richly innervated by Type IVa free nerve endings, which transmit pain and inflammation, and is therefore a recognised source of anterior knee pain.
The typical presentation of PT-LFCFS is anterior knee pain inferior to the patella, which is exacerbated by knee extension. This is associated with focal point tenderness in the inferior patella. The fat pad is thickened on the affected side, resulting in difficult palpation of the patella.(5) Both signs and symptoms are non-specific, often generating a wide range of clinical differentials, such as patellofemoral stress syndrome, chondromalacia patellae, patellar tendinopathy and tear of the lateral meniscus.(1) This highlights the importance of MR imaging in the evaluation of patellofemoral arthralgia. On MR imaging, superolateral fat pad oedema appears to be a sensitive but non-specific sign for PT-LFCFS. In a study by De Smet et al,(7) this finding was present in all clinically symptomatic patients, although it was also seen in asymptomatic patients.
The presence of anatomical predispositions contributing to instability in patients raises the index of suspicion for PT-LFCFS. They include the presence of patella alta, patellar malalignment, a TT-TG distance of ≥ 20 mm and trochlear dysplasia. Assessment of these conditions was discussed in the aforementioned case earlier in this series.(3)
Following the diagnosis of PT-LFCFS, non-operative management is the mainstay of treatment, with rest, activity modification and ice as the essential components.(8) Anti-inflammatory drugs often help in the initial stages of treatment to reduce pain and inflammation and improve the patient’s compliance with physical therapy. Surgery is considered when conservative treatment fails to provide symptom control. The main techniques involve distal realignment, moving the tibial tubercle anteriorly and lateral retinacular release, all of which attempt to decrease the contact stresses between the patella and distal femur in the patellofemoral articulation.
PT-LFCFS is likely related to the clinical entity that has previously been called Hoffa’s fat pad impingement, described by Albert Hoffa in 1904. The latter is due to single or repetitive traumatic episodes with hyperextension and rotational forces causing haemorrhage. The inflamed fat pad then becomes hypertrophied, predisposing it to impingement between the tibia and femur, and thus, further injury and inflammation.(9) On MR images, acute findings indicate the presence of fluid, oedema and haemorrhage (
Fig. 3
A 30-year-old man sustained a twisting injury to the left knee. Sagittal fat-saturated proton density fast spin-echo MR image shows an acute shear injury of the infrapatellar fat pad (arrowheads). An accompanying complete tear of the anterior cruciate ligament (arrow) is noted.
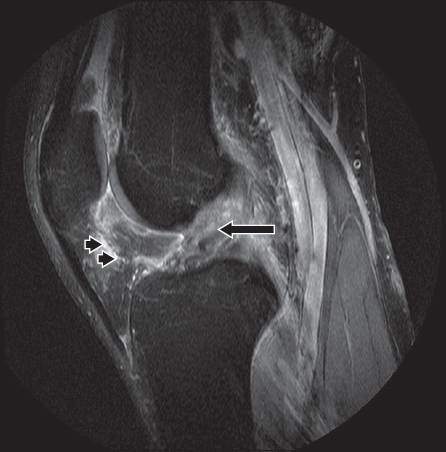
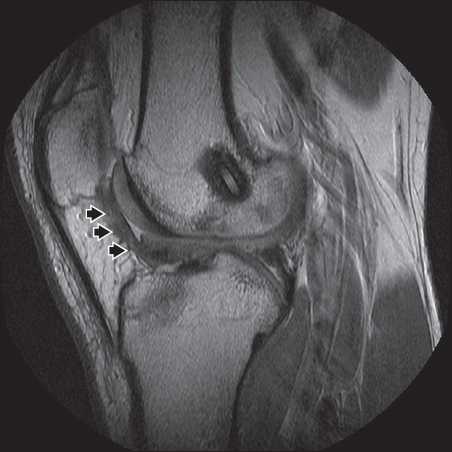
Fig. 4
A 21-year-old man who had prior anterior cruciate ligament (ACL) reconstruction presented with left knee locking. Sagittal fat-saturated proton density fast spin-echo MR image shows a prominent area of arthrofibrosis (arrowheads) anterior to the reconstructed ACL graft. Findings are related to chronic scarring due to the previous surgery.
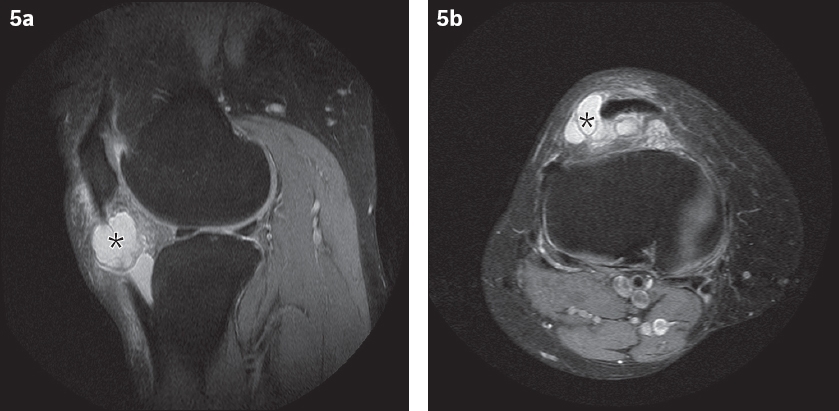
Several other entities that involve the peripatellar fat may be encountered when evaluating MR imaging of the knee. Cysts around the knee are common and those occurring within the infrapatellar fat pad may resemble Hoffa’s disease. Ganglion cysts arising in the infrapatellar fat pad were previously thought to be rare, with only a few having been reported in the literature (
Fig. 5
A 59-year-old woman presented with localised swelling at the lateral joint line of the right knee. (a) Sagittal and (b) axial fat-saturated proton density fast spin-echo MR images show a ganglion cyst (asterisks) involving the infrapatellar fat pad.
A parameniscal cyst is another intra-articular cystic lesion that has a similar appearance to a ganglion cyst and may involve the infrapatellar fat pad. It can be difficult to differentiate between the two, especially when the meniscal cyst arises from the anterior horn of the meniscus and extends into the infrapatellar fat pad. The clue to differentiation is the presence of a horizontal meniscal tear in the case of a parameniscal cyst (
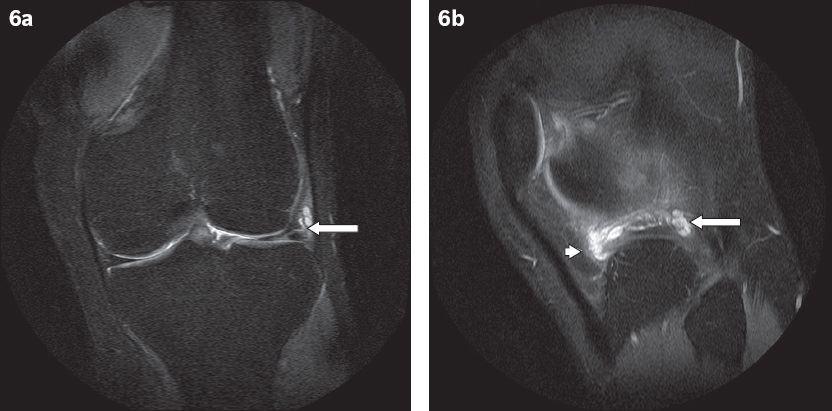
Fig. 6
A 22-year-old man presented with lateral joint line tenderness in the left knee. (a) Coronal and (b) sagittal fat-saturated proton density fast spin-echo MR images show a multiloculated parameniscal cyst related to a horizontal tear of the body of the lateral meniscus (arrows), which decompresses anteriorly toward the Hoffa’s fat pad (arrowhead).
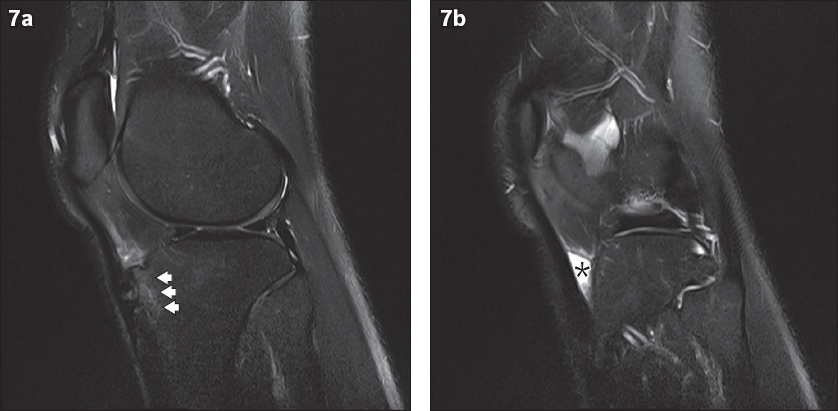
A further, not uncommon, abnormality to occur in the infrapatellar fat pad is deep infrapatellar bursitis, also known as retropatellar bursitis. Deep infrapatellar bursae are located between the distal patellar tendon and the anterior cortex of the proximal tibia. Small fluid collections in this area can be physiologic and are therefore considered to be normal. However, when there is pain and tenderness above the level of the tubercle or a palpable mass lateral to the distal patellar tendon, the diagnosis of infrapatellar bursitis should be considered. Deep infrapatellar bursitis usually results from overuse of the knee extensor mechanism, especially in runners and jumpers.(12) It has also been identified in patients with Osgood-Schlatter disease. In one study of such patients, a distended deep infrapatellar bursa was seen on MR imaging in 71% (12/17) of cases.(13) Deep infrapatellar bursitis is also associated with infection and inflammatory conditions. On MR imaging, it appears as a triangular fluid collection posterior to the patellar tendon (
Fig. 7
A 19-year-old man presented with pain at the anterior aspect of the knee. Sagittal proton density fat-saturated turbo spin-echo MR images show (a) fragmentation and increased signal intensity of the tibial tuberosity (arrowheads) compatible with Osgood-Schlatter disease, and (b) a triangular fluid signal collection deep to the distal patellar tendon (asterisk). This is the typical appearance of deep infrapatellar bursitis.
In conclusion, PT-LFCFS is a less well-recognised but important cause of anterior knee pain and represents an entity in a spectrum of disorders related to patellofemoral instability. It is also one of several conditions that affect the infrapatellar fat pad, with specific findings on MR imaging. Although the conditions are related based on the location of the disease, their imaging appearances are distinctly different, allowing differentiation of the abnormalities, which thereby enables the clinician to provide the necessary and appropriate care based on the correct diagnosis.
SMJ-59-182.pdf


