Abstract
An 82-year-old woman presented with neck pain and bilateral upper limb paraesthesia after sustaining an unwitnessed fall at home the day before. Physical examination revealed tenderness over the C4–6 region but no evidence of step deformity or neurological deficit. Magnetic resonance imaging of the cervical spine revealed multiple small fractures at the anteroinferior endplate corners of the C3, C5 and C6 vertebrae with focal kyphosis and marrow oedema at these levels, as well as associated disruption of the anterior longitudinal ligament and central spinal canal stenosis. The diagnosis of multiple flexion teardrop fractures was made based on these imaging findings, and the patient subsequently received conservative management. This paper illustrates the radiological features of flexion teardrop fractures and highlights the importance of prompt diagnosis and management of such cases.
CASE PRESENTATION
An 82-year-old woman presented to the emergency department with complaints of neck pain and bilateral upper limb paraesthesia. She had sustained mild injury to the left knee and neck after an unwitnessed fall at home the day before. Physical examination revealed tenderness over the C4–6 region but no obvious step deformity. Neurological examination of the limbs was limited by pain. Plain radiography of the cervical spine showed thickening of the pre-vertebral soft tissue and age-related degenerative changes, but no apparent fracture was seen. Subsequent computed tomography (CT) and magnetic resonance (MR) imaging were performed. What do the images (Figs.
Fig. 1
(a) Plain lateral radiograph of the cervical spine. (b) Unenhanced sagittal CT image of the cervical spine in bone window.
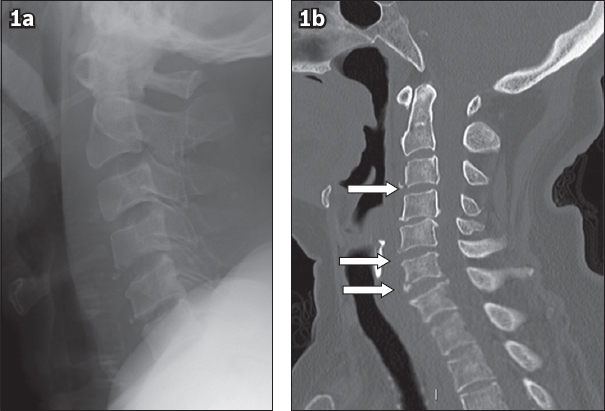
Fig. 2
Contiguous sagittal inversion recovery MR images of the cervical spine in (a) midline and (b) lateral view.
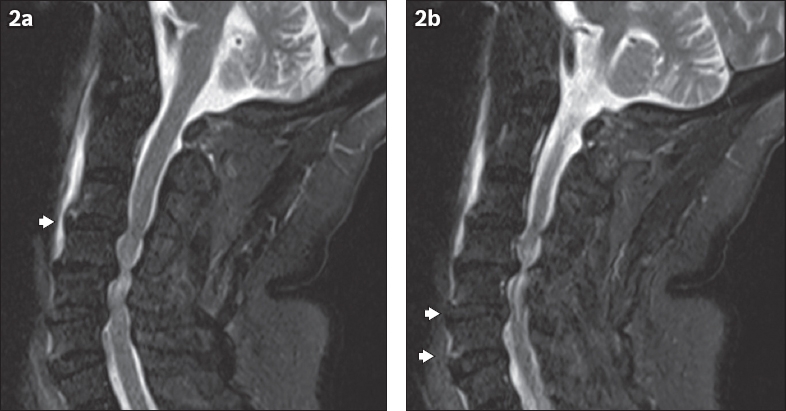
IMAGE INTERPRETATION
Lateral radiograph of the cervical spine (
DIAGNOSIS
Flexion teardrop fracture (FTDF).
CLINICAL COURSE
The patient was not suitable for surgical intervention in view of her multiple comorbidities. Thus, she was managed conservatively with an Aspen collar and physiotherapy.
DISCUSSION
FTDF of the cervical spine, originally described by Kahn and Schneider in 1956, derives its name from the characteristic triangular bony fragment (resembling a drop of water) that separates from the anteroinferior endplate corner of the cervical vertebral body.(1)
FTDFs represent forced hyperflexion of the cervical spine and axial compression at the anterosuperior aspect of the vertebral body culminating in oblique coronal vertebral fractures, which occur most commonly at the C5 level and less frequently at the C4 and C6 levels.(2) The involved vertebral body can be split coronally into two principal fragments. Associated retrolisthesis of the divided vertebral body into the spinal canal and disruption of the supporting ligaments result in marked instability at the level of injury.(3) Consequently, this particular type of fracture has the highest risk of neurological injury among all cervical injuries.(4) A majority of patients who present with FTDFs often have sustained high-energy traumatic injuries (e.g. from shallow water diving accidents and motor vehicle accidents), and a large number are quadriplegic at presentation.(3)
Diagnosis of FTDFs in an acute trauma setting is problematic, as movement of the cervical spine is prohibited in patients with spinal injuries and physicians are unable to accurately predict such injuries based solely on history and physical examination.(5) The combination of a potentially catastrophic injury and an inability to diagnose it clinically creates a conundrum, and herein lies the value of radiology.
Plain radiography is an excellent screening tool for cervical trauma in an acute setting when clinical suspicion is high. On the lateral view, the affected vertebral body is divided into two fragments: the anterior characteristic ‘teardrop’ fragment and the remaining posterior vertebral body. The anterior aspect of the anterior triangular fragment is, in most cases, aligned with that of the vertebral body below. A small proportion of these anterior fragments may be displaced beyond the anterior vertebral line. In all cases, however, the posteroinferior aspect of the posterior vertebral body fragment is displaced dorsally beyond the posterior vertebral line to varying degrees in relation to the vertebral body below.
Depending on the degree of subluxation of both fracture fragments, characteristic disruption of the supporting anterior and posterior ligamentous structures is seen. Consequential instability results in kyphotic deformity of the cervical spine at the level of injury. A study by Fuentes et al found that in cases where the kyphotic deformity is greater than 20°, there is often accompanying tetraplegia or anterior spinal cord injury.(6)
A series of compressive flexion injuries compiled and grouped into increasingly severe stages based on radiographic features by Allen et al indicates that the incidence of spinal cord injury ranged from 0% in the mildest category to 100% in the most severe.(7) Kim et al attempted to correlate radiographic features with neurological status and found similar results: 97% of cases exhibited neurological deficits in the setting of sagittal body or laminar fractures.(8)
CT (
Fig. 3
(a & b) Sagittal T2-W MR images of the cervical spine of a 64-year-old motor vehicular accident victim show disruption of the anterior longitudinal ligament as a result of a C4 flexion teardrop fracture (arrows denote the separate ends) with resultant pre-vertebral haematoma (arrowheads).
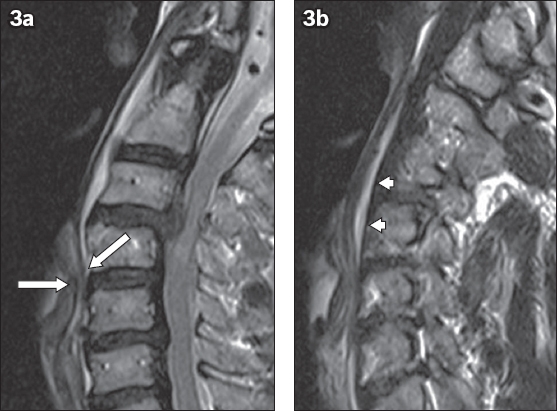
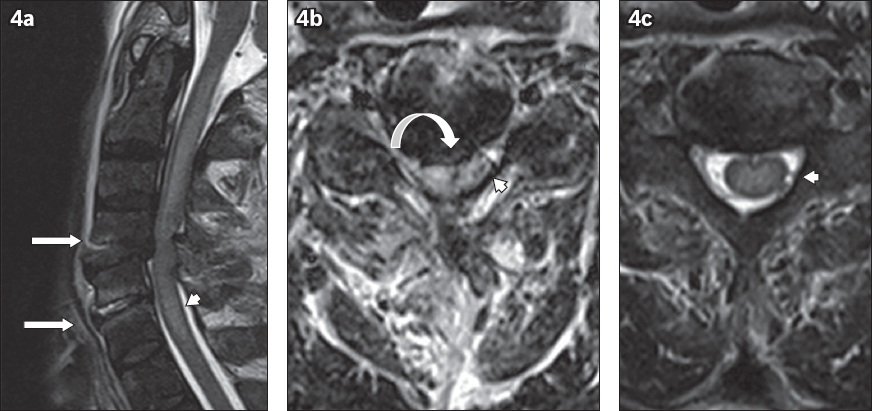
MR imaging is considered the gold standard in assessing the extent of injury to the spinal cord in blunt trauma.(9) Labattaglia et al suggested that the detection of MR abnormalities should determine changes to subsequent management.(10) Although MR imaging does not add significant value in the detection of unstable osseous injury that is not already evident on plain radiography or CT,(10) it is often employed in severe trauma due to its superior characterisation of injury to soft tissue structures, including pre- and paravertebral haematoma, supporting ligamentous disruption, post-traumatic intervertebral disc herniation, cord oedema and cord compression (
Analysis of the cervical spine fracture mechanism often requires understanding of radiographic appearances that characterise the end result of trauma. Careful correlation with clinical history and physical examination is therefore necessary due to the imaging similarities between FTDFs and other cervical injuries. Despite the recognised radiological features of FTDFs, diagnostic confusion may still arise between FTDFs and other types of cervical fractures with triangular fragments. For example, a hyperextension injury may produce an avulsed bony fragment at the anteroinferior corner of a vertebral body and disruption of the anterior longitudinal ligament, both of which appear similar to an FTDF. Distractive flexion injuries with sufficient axial compression may likewise produce equally misleading features.(3) Therefore, it is crucial to consider the clinical history, including injury mechanism and position of neck during such injury, in the evaluation of cervical spine trauma imaging, as shown by the Allen and Ferguson Classification.(7)
Fig. 4
(a) Sagittal T2-W and (b & c) axial MR images of the cervical spine of a 67-year-old man after an unwitnessed fall. As a result of a C4 flexion teardrop fracture, there is disruption of the anterior longitudinal ligament at C4–5 and C5–6 with periligamentous oedema and fluid tracking into the exposed intervertebral disc spaces (arrows). Heterogeneity and raised signal of the interspinous ligaments at these levels indicates associated injury. Compression of the spinal cord at the C5 level (curved arrow) secondary to the C4/C5 retrolisthesis with resultant cord oedema (arrowheads) is seen.
The main aims of treatment are to alleviate or reduce the risk of neurological deficit and to restore alignment of the cervical spine. Due to the inherent instability of FTDFs, surgery is the mainstay of management. Widely accepted surgical management for FTDFs includes complete excision of the affected vertebral body (corpectomy) with subsequent anterior cervical plate insertion. Fisher et al compared the outcomes of patients with unstable FTDFs who undergo surgery versus those who were managed conservatively (with thoracic halo vest), and found that surgical management is far superior in re-establishing and maintaining sagittal alignment of the cervical spine. This is further exemplified by the fact that 17% of patients who received conservative management initially went on to have operative treatment subsequently.(12) Another study by Kim et al found similar results and also demonstrated improvement in neurological status in those who received surgery.(13)
CONCLUSION
FTDFs are traumatic injuries to the cervical spine resulting from flexion-compression forces, and carry significant risk of bony instability and potential neurological damage. Imaging is indispensable for prompt diagnosis, and advanced imaging such as MR imaging is particularly advantageous in the identification of neurological injury. Nonetheless, careful correlation of radiological clues with clinical findings is needed – given the possible imaging similarities between FTDFs and other cervical injuries – to positively influence patient management and outcome.
SMJ-59-566.pdf


