Abstract
A 95-year-old woman presented with abdominal bloating and anorexia of one week’s duration. Contrast-enhanced computed tomography (CT) revealed features in keeping with gastro-gastric intussusception with a lead mass. Oesophagogastroduodenoscopy demonstrated a large 5-cm pedunculated fundal mass intussuscepted into the distal stomach. The patient subsequently underwent endoscopic polypectomy and open gastrostomy. Histological evaluation of the gastric mass revealed a gastrointestinal stromal tumour. Her postoperative course was uneventful. We herein describe the radiological features of adult intussusception and illustrate the usefulness of CT in the detection and characterisation of lead masses.
CASE PRESENTATION
A 95-year-old woman with a past medical history of hypertension and chronic kidney disease presented with abdominal bloating and poor appetite of one week’s duration. Physical examination showed conjunctival pallor and mild generalised abdominal tenderness without signs of peritonism. Blood tests revealed anaemia of 6.8 g/dL from a baseline level of 11.5 g/dL. Liver function tests and amylase were within normal limits.
Initial chest and abdominal radiographs were unremarkable. Contrast-enhanced computed tomography (CT) of the abdomen and pelvis (
Fig. 1
Contrast-enhanced (a) axial, (b) reconstructed coronal and (c) reconstructed sagittal CT images of the upper abdomen.
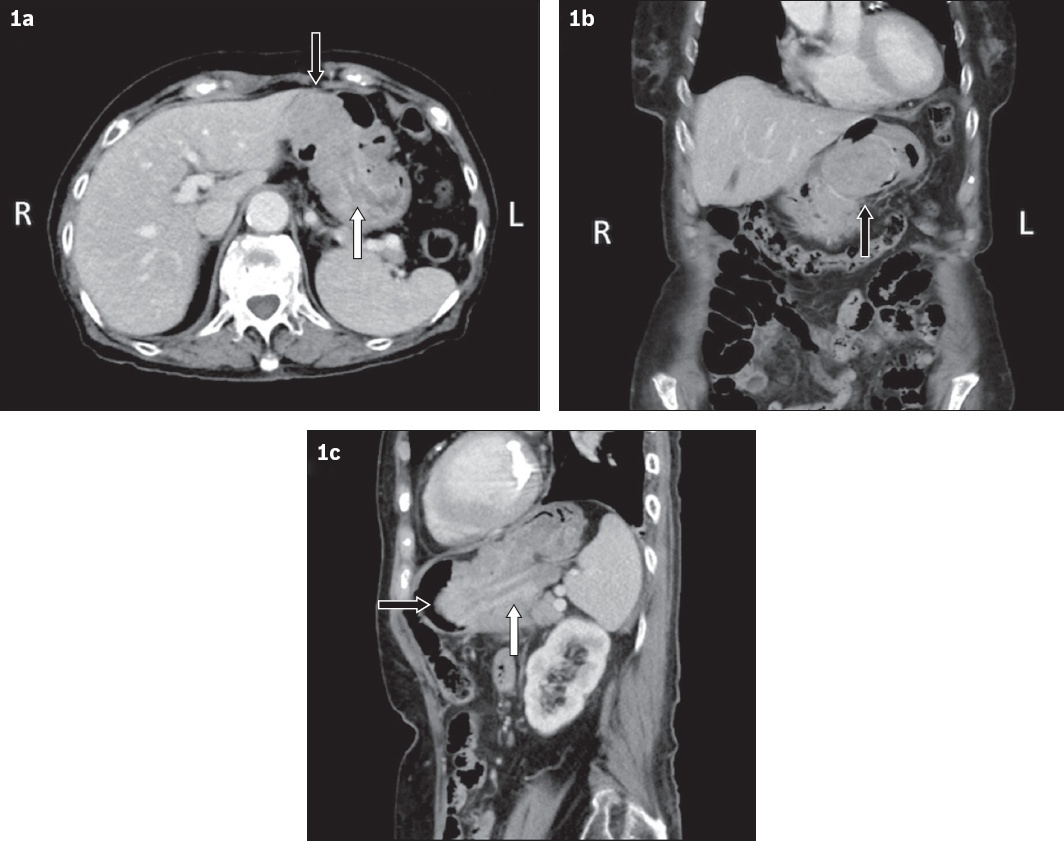
IMAGE INTERPRETATION
Contrast-enhanced CT images of the abdomen and pelvis show a well-defined, heterogeneously enhancing intraluminal gastric mass, measuring 5.5 cm × 3.8 cm, infiltrating the wall of the gastric fundus (black arrows,
DIAGNOSIS
Gastro-gastric intussusception due to gastric gastrointestinal stromal tumour (GIST).
CLINICAL COURSE
The patient subsequently underwent oesophago-gastroduodenoscopy, which confirmed gastro-gastric intussusception (Figs.
Fig. 2
Oesophagogastroduodenoscopic images show (a) gastro-gastric intussusception; (b) a polyp from the fundus; (c) the polyp after reduction; and (d) post excision.
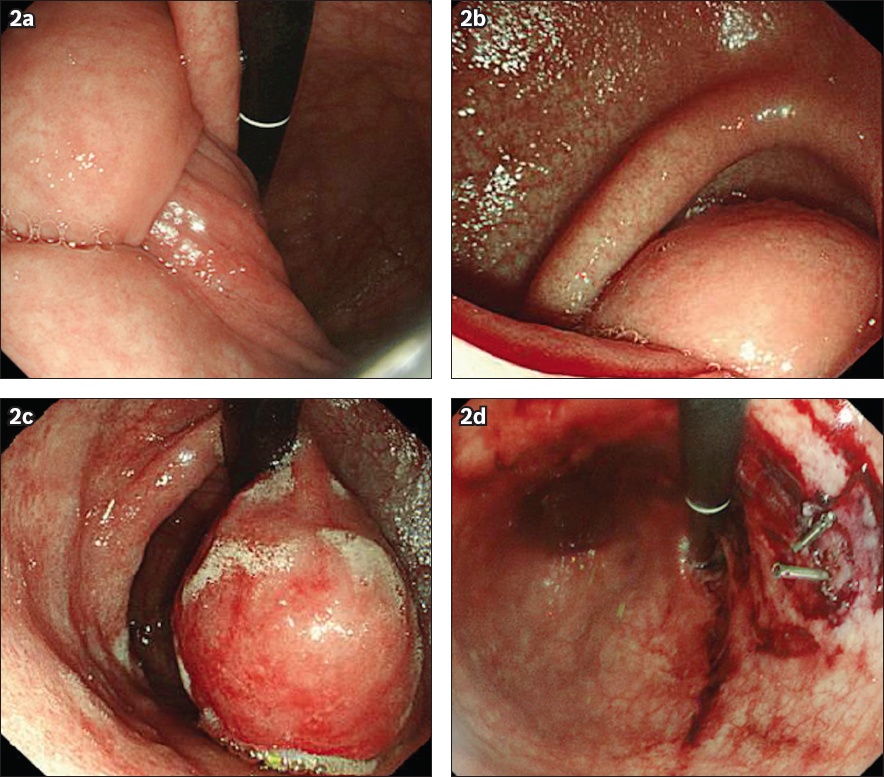
In view of the large size of the polyp and the patient’s relatively good premorbid status, the decision was made to perform endoscopic polypectomy with open gastrostomy. On endoscopic polypectomy, recurrence of gastro-gastric intussusception was noted (
DISCUSSION
Intussusception refers to the invagination of one part of the gastrointestinal tract into another, most commonly a proximal segment of bowel (intussusceptum) into a distal segment (intussuscipiens). Intussusceptions have been classified into four categories depending on their location: (a) entero-enteric, involving the small bowel only; (b) ileo-colic, with prolapse of the terminal ileum into the ascending colon and beyond; (c) colo-colic, involving the large bowel only; and (d) sigmoido-rectal, involving the sigmoid colon and rectum. The entero-enteric type is the most common, followed by the ileo-colic, colo-colic and sigmoido-rectal types. Foregut involvement, as described in the case above, is exceedingly rare and is not part of any anatomical classification mentioned in our review of the literature.
Gastro-gastric intussusception results from the invagination of the proximal stomach into the distal stomach. There have only been several published cases of gastro-gastric intussusception,(1-6) all of which have a gastric tumour as a lead point. The gastric tumours in question include primary gastric lymphoma,(1) gastric carcinoma(2) and hypertrophic gastric polyps.(3) Only two cases of gastro-gastric intussusceptions due to leiomyomas(4,5) and one due to a GIST(6) have previously been reported.
Adult intussusception is much more rare than its paediatric counterpart, accounting for only 5%‒10% of all cases of intusssuceptions(6-8) and 1%‒5% of bowel obstruction in adults.(7) In contrast to paediatric intussusception, which classically presents with the triad of abdominal pain, mass and per-rectal bleeding, the clinical presentation of intussusception in adults is usually non-specific. The most common presenting symptoms include abdominal pain, nausea and emesis in the acute setting, and intermittent abdominal pain and vomiting in the subacute or chronic setting.(9) Given the often-vague presenting symptoms, imaging investigations are of value in the evaluation of adult patients with suspected intussusception.
Abdominal radiographs, which are typically the first imaging investigation obtained, may be useful in demonstrating signs of intestinal obstruction and providing information regarding the site of obstruction. Contrast fluoroscopic studies, namely upper gastrointestinal contrast series for foregut/small bowel involvement and barium enema for large bowel involvement, may show a classic ‘coiled spring’ appearance.(4,5)
Ultrasonography is a frequently employed modality for diagnosing intussusception, especially in the paediatric population, although it is also used in adults. Classic sonographic features include the ‘target’ sign on the transverse view and the ‘pseudo-kidney’ sign on the longitudinal view.(7) The limitations of ultrasonography include its operator dependency and certain patient factors such as gaseous bowel distension, which may limit image quality and diagnostic accuracy.(7)
CT is currently considered the most useful and sensitive modality to diagnose intussusception in adults, with a reported diagnostic accuracy of 58%‒100%.(7,8,10,11) Characteristic CT features are well documented, such as the ‘target’ or ‘sausage’ sign and invagination of mesenteric fat and vessels within the bowel lumen.(7) Unlike ultrasonography, CT is not affected by the presence of gas in the bowel.(8) CT can also help to define the location and nature of the lead mass and its relationship to the surrounding tissues.(8,12) In addition, other findings such as the presence of lymphadenopathy or metastasis may also be detected in the setting of an underlying malignancy.(7,8)
Adult intussusception is usually caused by a structural lesion acting as a lead mass,(6-8) as opposed to intussusception in children, which is usually primary and benign.(7) It is believed that the presence of a lesion in the wall of the gastrointestinal tract alters normal peristaltic activity, initiating the invagination, with subsequent peristaltic activity causing further telescoping of the lead point.(8-11)
One of the most common benign lead masses in adult intussusception is a lipoma (
Fig. 3
(a) Coronal and (b & c) axial CT mesenteric angiograms of a 70-year-old man show a predominantly fatty mass in the descending colon lumen (black arrows). Proximal colonic intussusception is noted, with the entry point at the level of the splenic flexure (white arrow). Following left hemicolectomy and omentectomy, histology revealed a submucosal lipoma.
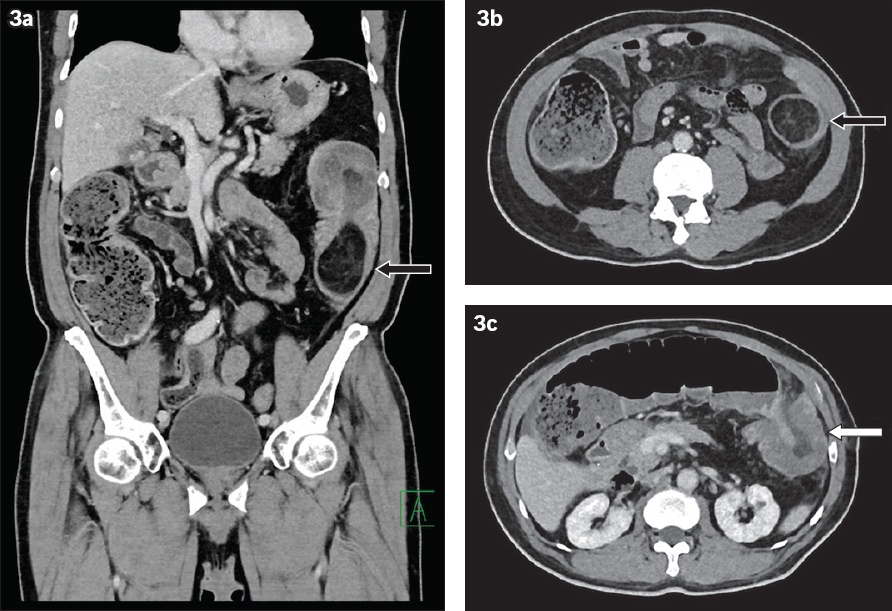
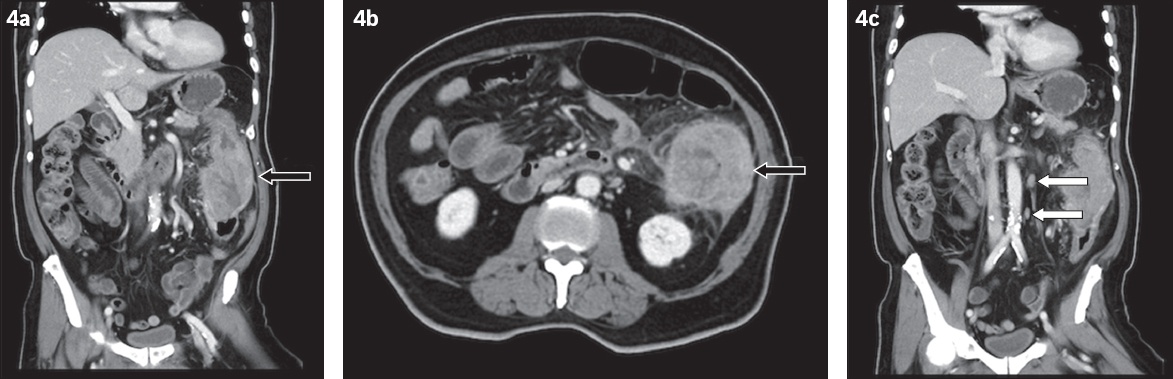
Fig. 4
(a & c) Coronal and (b) axial contrast-enhanced CT images of the abdomen and pelvis of an 84-year-old man show a long segment of diffuse irregular thickening along the descending colon with colocolic intussusception (black arrows). Enlarged para-aortic lymph nodes are also seen (white arrows). Following subtotal colectomy, histology revealed moderately differentiated adenocarcinoma.
Underlying gastrointestinal polyposis syndromes must be considered when an adult patient presents with suggestive clinical features in addition to intussusception (Figs.
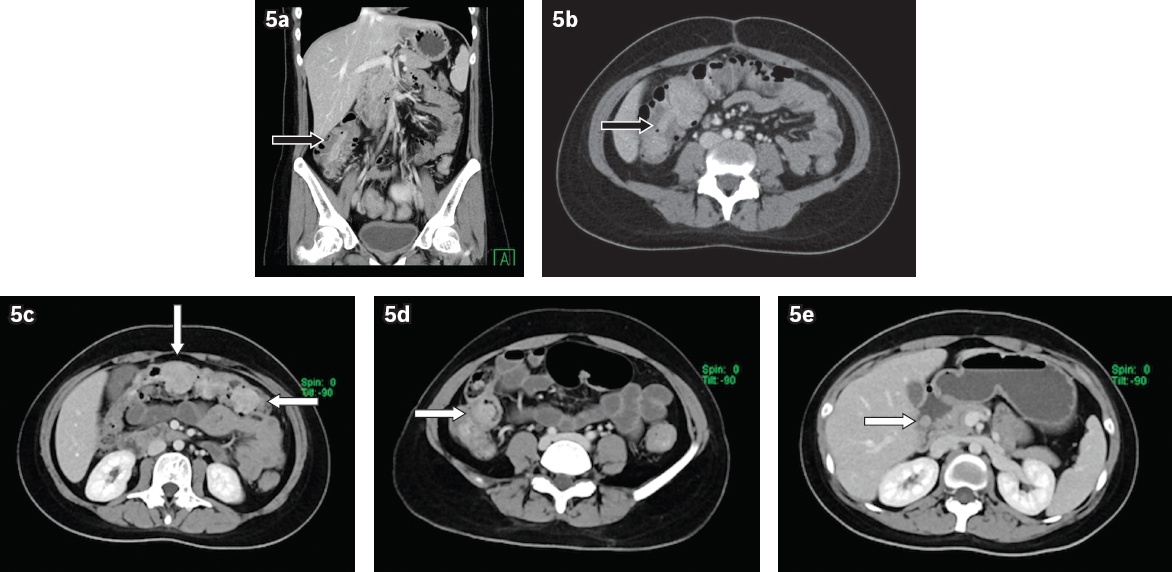
Fig. 5
(a) Coronal and (b) axial contrast-enhanced CT abdomen and pelvis of a 25-year-old woman shows a bowel-within-bowel configuration in the ascending colon, raising suspicion of an ileo-colic intussusception (black arrows). (c‒e) Subsequent axial contrast-enhanced CT enterography shows multiple polypoidal lesions in the small and large bowel loops (white arrows), in keeping with the hamartomatous polyps of Peutz-Jeghers syndrome. The patient underwent subtotal colectomy with jejunal and duodenal enterotomy for polypectomy.
In conclusion, intussusception in adults is difficult to diagnose preoperatively because it usually presents with nonspecific symptoms, as in this case. A high index of clinical suspicion may be required. The characteristic features of intussusception on CT makes CT a good modality for the evaluation and confirmation of intussusception, including the involvement of unusual sites such as the foregut, as well as for identifying lead masses and excluding other sinister pathology.
SMJ-61-74.pdf


