Abstract
INTRODUCTION:
Inappropriate attendances (IAs) at emergency departments (ED) are contributed by patients with mild or moderate medical conditions that can be effectively managed by primary care physicians. IAs strain limited ED resources and have an adverse impact on efficiency. This study aimed to identify factors associated with IA at the ED of a tertiary hospital in Singapore.
METHODS:
We conducted a retrospective cohort study of all eligible visits to the aforementioned ED between 1 January 2015 and 31 December 2015. The appropriateness of each attendance was estimated using criteria based on investigations or procedures that were performed on the attendee and the discharge type of that attendance. IAs were then compared against appropriate attendances in these areas: attendee demographics; referral source; time of ED visit; proximity to ED and 24-hour general practitioner clinics; and history of ED visits in 2014. Multivariate analysis was performed on significant variables associated with IAs.
RESULTS:
Among 120,606 attendances, 11,631 (9.6%) were IAs. Multivariate analysis showed that gender, ethnicity, referral source, time of ED visit, nationality and history of frequent visits to the ED were factors associated with IAs. Moreover, the odds of IA were found to be higher among attendees who were younger, were self-referred, or had at least one IA in 2014.
CONCLUSION:
This study identified subgroups in the population who were more likely to contribute to IAs at the ED. These findings offer relevant insights into future research directions and strategies that might potentially reduce avoidable IAs.
INTRODUCTION
Crowding is defined by the American College of Emergency Physicians as a situation where “demand for emergency services exceeds available resources for patient care in the emergency department (ED), hospital, or both.”(1) Crowding is an undesirable phenomenon, as it can compromise the quality of care to ED patients, which may in turn have an adverse impact on their health outcomes.(2-5) Studies have shown that ED crowding is detrimental to the morale,(6) productivity(2,7) and training(8) of ED staff. Over the years, the problem has grown and is affecting the healthcare systems in many countries, including developed countries such as Australia, the United Kingdom and the United States.(9-12) Given the prevalence of ED crowding across the world, studies(13-18) that are pertinent to understanding its causes or identifying measures that can potentially alleviate ED crowding have received a lot of attention from the research community.
One reported mitigating measure for ED crowding(17-20) entails managing the demand for an ED from patients whose medical conditions do not warrant an ED visit; such visits are commonly known as inappropriate attendances (IAs). Patients who visit EDs inappropriately are usually those with low urgency health problems that are unlikely to require admission and more suitably seen by a primary care physician (PCP). In a crowding situation, such patients utilise limited ED resources, and this may hinder ED physicians from treating other patients who require emergency medicine service in a timely and safe manner.
In general, an ED visit is classified by researchers as an IA if the patient involved could be adequately treated in a primary care setting.(20,21) However, there is no consensus(22-24) among the research community and policymakers on the methodologies for classifying ED visits as either appropriate or inappropriate. For example, IA classification may be prospectively performed(22) in triage areas of ED and based on somatic complaints and/or vital sign collection. Alternatively, such classification may also be retrospectively performed(22) based on the diagnosis, results of tests obtained during the ED visit and hospital admission. As a result, there is wide variability(22) in the reported estimation of IA prevalence (4.8%‒90%).
In Singapore, there is a dearth of research on IAs at EDs. This study aimed to fill the current research gap in two major ways. First, it sought to estimate the extent of IAs at an ED in a local restructured hospital in Singapore using a pragmatic and objective approach to defining IA. Second, we aimed to identify the factors associated with IAs at this ED.
METHODS
This was a retrospective cohort study that analysed variables extracted from the administrative databases of the Accident and Emergency Department (A&E) at Changi General Hospital (CGH), Singapore. The study population included all CGH A&E attendances occurring between 1 January 2015 and 31 December 2015, excluding patients who left without being seen, were discharged against advice, absconded or were dead on arrival, as well as CGH staff, referrals by the Singapore Prison Service and Singapore Police Force, and Singapore Armed Forces (SAF) personnel. All 18-year-old male Singapore citizens and permanent residents are required statutorily to undergo two years of compulsory service in the uniformed services, with the majority of them in the SAF. Existing financing policy allows SAF personnel to visit the EDs of public hospitals in Singapore without requiring them to pay A&E attendance fees. A study has found that the odds of IA among attendees who did not pay for ED consultation were higher than among those who did.(25) Since SAF personnel contributed to about 7.0% of the annual CGH A&E workload and their health-seeking behaviour could be different from other attendees, ED attendances contributed by SAF personnel were also excluded from our study population. Ethics approval to conduct the study was given by the SingHealth Centralised Institutional Review Board.
Attendances that were included in the analysis were divided into two groups for comparison, namely appropriate attendances (AAs) and IAs. In our study, an ED attendance was considered an AA if one or more of the following conditions were met: the attendee (a) required investigation tests (i.e. laboratory or radiological tests) during the visit; (b) underwent procedures such as intravenous drip, dressing or minor surgical procedures; (c) was admitted to an inpatient ward; (d) was admitted to the short-stay unit, a ward for observation for up to 23 hours of ED patients who have specific clinical conditions and do not require inpatient admission; (e) was referred for follow-up at a specialist outpatient clinic after discharge from the ED; or (f) was referred to the ED of other hospitals. If the ED attendance did not meet any one of these criteria, it was classified as an IA. Since early 2014, CGH A&E has been using the aforementioned set of administrative criteria to classify the appropriateness of general practitioner (GP) referrals. In a recent study,(26) this retrospective classification of ED attendances based on the same criteria was found to be consistent with the opinions of senior A&E physicians in CGH after they had reviewed the medical records of the sampled attendances.
We compared the two groups of attendances in terms of patient demographics (e.g. age, gender, race and nationality), referral source, time of ED visit, proximity to the CGH A&E, proximity to private 24-hour GP clinics, and history of ED visit in the preceding year. Ethnicity was categorised into four main groups, namely Chinese, Malay, Indian and others. Referral sources of attendances were also classified into four main groups, namely PCP, ambulance-conveyed, other healthcare institutions (i.e. community hospitals, dialysis centres, national specialist centres or nursing homes) and self-referred. Referrals by PCPs included those made by GPs and doctors at polyclinics, while ambulance-conveyed cases were attendees brought to CGH A&E by public or private ambulances. In terms of the time of the ED visit, attendances were classified into whether the attendee had arrived at the ED during the normal GP clinic operating hours of 9 am‒9 pm or outside of those hours.
In our study, proximity was measured as the shortest driving distance between the attendee’s residential address and the ED or the nearest 24-hour GP clinic. Based on the residential addresses of ED attendees, and the addresses of the CGH A&E and 24-hour GP clinics, every shortest driving distance was calculated using the API (application programming interface) of OneMap,(27) a local integrated map system developed by the Singapore Land Authority. Using the relevant CGH A&E attendance records in 2015, the median driving distance of the attendees to the CGH A&E was computed. Attendees residing within this median driving distance to CGH A&E were then compared against the rest. Similarly, attendees residing within this median driving distance of their respective nearest 24-hour GP clinics were also compared against the rest. The addresses and operating hours of all GP clinics in Singapore were based on online information made available by Singapore Health Services.(28) ED visit history included information pertinent to whether the same attendee had at least one IA or was a frequent ED visitor in the preceding year. To be considered a frequent ED visitor in a calendar year, an attendee needed to have four or more ED visits in the same calendar year.
Data analysis was performed using IBM SPSS Statistics version 19.0 for Windows (IBM Corp, Armonk, NY, USA). Using univariate analysis, the two groups of attendances were compared by first identifying the variables that were significantly different. The level of statistical significance was set at p < 0.01. Multivariate logistic regression was then performed to study the combined effects of the identified significant factors. The backwards model selection method was employed, with the significance level also set at p < 0.01.
RESULTS
After applying the exclusion criteria described earlier, 126,796 attendances were seen at CGH A&E from 1 January 2015 to 31 December 2015. As 6,190 of these attendances did not have complete information for analysis due to missing values (e.g. race or postal codes) or entry of invalid postal codes (i.e. those not indexed by OneMap), they were excluded from our study. Of the remaining 120,606 eligible attendances, 11,631 (9.6%) were found to be IAs. The demographic characteristics of AAs and IAs that were included in the study are shown in
Table I
Demographic characteristics of attendances included in the study (n = 120,606).
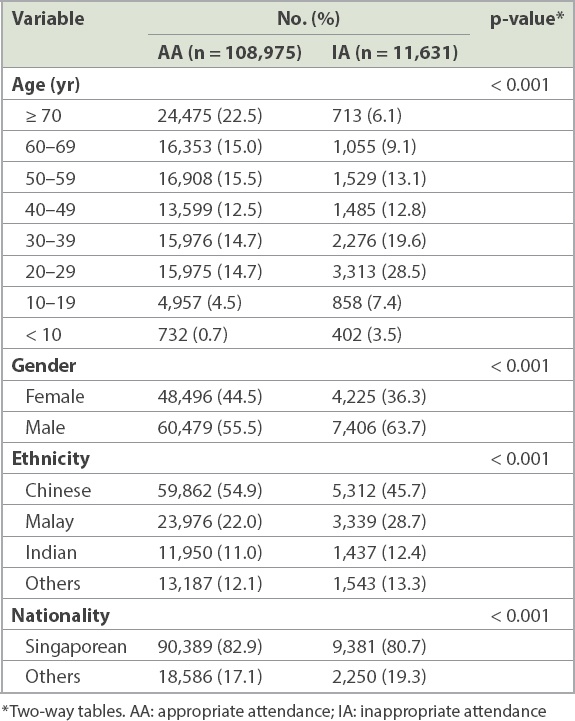
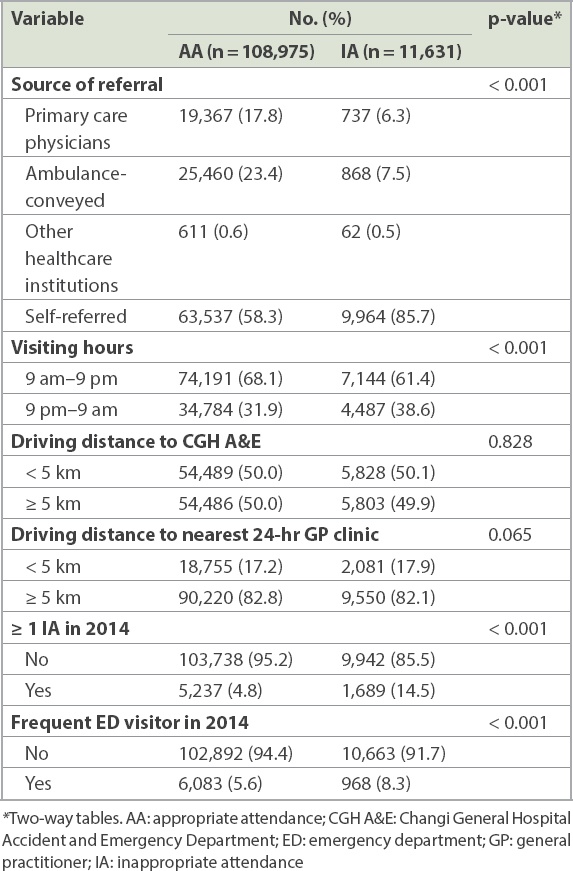
Table II
Other characteristics of attendances included in the study (n = 120,606).
In the multivariate analysis, all the aforementioned factors remained significant (
Table III
Results of multivariate analysis (n = 120,606).
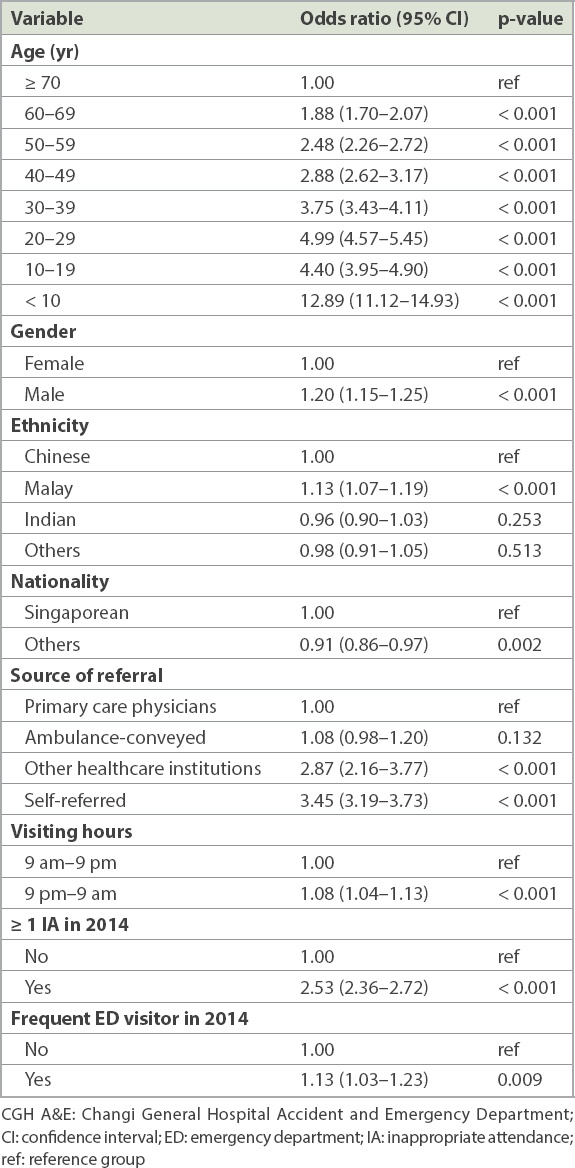
Unlike the aforementioned three factors that increased the odds of IA by 1.88 times or more, four other factors increased the risk of IA by 8%‒20%: being male (odds ratio [OR] 1.20; p < 0.001) compared to female; being Malay (OR 1.13; p < 0.001) compared to Chinese; visiting the ED between 9 pm and 9 am (OR 1.08; p < 0.001) compared to visiting between 9 am and 9 pm; and attendees who were frequent ED visitors in 2014 (OR 1.13; p = 0.009) compared to those who were not. Conversely, non-Singaporean attendees had a lower risk of IA (OR 0.91; p = 0.002) compared to Singaporeans.
DISCUSSION
In the present study, it was estimated that 9.6% of attendances at the CGH A&E in 2015 were deemed inappropriate. This proportion, which was similar to that reported in a recent study of ED attendances in England,(20) offered a favourable opportunity for CGH to address the ED crowding problem via measures to reduce avoidable IA.
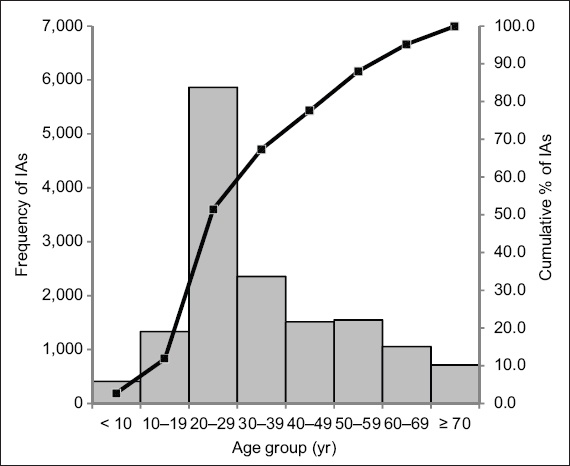
We noted in our multivariate analysis that attendee age has a strong relationship with IAs, with the odds of IA increasing from the oldest age group to those aged 20‒29 years. However, the odds decreased slightly in the next younger age group (10‒19 years) before spiking (OR 12.89) in the youngest age group (< 10 years), a similar trend seen in other studies.(20,29-31) Some factors that were reported to be associated with IAs among children included: the lack of a continuous relationship with PCPs;(32) caregivers overestimating the severity of their children’s illness; caregivers having had prior experience of being taken to the ED as children; being a single parent with no other adults living in the household;(33,34) availability of after-hour care offered by the ED; and mistrust of the PCP’s ability to manage paediatric conditions.(35) However, there are limited studies on factors associated with IAs specifically among attendees in the 20‒29 years age group, which contributed 28.5% of all IAs at the CGH A&E in 2015. In our study cohort, 39.3% of IAs were younger than 30 years of age (
Fig. 1
Chart shows age distribution of patients with inappropriate attendances (IA) at Changi General Hospital’s Accident and Emergency Department in 2015.
Unlike PCP-referred attendees, self-referred attendees did not seek the advice of qualified doctors on their respective medication conditions prior to their visits to the CGH A&E. Hence, it was not surprising that the odds of IA among self-referred attendees were higher than those among PCP-referred attendees. However, the higher odds of IA among self-referred attendees (OR 3.45, p < 0.001) and the fact that a large proportion of the IAs were from this group (85.7%) could indicate the practical value of further studies to understand the main contributing factors to IAs among this group. It is also interesting to note that the odds of IA among attendees referred by other healthcare institutions were 2.87 times (p < 0.001) that of PCP-referred attendees. Thus, there may be room for improvement in ED referral processes among these healthcare institutions, which could potentially help to reduce IAs at EDs.
Our finding of significantly higher odds of IA among attendees who had at least one IA in the preceding year, compared to those who did not, was similar to the finding reported in another study.(29) This appeared to suggest that future avoidable IAs may be reduced by aiming IA reduction efforts at known attendees who were known to have previous IAs. Moreover, our results also showed that those with a history of frequent ED visits in a year appeared to have high odds of IA in the following year. Thus, the past visit history of ED attendees could be used to identify individuals who are likely to visit the ED inappropriately again in future, while IA reduction efforts could be streamlined to target these attendees.
Interestingly, 61.4% of IAs in our study cohort took place during hours when PCPs were more readily available (i.e. 9 am‒9 pm). Our univariate analysis also showed that proximity to a 24-hour GP clinic was not a significant factor associated with IA. Logistic regression indicated that attendees who visited the ED at 9 pm‒9 am had a marginally higher risk of IA (OR 1.08; p < 0.001) than those who visited the ED at other hours. This appeared to suggest that the higher odds of IA among attendees visiting the ED at 9 pm‒9 am might not be due to the lack of 24-hour GP clinics. This observation was consistent with a study reporting that increased access to and availability of alternative sources of primary care did not reduce avoidable IA.(36) Potentially, other factors such as lack of knowledge about what constitutes an appropriate ED visit, lack of awareness of nearby 24-hour GP clinics, mistrust of the ability of PCPs, lack of onsite ancillary facilities such as laboratory testing and radiography facilities at GP clinics, and the high consultation costs of PCPs could be contributing to the marginally higher odds of IA among patients who visited the ED at 9 pm‒9 am.
To date, several studies(17-18) have been performed to evaluate the effectiveness of various interventions that aimed to reduce ED utilisation, including efforts pertinent to IA reduction. As highlighted by a recent systematic review,(17) these IA reduction interventions can be broadly classified into three main types, namely primary care linkage, ED diversion, and financial penalties or cost-sharing. Primary care linkage refers to programmes(37,38) aimed at IA reduction via strengthening the population’s linkages to primary care networks and/or providing care coordination of ED attendees with PCPs. On the other hand, ED diversion involves interventions that aim to direct patients with IAs away from the ED either before or at the time of ED triage. For example, IA can potentially be diverted prior to ED triage using a 24-hour hotline such as that offered by the United Kingdom’s National Health Service (NHS), NHS-111, in which a trained hotline team advises callers from the public whether they have a clinical need to visit the ED and what alternative local healthcare services are available if they have no clinical need to visit the ED. A post-ED triage diversion programme(39) for ED patients with low-acuity complaints was also reported by an ED of a hospital in the United States: eligible patients were referred to either an onsite primary care clinic in the same hospital or the usual care in the ED, depending on which option would result in the least delay for the patients. Finally, financial penalties or cost-sharing programmes(40-42) involve modifications of co-payment schemes for ED visits and other healthcare service providers such as PCPs. In Singapore, a primary care incentive scheme was introduced recently in the eastern part of the island. Patients who consulted private GPs participating in this scheme would receive a waiver of SGD 50 in ED consultation fees should they be subsequently referred to the ED. A study showed that this scheme appeared to contribute to a greater reduction in ED attendances via self-referrals in the first year of implementation relative to the preceding two years.(43)
On the whole, results on the effectiveness of reported IA reduction interventions were limited and mixed. Nevertheless, lessons from past studies and the findings of this study could guide how future research studies should be organised to better understand why specific subgroups of the population visit the ED inappropriately and what interventions could effectively reduce their IA.
Our study was not without limitations. Although a recent study(26) found that the appropriateness criteria employed in our study to classify ED attendances into AA and IA were consistent with the opinions of senior A&E physicians in CGH, we acknowledge that these criteria may not result in error-free classification. Since the beginning of 2014, CGH A&E physicians have employed the same classification criteria to estimate and monitor the appropriateness level of referrals by GP clinics. Due to the positive experience of using these criteria, CGH A&E physicians felt that they offered good and reliable estimates of IA in their A&E. Another limitation was the use of driving distance as a proxy measure for the proximity of attendees to the CGH A&E and the nearest 24-hour GP clinics. The residential addresses of attendees captured in the CGH A&E databases might not be up to date; attendees might also not have commuted from their residences to the A&E for their respective attendances. Moreover, they might not have used driving distance in deciding between GPs and the A&E but based their decision on travelling time or cost instead, which in turn depended on factors including transportation modes, traffic conditions and time of the day. However, the lack of relevant data made the shortest driving distance based on the reported residential address of the A&E attendees the best estimate of their proximity to the CGH A&E and their nearest 24-hour GP clinics. Last but not least, we were also unable to account for the effect of other attendee-related factors, such as health literacy, socioeconomic status and educational background, in this analysis due to the lack of relevant information in our data set.
In conclusion, this study offered insights on subgroups in the local population who were more likely to contribute to IA at the CGH A&E. It also suggests that more research is required to understand the factors influencing the choice to visit the ED rather than a PCP for non-emergency conditions. Interventions could then be designed to address these factors and therefore reduce the workload attributable to IA. Such an understanding would be crucial for the development of measures or policies that could effectively reduce avoidable IA.


