Abstract
Intramuscular haemangiomas are benign soft tissue tumours that are more frequently seen in children and young adults. As they may be difficult to diagnose clinically, imaging has an important role in the detection, diagnosis and preoperative planning of these lesions. Haemangiomas of the extremities may be classified into capillary, cavernous, venous and mixed types, with or without an arteriovenous shunt, depending on the predominant vascular channels. Nonvascular components such as fat, smooth muscle, fibrous tissue and thrombus may also be present. This pictorial essay highlights the imaging features of intramuscular haemangiomas, with an emphasis on magnetic resonance imaging.
INTRODUCTION
Intramuscular haemangiomas are benign soft tissue tumours that are more frequently encountered in children and young adults. Their clinical features are variable, as they may remain undetected for years, or may present as a painless mass or a mass with vague pain after exercise. In the absence of skin discolouration, physical findings in intramuscular haemangiomas are often non-specific. Therefore, imaging, particularly magnetic resonance (MR) imaging, has an important role in detection, diagnosis and preoperative planning of these lesions. In this pictorial essay, we present the imaging features of haemangiomas, emphasising the characteristic features of intramuscular haemangiomas on MR imaging.
CLASSIFICATION
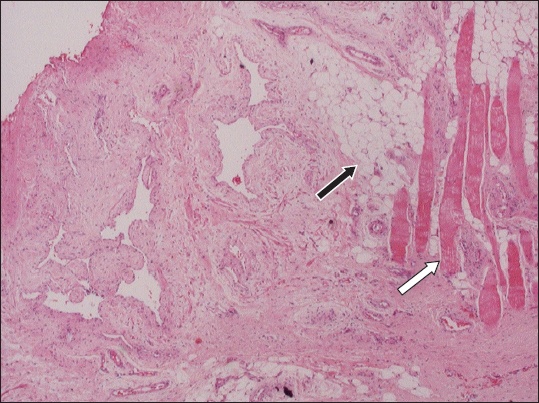
Haemangiomas represent a broad spectrum of benign neoplasms that histologically resemble blood vessels. Haemangiomas are pathologically classified into four types based on the predominant type of vascular channel identified within the lesion; capillary, cavernous, venous and arteriovenous (AV) haemangiomas.(1,2) However, some lesions are known as mixed-type haemangiomas because they have an admixture of different types of vessels. Apart from vascular channels, nonvascular components may be present, particularly in the cavernous type of haemangioma (
Fig. 1
Photomicrograph shows an intramuscular haemangioma that is composed of well-formed vessels as well as some mature fat (black arrow) adjacent to the skeletal muscle fibres (white arrow) (Haematoxylin & eosin, × 10).
CLINICAL PRESENTATION
The clinical presentation of intramuscular haemangiomas is non-specific. Patients usually present with chronic pain and a new palpable mass. Pain is often worsened with exercise due to vascular dilatation and increased regional blood flow, causing swelling and compressive pain.(3) These lesions may intermittently increase in size when placed in a dependent position or during straining, but this change may be difficult to detect in deep-seated lesions. Skin discolouration may be present if the lesion involves the skin and subcutaneous tissue.(2)
GENERAL IMAGING FEATURES
Imaging features reflect the vascular and nonvascular components of haemangiomas. Although haemangiomas are usually either not visible or seen as a non-specific soft tissue mass, radiographs play a major role in detection of calcifications and bone changes. Phleboliths, which are characteristic calcifications present in cavernous and venous haemangiomas, are seen in 20% of intramuscular haemangiomas(4) (
Fig. 2
Radiograph of the foot of a patient with a cavernous haemangioma shows multiple phleboliths (arrows) and an adjacent periosteal reaction in the second metatarsal bone (arrowheads).
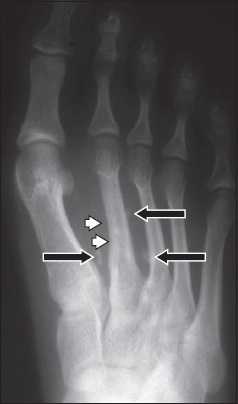
Fig. 3
Radiograph of the shoulder of a patient with cavernous haemangioma shows erosion in areas of the scapula near the glenoid fossa (arrow), with areas of coarsened trabeculae.
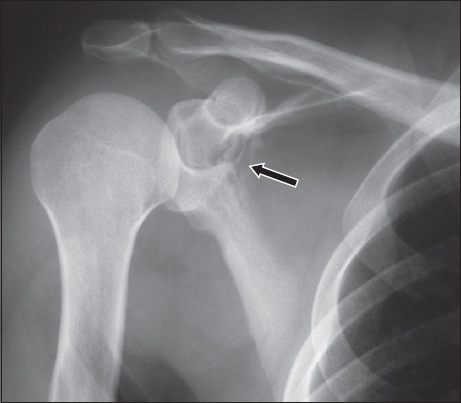
Fig. 4
(a) Radiograph of a patient with arteriovenous haemangioma of the hand shows a soft tissue mass with bony erosion and reactive sclerosis affecting the proximal phalanx of the middle finger. (b & c) Angiograms show markedly dilated and tortuous feeding arteries and prominent arteriovenous shunting.

On unenhanced computed tomography (CT), haemangiomas are seen as poorly defined lesions of similar attenuation as skeletal muscle. After intravenous contrast administration, haemangiomas have a variable degree of enhancement.(2) Small haemangiomas may have intense enhancement similar to that of the adjacent blood vessels. Large haemangiomas may have intense enhancement of the peripheral area and serpentine vascular component, or may have no enhancement.(5,6) Area of fat overgrowth may be detected. Phleboliths are best seen on CT and their detection leads to a specific diagnosis (
Fig. 5
Axial post-contrast CT image of cavernous haemangioma shows a phlebolith (white arrow) within an ill-defined, poorly enhancing mass located in the biceps brachii muscle. The brachial artery and adjacent brachial vein are enhanced (black arrow).
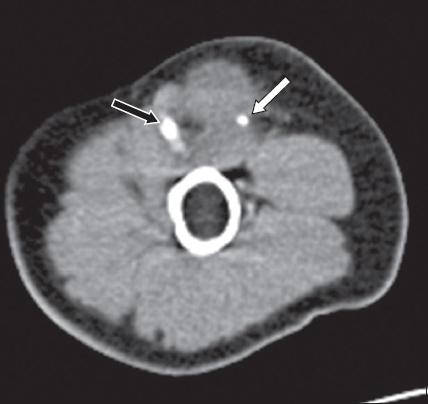
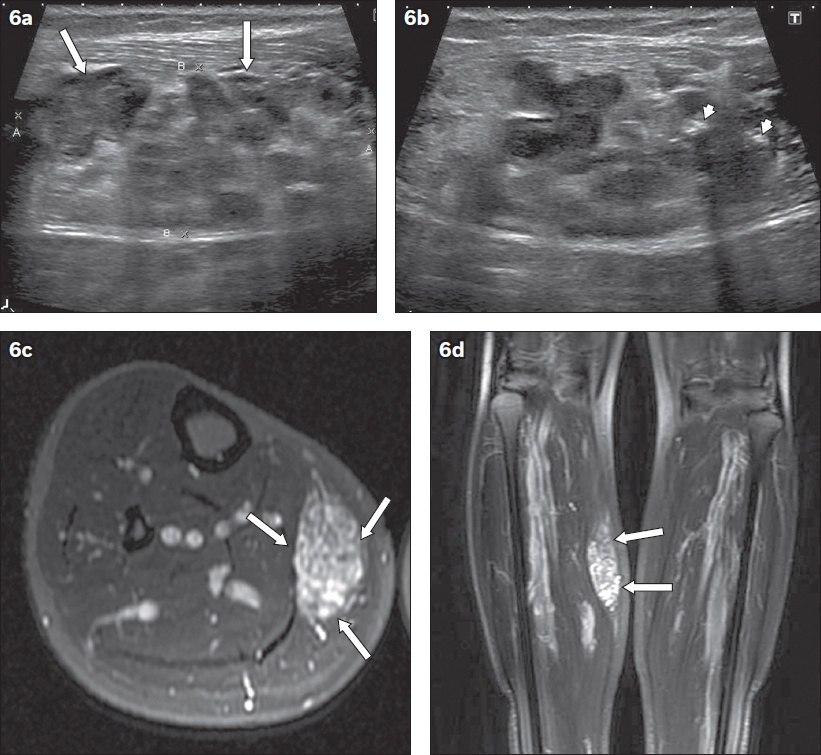
Fig. 6
Superficially located cavernous haemangioma in a 29-year-old man. (a & b) Longitudinal US images show an ill-defined mass with prominent vascular channels (arrows) and phleboliths within (arrowheads). Corresponding (c) axial and (d) coronal T2-weighted MR images show typical features of a well-marginated, predominantly markedly hyperintense, heterogeneous mass within the medial gastrocnemius muscle (arrows).
On MR imaging, both the vascular and nonvascular components of haemangiomas are depicted. The vascular channels are seen as a tangle of tubular structures with hypointense to isointense signal on T1-weighted images and hyperintense signal on T2-weighted images relative to muscle.(2) The flow voids seen on all pulse sequences indicate rapid blood flow.(10) On T1-weighted images, fat overgrowth is seen as areas of hyperintensity. Phleboliths appear as circular areas of hypointensity. Haemorrhage may be detected as areas of hyperintense signal on T1-weighted images, with fluid-fluid levels on T2-weighted images.(11) On angiography, variable findings are associated with haemangiomas, depending on the types of vascular components (Figs.
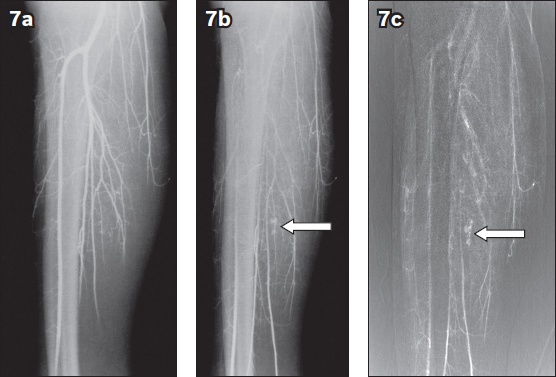
Fig. 7
Nonsubtracted serial angiograms of a calf venous haemangioma taken at (a) five seconds and (b) ten seconds and (c) a digital subtraction image taken at 20 seconds show normal arteries and gradual filling of a small tangle of blood vessels (arrows).
In clinical practice, MR imaging is the single most useful modality for diagnosis of haemangiomas, because it can characterise the flow rate of the vascular channel and identify the type of nonvascular component.(8) Radiographs complement MR imaging in detecting calcifications. Haemangiomas may be detected by US or CT, but the advantages of US and CT are fewer than those of MR imaging. Angiography is reserved for further imaging of AV haemangiomas to identify the feeding arteries and draining veins, usually prior to embolisation. The MR imaging protocol for extremity lesions should include the axial and longitudinal planes – with the longitudinal plane being either a coronal or sagittal plane depending on lesion location. The pulse sequences typically comprise T1- and T2-weighted sequences and post-contrast enhanced T1-weighted images. The latter are obtained with application of fat suppression for better lesion delineation.
IMAGING FEATURES IN SPECIFIC TYPES OF HAEMANGIOMAS
Capillary haemangioma
Capillary haemangiomas are composed of small vessels lined by a flattened endothelium. This type of haemangioma usually involves the skin and subcutaneous tissue, and has a typical clinical appearance (
Cavernous haemangioma
Cavernous haemangiomas are composed of dilated blood-filled spaces lined by flattened endothelium. Fat components have been found in as many as 93%–100% of lesions, and are considered a reactive phenomenon rather than a true neoplasm.(2,5) Because the mass does not involute and often requires surgical excision, cavernous haemangioma is the type of haemangioma that most frequently requires imaging for either diagnosis or surgical planning.(7) Phleboliths are commonly seen in cavernous haemangiomas as a result of dystrophic calcification within organising thrombi, and typically appear as rounded T1- and T2-hypointense areas on MR imaging. Amorphous or curvilinear calcification may occur. Pathologically, the amorphous and curvilinear calcifications reflect the mature bone interspersed with large cavernous vascular channels.(14)
On MR imaging, cavernous haemangiomas appear as heterogeneous masses due to nonvascular components, which consist of fat, fibrous septa, smooth muscle or blood products (
Fig. 8
Longstanding subcutaneous capillary haemangioma with intramuscular involvement in a 20-year-old woman. (a) Clinical photograph of the left buttock shows soft, raised, reddish lesions that are non-tender to the touch. Axial (b) T1-weighted, (c) T2-weighted and (d) post-contrast T1-weighted MR images show an extensive infiltrative T1-isointense and T2-hyperintense lesion that is intensely enhancing. Although it is mostly located in the subcutaneous fat plane, there is involvement of the underlying gluteus muscles. (e) Axial and (f) coronal two-dimensional time-of- flight MR angiography images show the feeding arteries from the left internal and external iliac arteries. The left common iliac vein is enlarged due to the increase in blood flow from the draining veins.
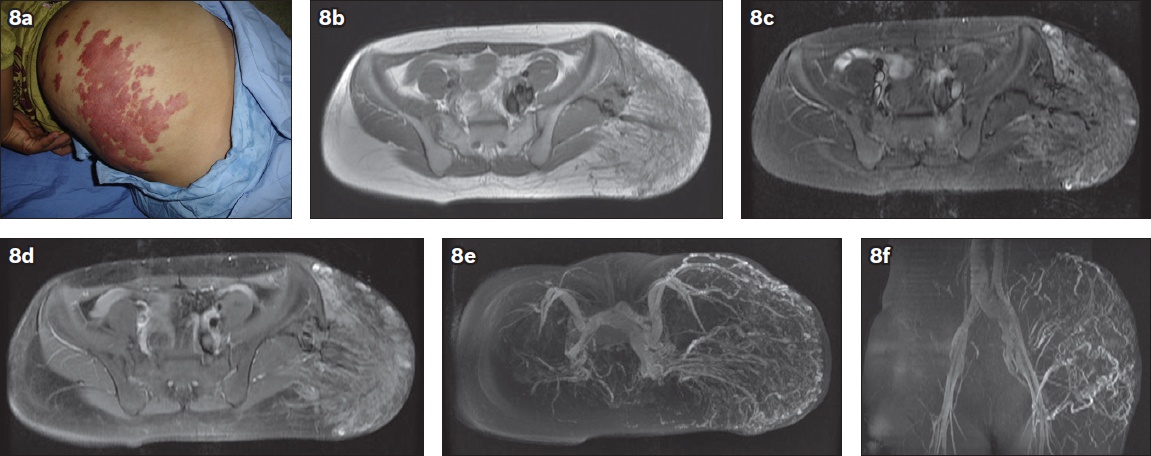
Fig. 9
Intramuscular cavernous haemangioma of the foot with subcutaneous and bone involvement. Axial (a) T1-weighted, (b) T2-weighted and (c) post-contrast T1-weighted MR images show T1-isointense and T2-hyperintense signal relative to muscle within an extensively infiltrating lesion. Contrast enhancement is mild and heterogeneous. Fluid-fluid levels due to previous bleeding are seen (white arrows). Non-enhancing components are due to phleboliths (black arrows), fibrous septa (dashed arrows) and smooth muscles (black arrowheads). Note the vascular channels in the cortical bone and medullary cavity of the metatarsal bone (white arrowheads).
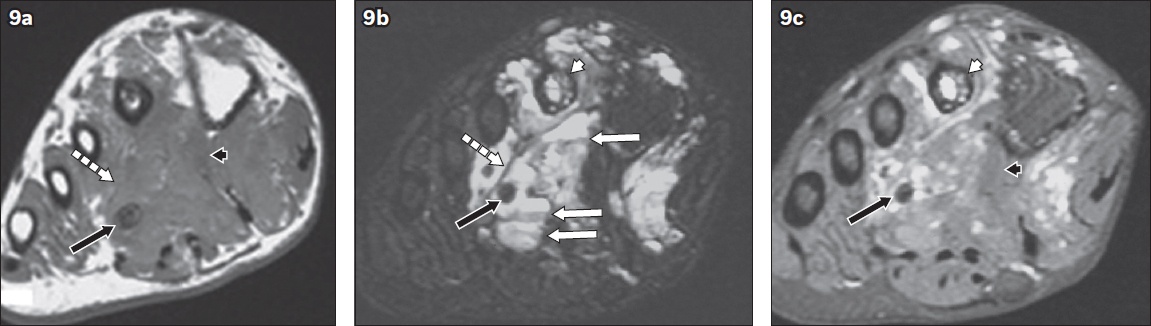
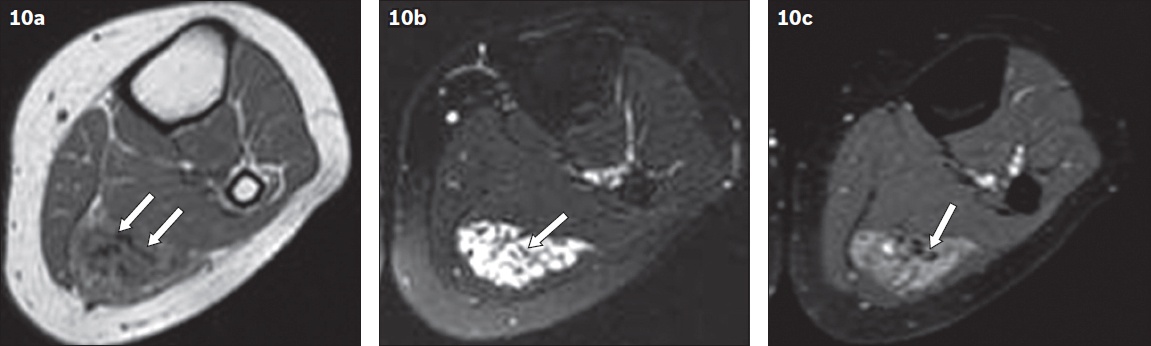
Fig. 10
Intramuscular cavernous haemangioma of the calf. Axial (a) T1-weighted, (b) T2-weighted and (c) post-contrast T1-weighted MR images show T1-isointense and markedly T2-hyperintense signal within a lobulated mass that is well-defined on T2-weighted imaging. Multiple septa are present (arrows). Contrast enhancement is heterogeneous.
Venous haemangioma
Venous haemangiomas are predominantly composed of vessels with thick muscular walls. These haemangiomas have slow blood flow. Thrombus and phleboliths may be found within these lesions.(2) On MR imaging, the serpentine vascular channels are seen as areas of T1-isointensity and marked T2-hyperintensity relative to muscles (
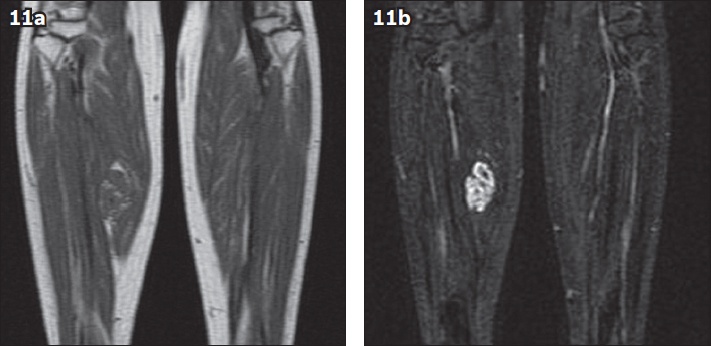
Fig. 11
Intramuscular venous haemangioma of the right calf. Coronal (a) T1-weighted and (b) T2-weighted MR images show T1-isointense and marked T2-hyperintense signal within a lesion that has a well-defined serpentine configuration on T2-weighted imaging. Small areas of intralesional fat appear T1-hyperintense.
Arteriovenous haemangioma
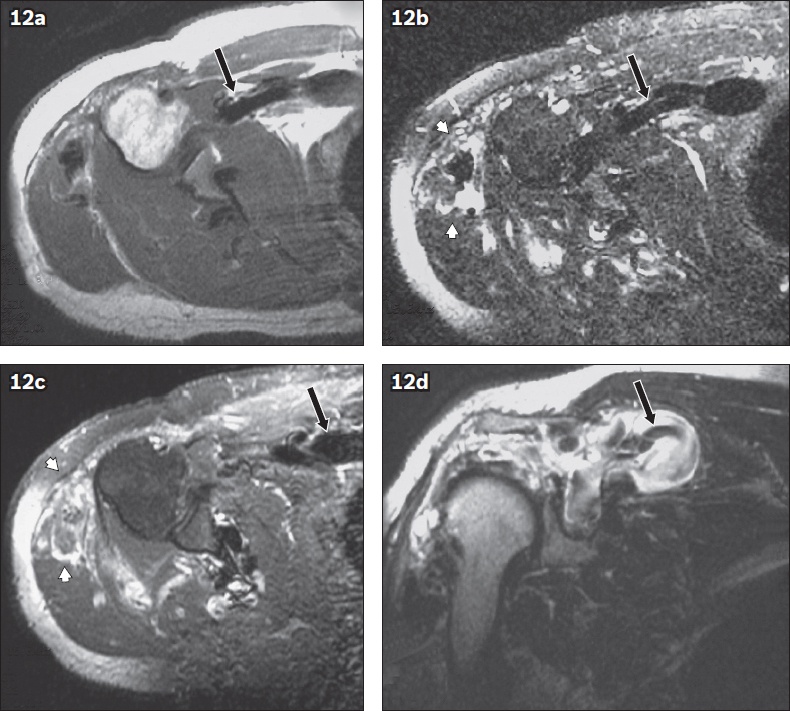
AV haemangiomas are composed of abnormal communications between arteries and veins. This type of haemangioma is characterised by high blood flow due to the AV shunting. Occasionally, stenosis and thrombus may cause reduced flow and mimic a mass.(16) Clinical abnormalities associated with high-flow lesions include venous distention, bruit and increased overlying skin temperature. In patients with a large AV shunt that increases cardiac output, Branham sign, which is a reflex bradycardia after compression of the shunt, may occur.(7) On MR imaging, AV haemangiomas contain high-flow vascular channels, which are seen as curvilinear or serpentine areas of flow void on all pulse sequences. Because they frequently contain areas of capillary or cavernous haemangioma, a combination of features may occur, and such AV haemangiomas are sometimes called mixed-type haemangiomas (
Fig. 12
Mixed arteriovenous and cavernous haemangioma of the shoulder of the patient in Fig. 3. Axial (a) T1-weighted, (b) T2-weighted; and (c) post-contrast T1-weighted and (d) coronal T2-weighted MR images show flow voids in the large vascular channels on all pulse sequences, due to the fast-flow phenomenon (arrows). The rest of the lesion represents the cavernous component, which shows patchy T2-hyperintense areas that are markedly enhanced (arrowheads).
CONCLUSION
Intramuscular cavernous, venous and AV haemangiomas have typical features on MR imaging. As clinical findings are usually non-specific, recognition of imaging appearances aids in detection and arriving at a confident diagnosis. Accurate diagnosis by MR imaging helps to avoid unnecessary surgery. In cases where surgery is required, MR imaging aids in preoperative planning.
SMJ-61-128.pdf


