INTRODUCTION
Mental illness is a growing public health concern. In a local population-based survey conducted in 2012, 12.0% surveyed had at least one lifetime affective, anxiety or alcohol use disorder. Among those with mental disorders, 50.6% had a chronic medical disorder.(1) Epidemiologic studies have shown a strong link between mental illness, mental health and physical health, especially in relation to chronic disease occurrence, health outcomes and treatment. It was suggested that when depression and chronic disease co-occur, the association between the two conditions could be the depressive disorders precipitating chronic disease or the chronic disease exacerbating symptoms of depression, or a combination of both.(2-4)
There has been a growing emphasis on the role of family physicians in the management of patients with mental illness given their key role in providing care in the community. In Singapore, a study in 2003 found that patients rated general practitioners as their most preferred caregiver, and family physicians were used by 41.1% of those who sought help for mental health illness.(5)
The National Healthcare Group Polyclinics (NHGP) comprise six primary care clinics located in the central and northern parts of Singapore. NHGP’s Health and Mind Service (HMS) was started since October 2012 as part of the National Mental Health Blueprint, which aims to promote mental health and prevent development of mental health problems. In collaboration with the Agency for Integrated Care and psychiatrists from the Institute of Mental Health and Khoo Teck Puat Hospital, it is a physician-led, multidisciplinary team that manages patients with mild to moderate common mental health conditions in the primary care setting.
Patients at the HMS range from existing NHGP patients whom we have seen for any number of years for their physical conditions before being referred to the HMS, to patients who visit polyclinics to be enrolled in the HMS and are subsequently noted to have concurrent physical health issues. They are first assessed by a psychologist. Patients requiring pharmacotherapy or further evaluation are referred to the doctors in the HMS, who have attained postgraduate qualifications (e.g. Graduate Diploma in Family Medicine, Graduate Diploma in Mental Health or Master of Medicine [Family Medicine]) and received prior training through direct supervision from psychiatrists. In addition to conducting psychotherapies to manage psychological conditions, psychologists are also equipped to modify maladaptive health behaviours exhibited by patients with behavioural risk factors. The allocated time for each HMS session with the doctors is 20 minutes, twice the time of general clinic consultations. Patients with concomitant physical health conditions will also be managed.
In this study, we sought to examine the impact of our mental health service on the management of chronic diseases in patients with both mental health conditions as well as chronic diseases.
METHODS
We reviewed the medical records of patients who were cared for by NHGP HMS teams from January 2016 to December 2018. We included all patients who (a) had been diagnosed with depression (based on Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria) at least once during this time period by the attending HMS doctor or psychologist and (b) had the diagnosis of diabetes mellitus and/or hypertension and/or hyperlipidaemia at the initial HMS visit date. Retrospective data was collected from patients’ electronic medical records, extracted using Oracle Business Intelligence Enterprise Edition. The following clinical outcomes were compared before and after enrolment: (a) Patient Health Questionnaire-9 (PHQ-9) score; (b) blood pressure (BP); (c) low-density lipoprotein cholesterol (LDL-C) levels; (d) glycated haemoglobin (HbA1c) for patients with diabetes mellitus; and (e) body mass index (BMI).
Baseline readings were compared to the latest readings within 18 months of the patient’s initial HMS visit. Wilcoxon signed rank test was used to compare the mean of the latest readings with the baseline mean. For each outcome, the listwise deletion method was used to handle patients with missing outcomes at baseline and with no follow-up readings within 18 months from their initial HMS visits. IBM SPSS Statistics version 26.0 (IBM Corp, Armonk, NY, USA) was used for all statistical calculations and analyses. Continuous variables were expressed as mean, while categorical variables were expressed as standard deviation and proportions, respectively.
RESULTS
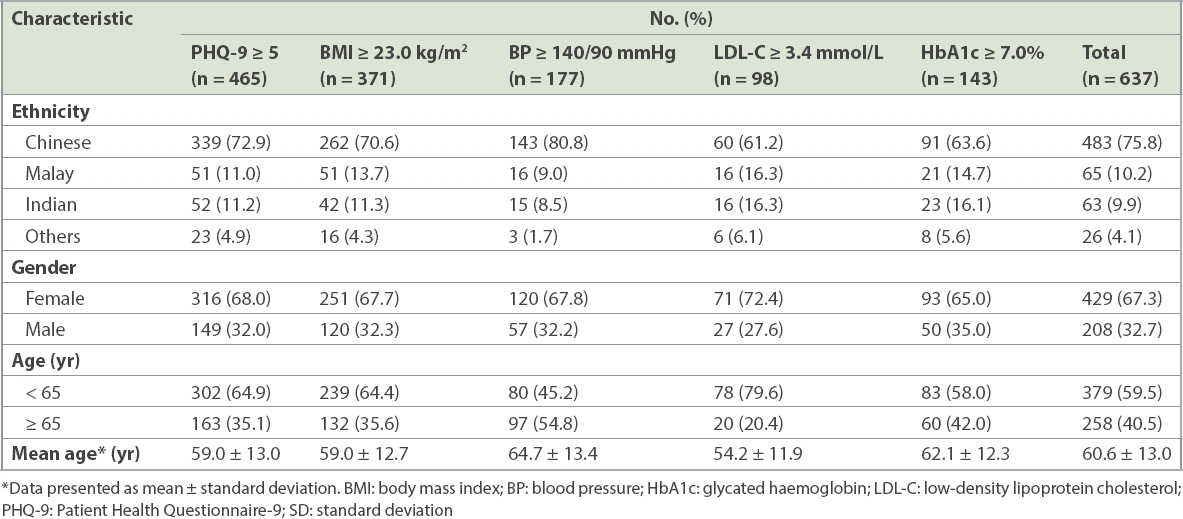
A total of 637 eligible patients who had been diagnosed with depression and had a diagnosis of diabetes mellitus and/or hypertension and/or hyperlipidaemia were evaluated. More than half (59.5%) were aged below 65 years and had a mean age of 60.6 ± 13.0 years. 547 (85.9%) patients had hyperlipidaemia, 459 (72.1%) had hypertension, and 272 (42.7%) had diabetes mellitus. This is reflective of the top three conditions for polyclinic attendance from 2017 to 2019 based on Ministry of Health, Singapore, statistics.(6) 201 patients had one of these three chronic diseases, 231 had two and 205 had all three chronic conditions.
Table I
Baseline characteristics of patients with suboptimal control of diabetes mellitus, hypertension and/or hyperlipidaemia who were enrolled in the Health and Mind Service (n = 637).
In addition, 57.3% (365/637) of the patients were on antidepressants. The average number of HMS psychologist sessions and doctor sessions utilised by these patients was 2.3 and 3.7, respectively.
The percentage of patients with PHQ-9 scores of ≥ 5 decreased from 86.8% at baseline to 53.2% within 18 months from the initial HMS visit. Mean PHQ-9 scores also showed a significant improvement from 10.4 ± 5.5 to 5.6 ± 4.9 within 18 months (p < 0.001). Mean LDL-C levels increased from 2.5 ± 0.9 mmol/L to 2.6 ± 0.9 mmol/L (p = 0.005). There was a significant gain from a mean baseline BMI of 25.8 ± 5.3 kg/m2 to 26.0 ± 5.5 kg/m2 within 18 months of the initial HMS visit (p = 0.03). There were no significant changes in BP and HbA1c levels from baseline (
Table II
Overall outcomes of patients with diabetes mellitus, hypertension and/or hyperlipidaemia who were enrolled in the Health and Mind Service.
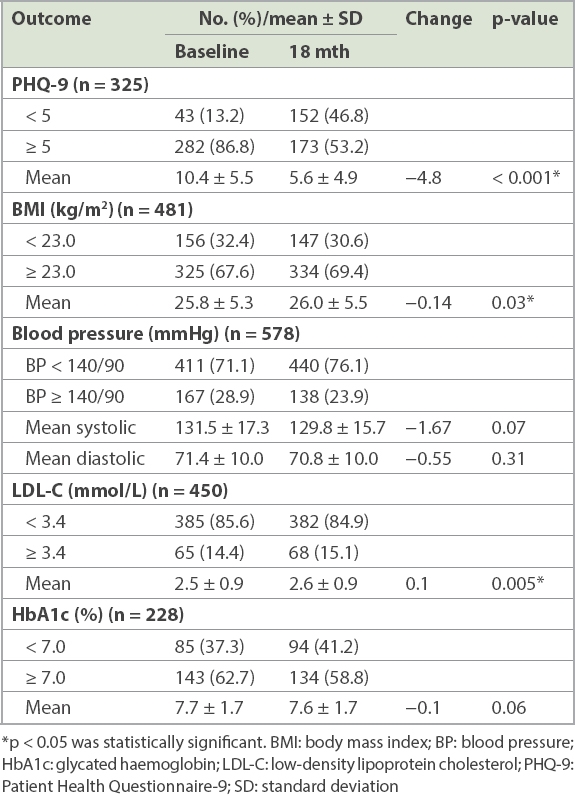
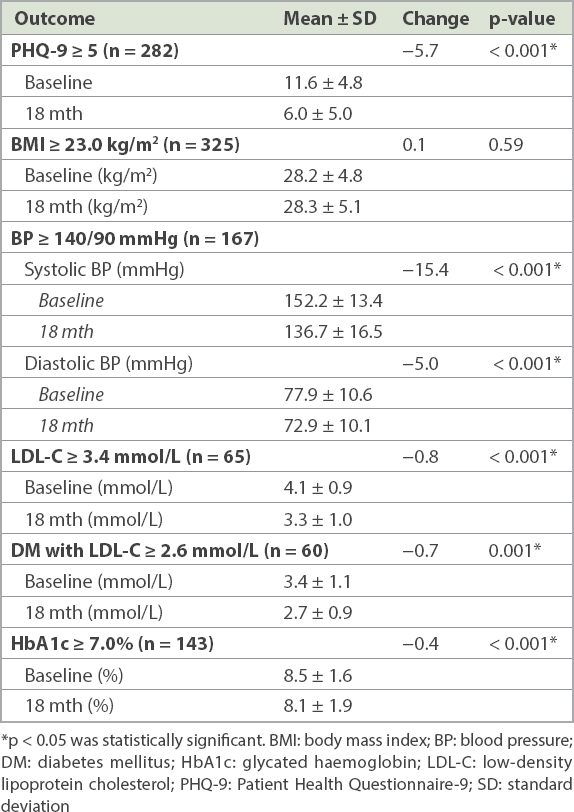
Table III
Outcomes of patients with elevated PHQ-9, BMI, BP, LDL-C or HbA1c values at baseline.
Notably, there was no available data on PHQ-9 and BMI for 49% and 25% of the study population. There was also no BP, LDL-C and HbA1c data for 21% (n = 578), 18% (n = 547) and 16% (n = 272) of patients with hypertension, hyperlipidaemia and diabetes mellitus, respectively (Appendix Supplementary
DISCUSSION
Our finding corresponds with those of other studies showing that treatment of depression within a primary healthcare setting is effective with the use of pharmacological and psychological interventions.(9-12) Treating depression of mild to moderate severity in a primary care practice could be more cost effective compared to the tertiary setting.(13) Furthermore, another study showed a reduction in costs associated with integrated depression treatment for patients with diabetes mellitus.(14) This underpins the feasibility of a primary care-led system addressing both physical and mental health needs in providing more cost-effective and affordable healthcare.
The overall mean percentage of patients across NHGP clinics who had optimal readings for BP (< 140/90 mmHg), LDL-C (< 3.4 mmol/L) and HbA1c (< 7.0%) in 2016 was noted to be 74.1%, 84.9% and 45.4%, respectively, as compared to the baseline percentage of our HMS patients (71.1%, 85.6% and 37.3%, respectively;
Patients with baseline BP ≥ 140/90 mmHg had significant improvement in their BP readings. This is consistent with previous reports on the benefits of psychological treatments on BP reduction. An article by Bogner and de Vries in 2008 showed that integrating depression treatment into care for hypertension improved adherence to antidepressant and antihypertensive medications, which in turn led to fewer depressive symptoms and reductions in systolic and diastolic BP.(15) Implementing such an integrated model at the primary care level appears to be feasible and effective in managing patients with depression and hypertension.
Our findings also showed improvements in LDL-C among patients with suboptimal baseline levels ≥ 3.4 mmol/L. A recent article by Rohde et al showed that depressed patients were more likely to be initiated with and be adherent to lipid-modifying medicine and glucose-lowering agents, as well as achieve their LDL-C target, when they were placed on antidepressant treatment.(16)
There was a significant reduction in HbA1c readings within 18 months of the initial HMS visit among patients with a baseline HbA1c level ≥ 7%. This observation is in keeping with extant literature on the efficacy of psychological interventions in improving glycaemic control. The American Diabetes Association has advocated that treatment with either cognitive behaviour therapy or antidepressant medication could improve both mood and glycaemic control.(17) A systematic review by Schmidt et al on the efficacy of psychological interventions in treating patients with diabetes-distress revealed that specifically tailored psychological interventions are effective in reducing elevated diabetes-distress and HbA1c.(18)
We also found a significant gain in mean BMI of 0.14 among the patients. This was not likely to be clinically significant. Further analysis of patients who were on antidepressants did not show any significant change in their BMI (Appendix Supplementary
Overall baseline mean BP, LDL-C and HbA1c were not poorly controlled in our patients despite the co-existing diagnosis of depression. This could be explained by the fact that patients with suboptimal control of chronic diseases made up less than half of our population with hypertension, hyperlipidaemia or diabetes mellitus. It also seems to contradict the widespread notion that depression tends to have a negative impact on chronic disease control. One could theorise that the patients we encountered in the primary care setting had mild to moderate psychological issues that did not impact their chronic disease control significantly.
To our knowledge, there is limited published literature on the impact of mental health services on chronic disease management at the primary healthcare level. Our study has sought to explore the benefits of involving mental health services in the management of our patients with physical illnesses.
Our study had some limitations. As we used existing, routinely captured data from medical records for this study, some patients had missing data and hence were not included in the study. Patients with missing data could have been defaulters and their exclusion from our data analysis could have skewed our results. There was also no control group to compare similar patients with chronic diseases who were not seen at the HMS, to allow us to draw the conclusion that mental healthcare had indeed led to improvements in patients’ chronic conditions. We did not include other forms of treatment that the patients might have received for their chronic conditions. For instance, an empanelment care model introduced in 2015 enables patients to see a designated team of healthcare professionals, which would have influenced the chronic disease outcomes of our patients.
In conclusion, for patients with depression and other concomitant chronic conditions, the HMS not only improved their psychological health but also the readings of patients with suboptimal control of diabetes mellitus, hypertension and hypercholesterolaemia. However, missing data could have introduced bias and affected our study conclusion. Further studies to assess the long-term effect of mental healthcare on these physical medical conditions could lead to improvements in long-term management.
Efforts to improve integration of care that address both the physical and mental health needs of our patients will help to raise the standard of patient care and experience. As Singapore’s population ages, an increasing number of people face chronic illness, and greater understanding of the value of addressing mental health issues in our chronic disease management strategies can significantly improve clinical outcomes and reduce disease burden.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to Dr Karen Ng, Director of Clinical Services, NHGP; Dr Colin Tan, Deputy Director of Clinical Services, NHGP; Ms Sheyanne Yow, Clinical Services, NHGP; and the Clinical Research Unit at NHGP for their support and roles as advisors. The authors would also like to express their appreciation to Dr Jared Ng Wei Lik, Consultant, North Region/Developmental Psychiatry, Institute of Mental Health; Dr Chan Keen Loong, Senior Consultant, Psychological Medicine, Yishun Health; Ms Tan Hui Nah, Principal Medical Social Worker, NHGP; and Dr Wong Mei Yin, Principal Psychologist, NHGP, for their roles in running and supporting the HMS.
SMJ-62-235-Appendix.pdf


