Abstract
INTRODUCTION
The efficiency of postoperative handover of paediatric patients to the children's intensive care unit (CICU) varies according to institutions, clinical setup and workflow. Reorganisation of handover flow based on findings from observational studies has been shown to improve the efficiency of information transfer. This study aimed to evaluate a new handover process based on recipients' perceptions, focusing on completeness and comprehensiveness of verbal communication, and the usability of a situation, background, assessment and recommendation (SBAR) form.
METHODS
This was a prospective interventional study conducted in the CICU of KK Women's and Children's Hospital, Singapore. It comprised four phases: (1) evaluation of the current handover process through an audit and opinion survey; (2) development of a new handover process based on the opinion survey and hospital personnel feedback; (3) implementation; and (4) evaluation of the new handover process. The new handover process was based on a PETS (pre-handover, equipment handover, timeout and sign out) protocol with a 'single traffic communication' flow and a new SBAR handover document. It included relevant patient information, and the options 'not applicable' and 'none', to increase compliance and reduce ambiguity.
RESULTS
Significantly more recipients indicated that the new SBAR form was the most important handover tool and provided more useful information. Recipients' perceptions indicated improvement in information sufficiency and clarity; reduction of omission errors; and fewer inconsistencies in patient descriptions in the new process.
CONCLUSION
Dual customisation of the handover process, PETS protocol and SBAR form is necessary to meet the workflow and information demands of the receiving team.
INTRODUCTION
Postoperative handover from the operating theatre (OT) to intensive care unit (ICU) is a key process to ensure patient safety and continuity of care.(1) Information communicated in the handover process should include perioperative anaesthetic and surgical issues, as well as recommended postoperative management.(2) The challenge is further increased in a setting where paediatric patients have complex surgical and medical issues, and interdisciplinary communication occurs between the outgoing anaesthetic team and incoming paediatric intensive care team.(3)
Over the years, various handover techniques have been established to provide continuity of patient care during change of shift,(4) interdisciplinary referral,(4,5) postsurgical care from the OT to ICU(6) and ward transfer of a patient.(7) Techniques such as narrative face-to-face communication,(3,8) standardised protocols,(1,2,5) and written documents(1,2) have been used in the handover process. In many institutions worldwide, handover documents have been shown to be a useful tool in the process, as they maximise communication during the handover.(1,2,6) The handover document also serves as a quick reference for pertinent perioperative information by providing a succinct summary of the patient's perioperative anaesthetic care.(2,6) Optimal efficiency for patient safety has been achieved by adopting communication mnemonics such as SBAR (situation, background, assessment, recommendations) for handover documentation and communication patterns.(8,9)
At KK Women's and Children's Hospital (KKH) in Singapore, handover from the OT, by outgoing anaesthetists to the paediatric intensivists (PIs) and nurses in charge of the children's intensive care unit (CICU), comprises verbal face-to-face communication and an SBAR handover document. Upon arrival in the CICU, the anaesthetist discusses the intraoperative events that are significant for initial management of the patient in the CICU, the surgeon provides surgical details and advice on patient care, while the anaesthetic unit nurse passes on the patient's particulars to the CICU nurse. The SBAR handover document is completed by the anaesthetic team prior to the transfer. However, issues regarding completeness, efficiency, clarity and accessibility of information pertaining to the current handover process and SBAR form have been raised by receivers from the CICU. As a response, we conducted a study to improve the current handover process and SBAR handover document. The objective of this present study was to evaluate the new handover process against the current process based on the recipients' perceptions, with the focus on the completeness and comprehensiveness of verbal communication and usability of the SBAR document.
METHODS
After procuring Integrated Regulatory Board approval, we conducted a prospective interventional study from October 2011 to December 2012 at the CICU of KKH, a 830-bedded hospital for women and children. The hospital's CICU is a 16-bedded unit that serves over 700 patients a year, with onsite attention for medical, general, trauma, plastic, neurological and cardiovascular surgery. The main caregivers include PIs, comprising seven paediatric consultants, rotating registrars, medical officers and 70 skilled nurses. A total of 52 CICU personnel participated in the study: eight PIs (seven paediatric consultants and one rotating paediatric registrar) and 44 nurses working in shifts.
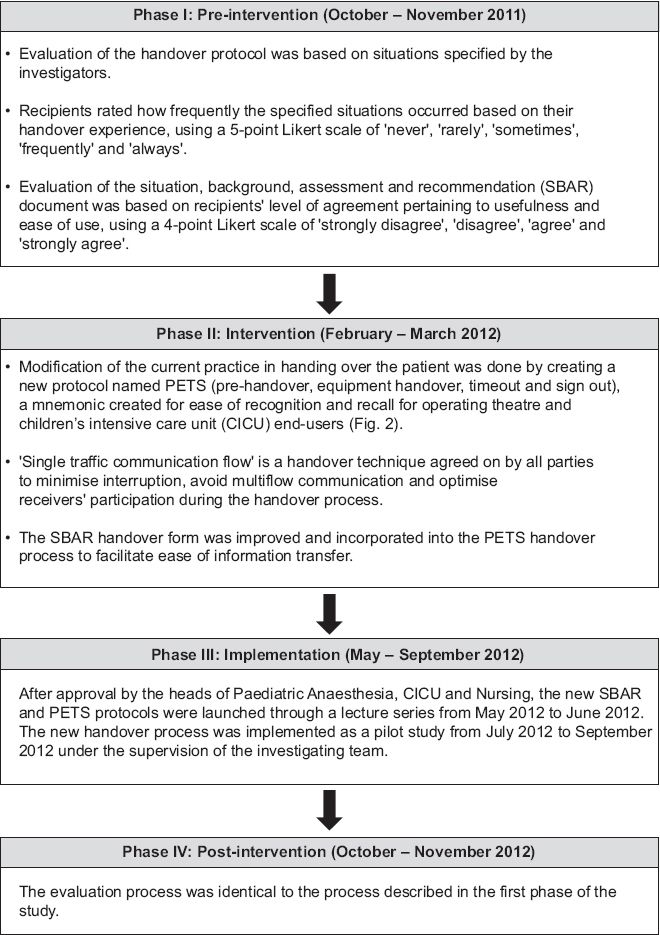
The study was conducted in four phases: pre-intervention, intervention, implementation and post-intervention (
Fig. 1
Flowchart shows the methodology of the study.
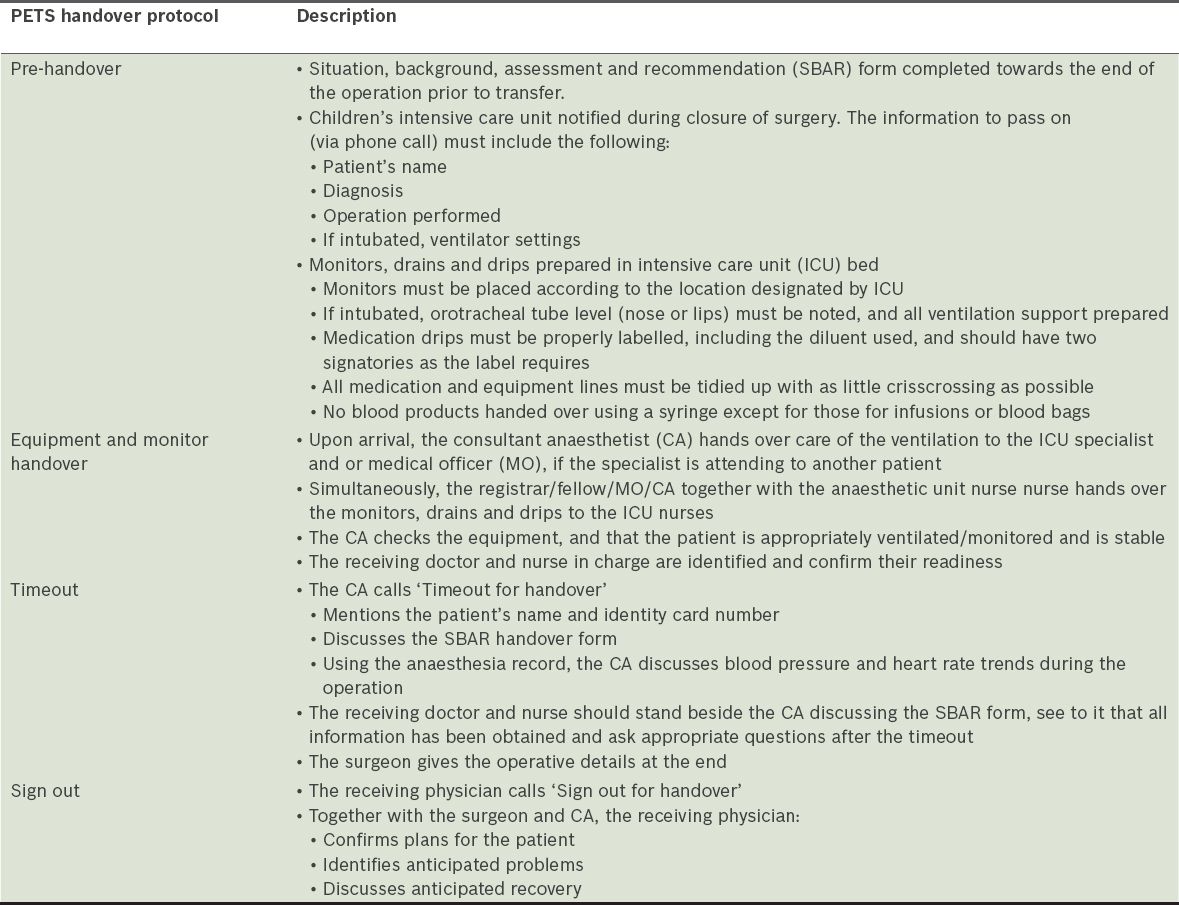
A new handover protocol, PETS (pre-handover, equipment handover, timeout and sign out), was created to meet the end-users' requirements as reflected in the pre-intervention survey (
Table I
Pre-handover, equipment handover, timeout and sign-out (PETS) protocol from operating theatre to children's intensive care unit.
To improve the usability of the original SBAR handover document (
Data pertaining to situational items in the handover protocol on a 5-point Likert scale was reclassified into three categories: 'rare' ('never'/'rarely'); 'sometimes'; and 'frequent' ('frequently'/'always'). Similarly, data pertaining to the utility of the SBAR documents on a 4-point Likert scale was dichotomised as follows: 'disagree' ('strongly disagree'/'disagree'); and 'agree' ('agree'/'strongly agree'). All data was recategorised to facilitate statistical comparison of the recipients' opinions before and after the new handover process was implemented. Frequencies and proportions were used to summarise the data, as all the variables were categorical in nature. Fisher's exact test was used to evaluate associations in each item between the current and new handover processes. Differences in proportions, with corresponding 95% confidence intervals (CIs) based on the Newcombe method,(10) were used to compare the two handover processes, based on recipients who selected 'frequent' and 'agree' for the recategorised situational and utility items, respectively.
The statistical significance level was set at 5%. All tests were two-sided. Data was analysed using R software, 2013 (R Foundation for Statistical Computing, Vienna, Austria; available at:
RESULTS
Table II
Participants' characteristics and perceptions of the pre- and post-intervention handover process.
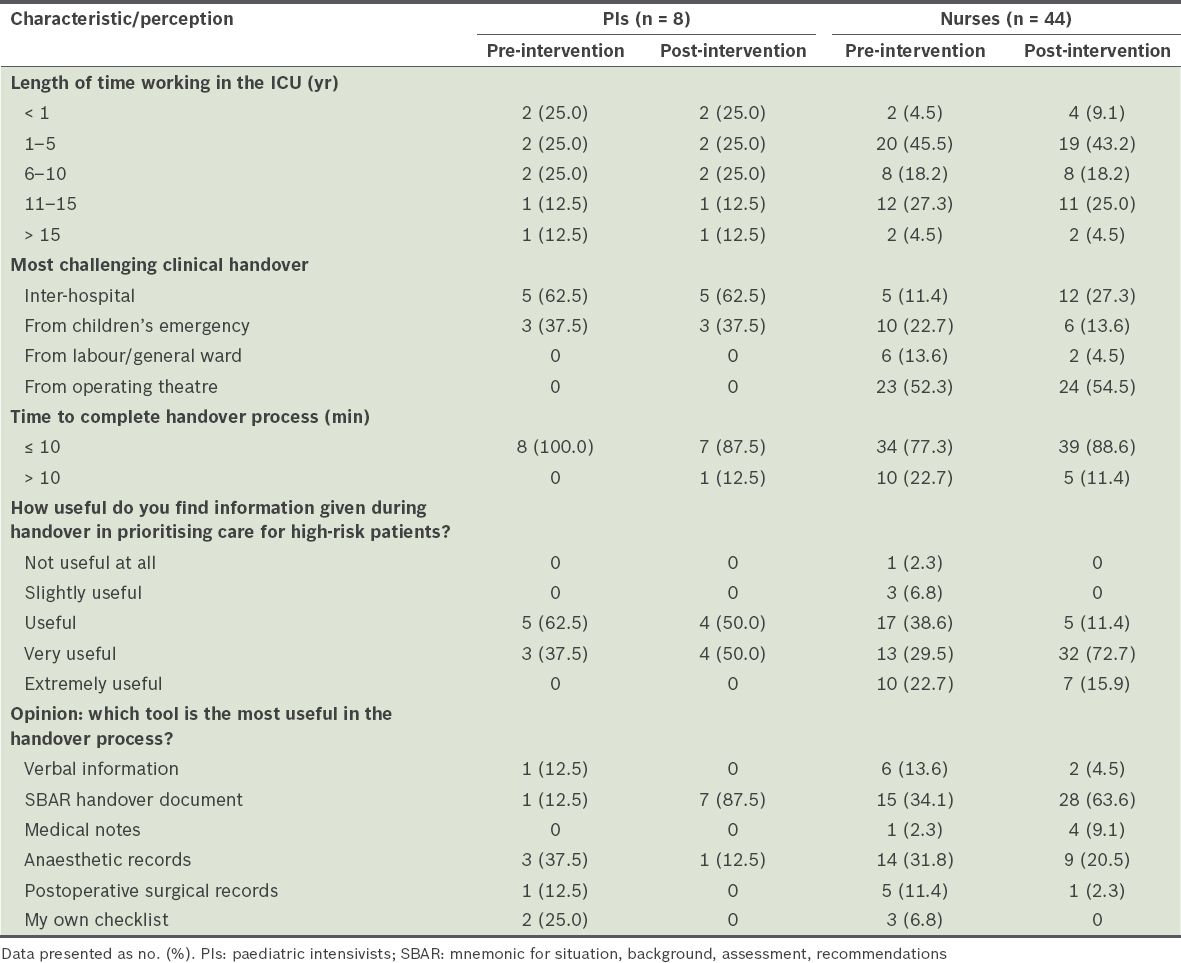
Fig. 2
Graphs show the assessments of children's intensive care unit (a) nurses and (b) paediatric intensivists of the pre-handover, equipment handover, timeout and sign out handover process in the pre- and post-intervention surveys.
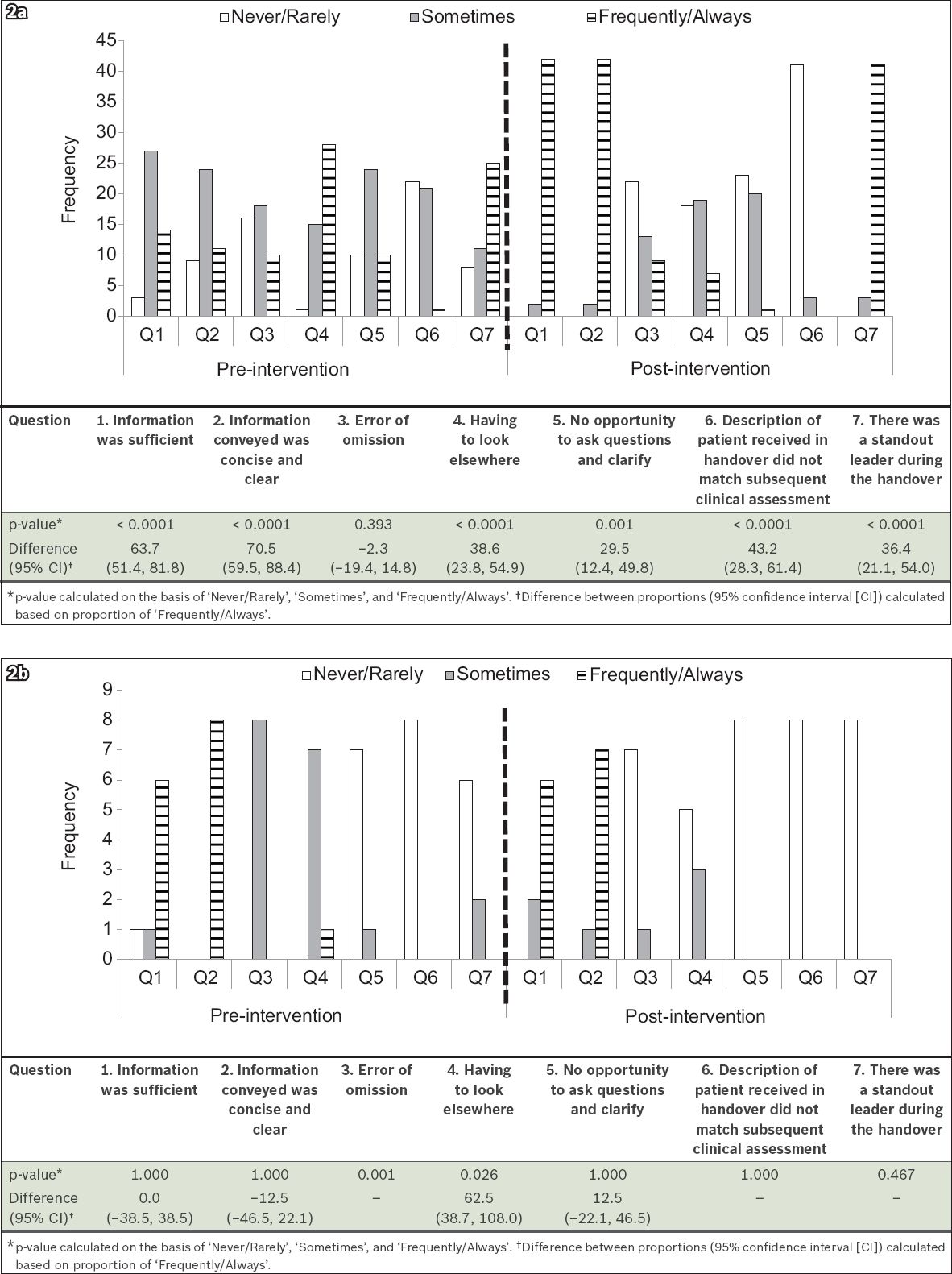
The frequency of occurrence of the situational items pre- and post-intervention, as perceived by the PIs, are detailed in
Overall, the perceived usefulness ('very useful' or 'extremely useful') of the SBAR handover document for prioritising care in high-risk patients during handovers significantly increased by about 33.0% (95% CI 15.0%–53.0%; p = 0.0004). All the PIs indicated that the information provided in the SBAR handover document for both the pre- and post-intervention phases was 'useful' or 'very useful' (
The nurses' and PIs' assessments of the SBAR handover document in the pre- and post-intervention phases are shown in Figs.
Fig. 3
Graphs show the assessments of children's intensive care unit (a) nurses and (b) paediatric intensivists of the situation, background, assessment and recommendation handover document in the pre- and post-intervention surveys.
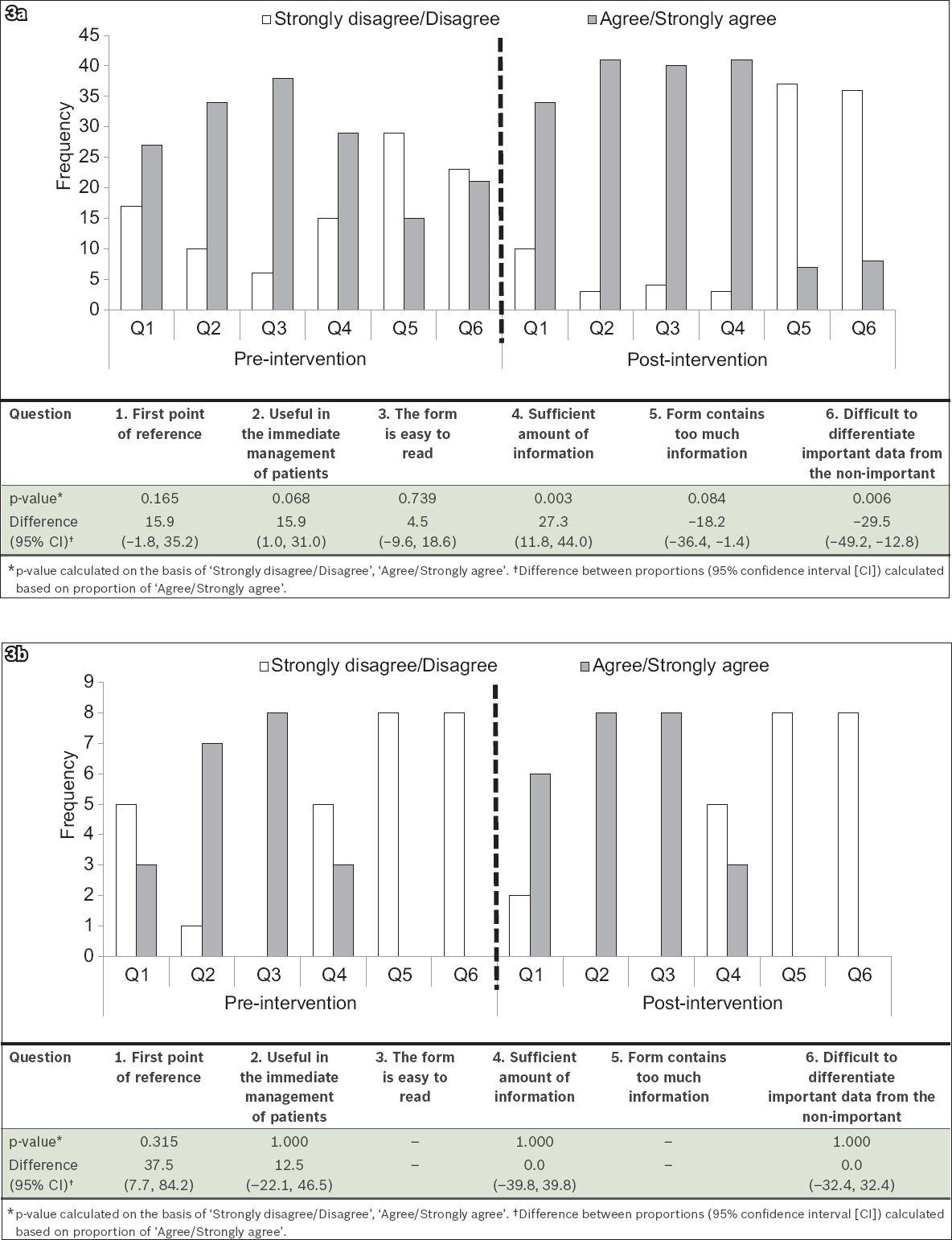
The proportion of PIs who agreed ('agree' or 'strongly agree') that the SBAR handover document was their first point of reference increased in the post-intervention phase (75.0% vs. 37.5%; difference: 37.5%; 95% CI 7.7%–84.2%; p = 0.315;
To evaluate the accessibility of the most informative items, recipients were asked to rank the categories of items based on perceived clinical significance. The rank assigned to a category by most of the recipients (i.e. the mode of each item's rank) was considered its overall rank. The nurses ranked 'patient identification' as their top priority, followed by 'diagnosis and type of surgery' and 'clinical alerts and allergy'. PIs, on the other hand, considered 'patient identification', 'intraoperative problems/issues/blood loss/abnormal bloods' and 'surgical issues' to be the more essential information. This difference in ranking between the PIs and nurses reflects their differing perceptions on the amount of information required at the initial management of patients. Henceforth, relevant patient information can be directed and highlighted in the handover document.
DISCUSSION
In the present study, most of the recipients relied on PETS and indicated that the SBAR handover document was the most important handover tool due to (but not limited to) the increased usefulness of the handover information passed from anaesthetists to recipients. This shows that the new PETS handover protocol was able to address the needs of CICU recipients.
Dual customisation of the handover process (i.e. PETS and SBAR) to meet the workflow and information demands of the receiving team is key to improving the interdisciplinary communication process and delivery of vital information, so as to optimise patient care upon arrival in the CICU. The timeout to call attention of all members of the handover team and sign out to allow the receiving team to question the handover team are essential aspects of the verbal communication during the handover process. Moreover, the addition of a 'none' or 'NA (not applicable)' option for an information item in the handover document facilitates differentiation between an omission error and absence of information and therefore helped to reduce anaesthetists' noncompliance in document completion.
Studies evaluating handover techniques have shown variations among healthcare centres and providers.(11-14) It has been suggested that communication flow during handover should be tailored to suit the structure of an institution and is dependent on processes such as provider transitions and trainee change of rotation.(13,15) Furthermore, anaesthetists and nurses often have different expectations regarding the content and timing of information transfer.(16) Anwari et al's study found that nurses often perceived anaesthetists' handovers to be unstructured with variable communication processes; in 14.0% of handovers, anaesthetists failed to provide any of the key information set by the study.(17)
Even in standard face-to-face handover systems, communication challenges can still occur if the transfer of care is not smoothly executed.(3,8,18,19) Many studies that evaluated handover processes reported that interruptions, environmental factors (e.g. noise, crowding) and specific patient care requirements for both groups of staff involved in the handover resulted in an unstructured and error-prone handover process;(9,15,20) this is similar to the findings of the present study. Furthermore, based on our new PETS handover protocol, while all the PIs indicated that there was rarely a standout leader during handover, 93.2% of the nurses indicated otherwise, thus showing that perception of the existence of a handover leader may depend on the type of CICU personnel. This study followed Nagpal et al's recommendation to involve surgeons during handover.(21) For the PIs, the information relayed by the anaesthetists and surgeon during the 'single traffic communication' handover is equally important; thus, the anaesthetists and surgeon were seen to share the leadership role.
The World Health Organization timeout and sign-out system provided simple and efficient measures to prevent intraoperative errors.(4,5) Adapting this system to the PETS handover protocol led to an increased perception among both nurses and PIs that the new protocol ensured ease in prioritising the management of high-risk patients. The timeout component of the PETS handover protocol called to attention the Pls and nurses in charge of the patient, which minimised interruptions during handover, thus improving the perceived quality and content of the communication delivered by the anaesthetists. The sign-out system was designed to provide opportunities for the CICU receivers to close the loop of information transfer by raising any questions or clarifications.
Catchpole's Formula 1 and aviation handover technique was used as a template in the PETS protocol for clearing equipment, lines and drain tangles during pre- and actual handover.(1) Although they had been trained on equipment handover, during the post-intervention survey, 18 (40.9%) nurses indicated that the equipment section of the PETS protocol required improvement, 15 (34.1%) felt that it had improved and 11 (25.0%) opined that there was no change. The investigators inferred that the following reasons could account for the nurses' perceptions: (a) in-service talks were inadequate to effect change; (b) handover of critically ill patients who required immediate transport could have resulted in disorganised equipment handover; and (c) the primary concern of the operating theatre team was ensuring safety in transport, and thus the organisation of lines, monitors and drains was not prioritised.
Despite the overall perceived improvements in the post-intervention phase, participants did not perceive an increase in the time required to transmit information. More than 80% of the CICU recipients noted that a handover lasted approximately ten minutes, which is on par with that reported by other studies.(2,17)
The SBAR handover document was reformatted to clear up ambiguity, carry optimal information (as expressed by end-users during the pre-intervention survey) for the initial management of patients, and promote ease of use for better compliance. Major changes made to the SBAR handover document to optimise transmission of information included: (a) addition of information on the patient's weight, antibiotics given and time of administration, the latest electrolyte and haemoglobin level, and ventilator setup for intubated patients; (b) recommendations were shortened and required the minimum essential data based on the pre-intervention survey results; and (c) creation of a single document that can be used for both cardiac and non-cardiac surgery (previously separate documents).
The previous SBAR handover document consisted of open-ended sections for each component, which the anaesthetists had to complete before handover. 23.0% of the end-users commented that the open-ended sections were left blank most of the time. It was thus unclear whether the blank sections indicated no clinical data to hand over or lack of compliance of the team handling the information. This scenario could be due to senior PIs' preference for conveying patient information at a face-to-face handover instead of via written communication, and points to the need for a communication form that guarantees compliance even among senior staff.(8,21)
Communication improved not only as a result of changes in the content of the SBAR handover document, but also in the use of the document during face-to-face handover to relay its content ('timeout'); the latter was a requirement of the new PETS handover protocol. Therefore, our results differed from Joffe et al's,(22) as our recipients appreciated the use of the SBAR handover document as a format for face-to-face verbal handover and as a reference for other CICU caregivers who did not participate in the actual handover. This shows that receivers' perceptions of the quality of handover are institution-dependent.(17-20)
The present study had some limitations. There may have been some recall bias among the survey participants. The recipients' perceptions may have been influenced by their level of experience and the number of critical incidents they previously handled. Furthermore, conformity and fear of administrative identification may have also induced bias in the recipients' perceptions; however, the anonymity of the study design and survey forms reduced the possible impact of the risk of bias.
The present study showed that dual customisation of the handover process (PETS protocol and SBAR documentation) was necessary to meet the workflow and information demands of the receiving team. These changes were essential to improving interdisciplinary communication and delivery of vital information so as to optimise patient care upon arrival at the CICU. Variation in information demands between nurses and doctors must be taken into consideration in the handover process and SBAR handover document. Providing options such as 'none' and 'NA' reduces ambiguity and facilitates differentiation between an omission error and a lack of information. The PETS handover protocol introduced in this study was individualised from the KKH-CICU team's demands, perceptions and opinions. However, this protocol can still be adapted by other centres or units (e.g. emergency room, surgical ICU or neonatal ICU) that have the same set of requirements for handover. In addition, we suggest that further investigations be conducted to determine the efficiency of the PETS handover protocol and the efficacy of the SBAR handover document for long-term use in practice. Other research designs, such as a metric target observational study or reciprocate survey involving anaesthetists who are handing over the patient, can be used to close the loop.
SMJ-57-251-appendix.pdf


