Abstract
INTRODUCTION
Laparoscopic sleeve gastrectomy (LSG) outcomes among adolescents and factors associated with adolescent obesity in Singapore were evaluated.
METHODS
Prospectively collected data of patients aged 16–19 years who underwent LSG was retrospectively reviewed. A lifestyle questionnaire, Berlin and Epworth scores, and Patient Health Questionnaire-9 scores were collected. Preoperative anthropometrics, comorbidities, weight loss and body composition outcomes were recorded.
RESULTS
Among 208 LSGs, 13 (6.3%) were performed on obese adolescents. Mean age and body mass index (BMI) at first presentation were 19.1 ± 0.9 (range 16.8–19.8) years and 46.2 ± 6.3 (range 36–57) kg/m2, respectively. There was family history of obesity (n = 7) and regular consumption of high-calorie drinks (n = 12). Most patients had comorbidities (n = 12), including hypertension (n = 5), asthma (n = 4), diabetes mellitus (n = 3), hernia (n = 3) and obstructive sleep apnoea requiring continuous positive airway pressure support (n = 3). At one year, excess weight loss was 64.3% ± 34.7% (range 21.8%–101.5%), while BMI and fat mass dropped to 31.2 ± 7.6 (range 23–40) kg/m2 and 17.4 kg, respectively. Pain score was 2/10 at 24 hours after surgery. Mean postoperative stay was 2.7 days. No complications or readmissions occurred. Remission of diabetes mellitus and hypertension was reported in two of three and four of five adolescents, respectively, within one year of surgery.
CONCLUSION
LSG is a safe option for adolescents with good short-term weight loss outcomes and remission of metabolic comorbid conditions.
INTRODUCTION
Worldwide, the number of obese individuals has doubled since 1980.(1) Every year, approximately 3.4 million people die as a consequence of being overweight or obese, according to the World Health Organization.(1) The increased prevalence of adolescent obesity in affluent countries correlates with per capita income, and Singapore is no exception. Adolescent obesity is potentially one of the most serious health problems of the 21st century. Childhood obesity tends to persist into adulthood and poses a risk of developing into metabolic conditions, such as diabetes mellitus, hypertension and cardiovascular disease, at a younger age.(2-7) Obesity prevalence among persons in Singapore aged 18–69 years has increased from 6.9% in 2004 to 10.8% in 2010.(8) In adults aged 18–29 years in Singapore, 15.4% of men and 5.8% of women were obese (body mass index [BMI] ≥ 30 kg/m2) in 2010.(8)
Efforts at lifestyle modification and use of pharmacotherapy to improve the health of morbidly obese adolescents are often unsuccessful. As obese children and adolescents are predisposed to a range of obesity-related disorders during growth and have increased risk of adult obesity with associated cardiovascular risk, early treatment is therefore essential.(9,10) More adolescents and their families are seeking surgical treatment for morbid obesity because of a lack of response to behavioural, diet and medical treatment approaches.(11) Bariatric surgery is in demand worldwide and is gaining much support and acceptance in Asia.(12,13) Among morbidly obese adolescents, bariatric surgery has been associated with resolution of concomitant metabolic conditions.(14,15) The most commonly performed procedures are laparoscopic sleeve gastrectomy (LSG), laparoscopic gastric bypass and gastric banding.(16) Among these, sleeve gastrectomy is increasingly being utilised for morbidly obese adults and adolescents, and has been shown to be more effective than gastric banding for adolescents.(17) The premise for using sleeve gastrectomy rather than the latter two options includes the relative simplicity of the surgical procedure and lower risk of long-term complications.(18)
According to the American Society for Metabolic and Bariatric Surgeons (ASMBS), the number of adolescents who underwent bariatric surgery increased in the late 1990s. In 2005, among members of the ASMBS, 53% had performed bariatric surgery on obese adolescents. In 2003, more than 100 hospitals performed bariatric surgical procedures on obese adolescents, with a mean age of 16 years.(19) The Obesity Surgery Society of Australia and New Zealand has set criteria that adolescents aged 15 years and above with associated morbidity should be considered for obesity surgery.(11)
To our knowledge, there are only a handful of studies on bariatric surgery for morbidly obese Asian adolescents.(13,20-24) Our study sought to provide an overview of adolescent bariatric surgery in a multiethnic population from Singapore.
METHODS
Adolescents aged ≤ 19 years who underwent bariatric surgery (i.e. LSG) at National University Hospital, Singapore, from November 2010 to July 2014 were selected. We performed a retrospective analysis of the data, which was collected prospectively and entered into our database, as approved by the institutional review board (IRB no. NUH-2012/00114). A questionnaire was completed for each patient at first presentation to the obesity management clinic. Data on dietary, exercise, cigarette and alcohol habits, family history of obesity, and the Berlin questionnaire,(25) Epworth Sleepiness Scale scores(26) and Patient Health Questionnaire-9 (PHQ-9) scores(27) was recorded by specialist nurses. Demographic, anthropometric and postoperative outcomes were retrieved from the database. Variables such as age, gender, BMI before and after surgery, length of hospital stay, complications, absolute weight loss, percentage excess weight loss, changes in body composition and remission of comorbidities were recorded. Blood pressure, fasting blood glucose (FBG), glycated haemoglobin (HbA1c) and serum lipids were checked at each visit. Adolescents with hypertension, diabetes mellitus or dyslipidaemia were assessed for remission according to ASMBS guidelines.(28) The Tanita® body composition analyser (model TBF-300; Tanita Corporation, Tokyo, Japan) was used for all patients. Pain scores were recorded using the Visual Analogue Scale. Complications were defined as adverse events that required medical or surgical intervention after surgery.
Data analysis and visualisation was aided by Microsoft Excel version 2010 (Microsoft Corporation, Redmond, WA, USA), QI Macros® for Excel (KnowWare International Inc, Denver, CO, USA) and Daniel’s XL Toolbox add-in for Excel version 6.60 (Daniel Kraus, Würzburg, Germany) software packages. Weight-related calculations, including BMI, were reported as mean ± standard deviation. A one-tailed paired t-test was used to compare preoperative and one-year postoperative mean body composition measurements, changes in blood pressure and serum lipid indices. Statistical significance was set at p < 0.05.
RESULTS
The eight boys and five girls who underwent LSG (n = 13) had a mean age of 19.1 ± 0.9 (range 16.8–19.8) years at the first visit to the weight management clinic. This patient group constituted 6.3% of a total of 208 LSG procedures performed at our institution during the study period. Ethnically, the patients were Chinese (n = 6, 46.2%), Indian (n = 4, 30.8%) and Malay (n = 3, 23.1%).
Table I
Behavioural and lifestyle variables associated with adolescent obesity (n = 13).
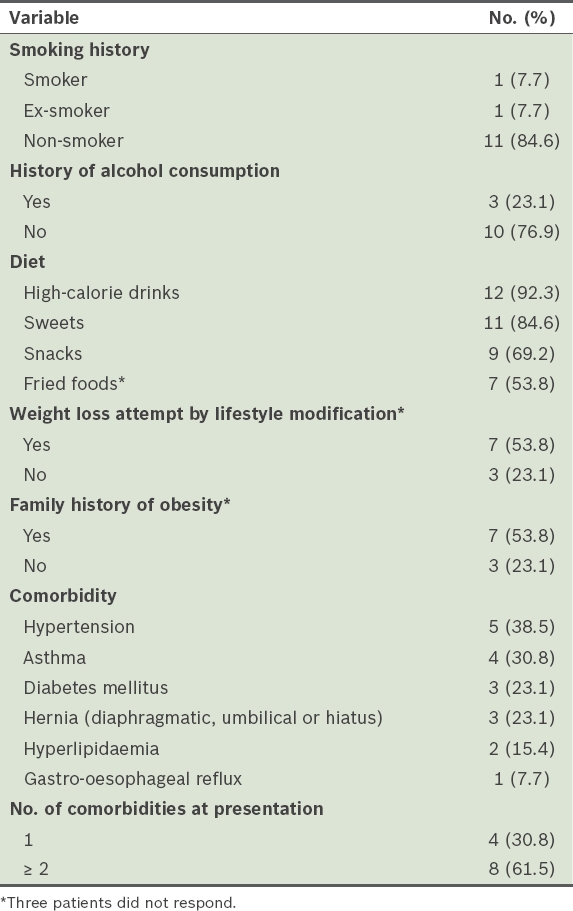
At presentation, 4 (30.8%) patients had one comorbid condition while 8 (61.5%) patients had two or more comorbidities. Hypertension, diabetes mellitus, asthma, hyperlipidaemia and hernia were observed (
The mean length of postoperative hospital stay was 2.7 (range 2–4) days. All patients ambulated freely on the first postoperative day and drank clear fluids within 24 hours of surgery. There were no mortalities, complications or reoperations to report. The mean pain score at 24 hours after surgery, recorded for eight of 13 patients, was 2 out of 10.
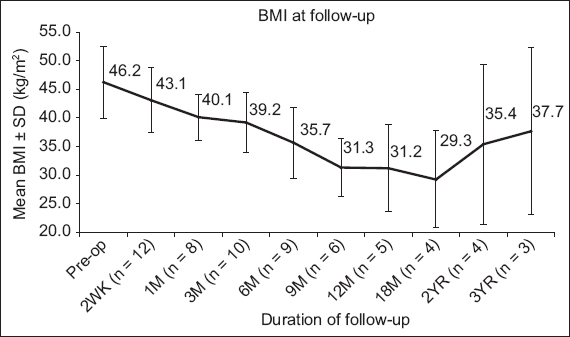
Of 13 patients, 5 (38.5%) completed the one-year review, and 3 (23.1%) completed three years of follow-up. At one year, the mean absolute weight was 39.3 kg lower than that before surgery (
Fig. 1
Mean absolute weight loss of obese adolescents after surgery. M: month; SD: standard deviation; WK: week; YR: year
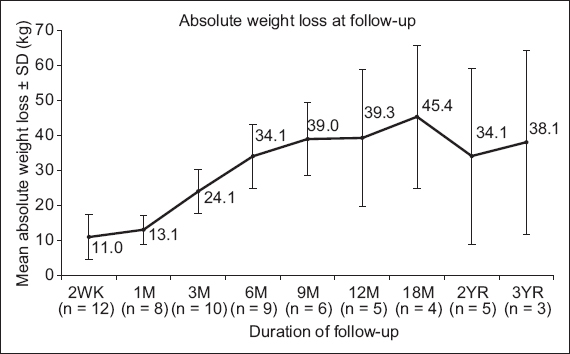
Fig. 2
Mean percentage excess weight loss of obese adolescents after surgery. M: month; SD: standard deviation; WK: week; YR: year
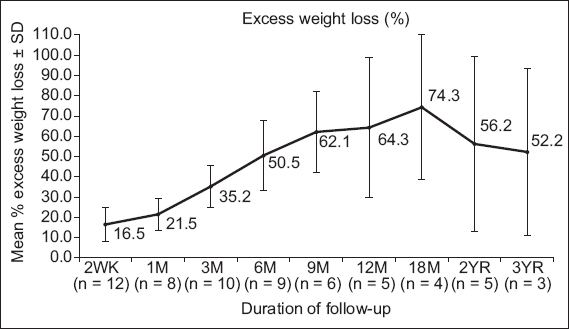
Fig. 3
Mean body mass index (BMI) of obese adolescents before and after surgery. M: month; preop: preoperative; SD: standard deviation; WK: week; YR: year
Apart from weight loss, we found substantial changes in body composition one year after surgery.
Table II
Changes in body composition of obese adolescents after surgery.
According to ASMBS outcome reporting standards,(28) full remission of diabetes mellitus is declared if FBG < 5.5 mmol/L and HbA1c < 6.5% in the absence of diabetic medications. Of the three diabetic adolescents who underwent LSG, two discontinued antidiabetic medications following surgery – one had complete remission at six months (FBG 4.3 mmol/L, HbA1c 5.3%) and the other had improvement at three months (FBG 5.3 mmol/L, HbA1c 6.7%), with recurrence later.
With regard to hypertension before surgery, according to ASMBS guidelines, five patients had prehypertension (systolic blood pressure [SBP] 120–139 mmHg, diastolic blood pressure [DBP] 80–89 mmHg), three had Stage 1 hypertension (SBP 140–159 mmHg, DBP 90–99 mmHg) and one had Stage 2 hypertension (SBP ≥ 160 mmHg, DBP ≥ 100 mmHg). Two patients proceeded to complete remission by one year (
Table III
Systolic and diastolic blood pressure values of hypertensive or prehypertensive adolescents (n = 9) before and after surgery.
Fasting serum lipid evaluation demonstrated significant reductions in triglycerides (p = 0.01) and total cholesterol/high-density lipoprotein (HDL) ratio (p < 0.01), and a significant increase in HDL cholesterol (p = 0.02) at one year (
Table IV
Fasting serum lipid analysis of obese adolescents before and after surgery.
Table V
ASMBS categories of dyslipidaemia among obese adolescents before and after surgery.
DISCUSSION
Our study sought to determine the outcomes of LSG in an obese adolescent population from Singapore. The study’s many strengths included its prospectively collected data, definitive follow-up schedules and treatment protocols. The finding of metabolic improvement highlights the clinical significance of LSG for treating not only obesity but also inducing remission of associated comorbidities, which is arguably more important. Long-term outcomes of sleeve gastrectomy in adults indicate that, on average, more than 60% excess BMI loss is maintained at over ten years from surgery, even as de novo gastro-oesophageal reflux occurred in 8% of patients in Europe.(30) Similar findings have been reported at five years in Asia.(31) These recent findings, published after the completion of our study, attest to the durability of the procedure in adults. While our cohort showed excellent excess and absolute weight loss, and improvement in BMI at 12 and 18 months, the results at three years were not as good.
After LSG, effective weight loss was achieved in morbidly obese adolescents in our study, with effective resolution of comorbidities. We suggest early postoperative weight-bearing exercise to prevent muscle loss in this group. The initial apparent rise in fat mass, body fat percentage and basal metabolic rate represents a change in the body’s electrical resistance, as measurements were made using bioelectrical impedance. Impedance calculations are based on total body water, and intracellular and extracellular water values.(32) Changes in the water-electrolyte balance of tissues, along with acute changes in body mass, are limitations of the use of bioelectrical impedance.(32) A reduction in total body water was noted in each participant at the two-week review.
A decrease in fat-free mass was also noted in our series. Fat-free mass constitutes not only muscle mass but total body water, bone density and minerals.(15) Supplementation of vitamins and minerals is compulsory to minimise the risk of nutritional deficiency.(15,33) Although the values for fat-free mass at two weeks may relate to total body water, protein catabolism in the first month may be more rapid than fat catabolism. By one year, the values for reduction in fat mass and fat-free mass converge. This reflects the nutritional status of bariatric patients after surgery and suggests a need for better support infrastructure and more early advice to prevent muscle loss. Regular follow-up after surgery is compulsory for active weight management,(11) and we also advocate resistance exercise to preserve muscle mass. Fat-free mass helps to dispose of excess nutrients, such as glucose, and is preserved by having adequate intake of proteins and regular exercise as part of an active lifestyle.
Ensuring the safety of LSG is a concern for adolescent patients, family and healthcare providers. Like other studies, the cases in our series had an absence of complications and rapid recovery enabling early discharge from hospital. Results from a series of 108 paediatric and adolescent patients from King Saud University Hospitals in Riyadh, Saudi Arabia, demonstrated LSG to be a safe and effective procedure.(21) A series of 22 patients from Korea reported the high rate of resolution of comorbidities.(20) Our institution keeps abreast of the outcomes of local and international adolescent bariatric surgery and constantly studies the risks and benefits of these procedures. Long-term results in this category of treatment, such as this study and efforts at other institutions, will explore the sustainability of bariatric surgery.(34) For obese adolescents, the effectiveness of bariatric surgery is well established. Among the different surgical options, LSG has become more popular in recent years due to good outcomes and its perceived simplicity when compared with other bariatric procedures such as laparoscopic biliopancreatic diversion with duodenal switch and Roux-en-Y gastric bypass.(35) Additionally, LSG may be followed by gastric bypass for further weight loss, if required.(36) Possible long-term nutritional risks, sustainability of weight loss and resolution of comorbid conditions should be adequately evaluated.(3) Questions still exist about how families can best support such lifestyle changes.
Psychopathologies are common in obese adolescents, and depressive disorder symptoms were observed among 66.7% of our cohort, which is at the higher end of the 15%–70% range noted in the literature.(37) Meanwhile, the reported ranges for anxiety disorder and eating disorder symptoms are 15%–33% and 48%–70%, respectively, prior to surgery, although these symptoms improve considerably after surgery.(37) If lifestyle modifications fail after surgery, those adolescents would gain weight despite the metabolic modification effects of surgery. The durability and efficacy of this surgery in young adults are partly dependent on the motivation of patients to adhere to the postoperative dietary and lifestyle regimens that are necessary to maintain the success of the weight loss procedure.
This study was not without limitations. Although we only had 13 patients, with over 50% being lost to follow-up at one year and further attrition noted at three years, the study provided preliminary data for early outcomes of LSG that may be valuable for future studies. The rate of loss to follow-up may reflect a satisfactory outcome in a majority of cases, adding a negative bias to the results, and efforts to counteract attrition should be considered when planning future surgery and studies. In particular, comorbid conditions would benefit from higher attendance at follow-ups, including an assessment of sleep apnoea remission. Medium- and long-term follow-up for this cohort would broaden the literature on the topic. Second, while we observed a trend of considerable changes in body composition in our cohort, the one-year values for body composition were elevated by one outlier. This outlier was neither typical of the cohort nor the trend for each individual and, consequently, statistical significance was lacking. Third, the role of the families and social groups of these adolescents should be mentioned. While parental concern about their adolescent wards’ conditions was noted, preoperative and postoperative psychological evaluations of parents and other family members were not performed. Additionally, the postoperative prevalence of depression could have been assessed among participants as a group. However, as ASMBS paediatric guidelines suggest the involvement of a mental health specialist for children,(29) these adolescents were referred for such care when appropriate.
In conclusion, most morbidly obese adolescents in Singapore who undergo bariatric surgery have obesity-related comorbidities at presentation. Common dietary habits include high-calorie drinks and foods. A family history of obesity is often present and attempts at weight loss via lifestyle modifications are unsuccessful. Our preliminary data showed that bariatric surgical intervention is a safe option for weight loss for obese adolescents in Singapore, with some resolution of associated comorbidities at one year after LSG.


