Abstract
INTRODUCTION
This study aimed to describe the planning, development and evaluation of the success of the first nationwide, resident-led, large-group teaching programme for medical students – the Singapore Health Services Student Internship Programme (SIP) Bootcamp.
METHODS
This was an initial feasibility study evaluating a half-day teaching boot camp initiated, developed and conducted by the resident educators. A three-month preparation period was required to set up an education subcommittee, liaise with medical student leaders, recruit resident educators, meet all the stakeholders and conduct the boot camp. During the SIP Bootcamp, resident educators conducted clinical case presentations using a question-and-answer format. Audience participation was strongly encouraged. A 15-item questionnaire was distributed to assess the participants' learning experience and the resident educators' teaching performance using a five-point Likert scale.
RESULTS
Overall, 94.8% (n = 110) of the 116 respondents agreed that the teaching sessions were of high quality and content was relevant to their training. The resident educators appeared well-informed (96.6%, n = 112) and enthusiastic about their respective topics (98.3%, n = 114). However, a few students (9.5%, n = 11) felt that the audio-visual aids and handouts could be improved to better aid their learning process.
CONCLUSION
This teaching boot camp for medical students was the first of its kind in Singapore and feedback from medical students showed that it was well-received. Further research using different teaching methods, including small-group discussions and surgical practical sessions by resident educators from different specialties, would be of great value to students.
INTRODUCTION
In 2010, Singapore switched from the British-based postgraduate medical training system (basic and advanced specialty training) to the American-based residency system under the Accreditation Council for Graduate Medical Education International (ACGME-I). All three sponsoring institutions including Singapore Health Services (SingHealth), the National University Health System and National Healthcare Group made this switch. Under the ACGME-I framework, all residents are expected to achieve competence in the following six core competencies: (a) patient care; (b) medical knowledge; (c) interpersonal and communication skills; (d) professionalism; (e) practice-based learning and improvement (PBLI); and (f) system-based practice.(1) As part of the PBLI component, all residents are expected to acquire essential teaching skills in order to improve in the areas of teaching and patient care.(1)
It is crucial to cultivate a strong teaching culture among residents early in their career. This may help improve their leadership and problem-solving skills through the discussion of case scenarios with medical students.(2) Contrary to the commonly held perception that attending physicians are better suited to teach medical students, residents believed that teaching was integral to their training and resident-led teaching was beneficial to medical students, especially in the context of a busy clinical setting.(3) Teaching in the clinical setting, small-group tutorials and large-group didactic sessions enable the residents to reinforce previously learnt information. In addition, teaching helps medical students to apply their theoretical knowledge to a clinical setting. Medical students are also generally more satisfied with their clerkship experience as they find it easier and more accessible to learn from resident educators in the hospital setting.(4) In the United States, a five-day surgical boot camp for senior medical students was shown to have improved young doctors' self-confidence in many areas of perioperative care, particularly in high-risk, infrequently performed technical tasks.(5) Furthermore, a boot camp is also an effective way to assess residents' needs during the early phase of their residency training.(6) In Scotland, near-peer teaching programmes were set up by a group of junior doctors to help facilitate practical and small-group teaching for medical students.(7) With adequate training, junior resident educators can be a ready resource for teaching relevant bedside material to medical students.(8)
At present, there are three medical schools in Singapore, namely the National University of Singapore Yong Loo Lin School of Medicine (NUS Medicine), Duke-National University of Singapore (Duke-NUS) Medical School and Lee Kong Chian School of Medicine. All medical students in Singapore spend their final year of medical school in the student internship programme (SIP), which rotates them to the different major specialties (e.g. internal medicine, general surgery, obstetrics and gynaecology, paediatrics, etc). The medical student functions as an intern and is part of the medical or surgical team during this 'preinternship' year.
Traditionally, residents conduct ad-hoc tutorial sessions based on the medical students' requests, in addition to formal teaching provided by lecturers in the university and hospital setting. Previous informal feedback reported that, as the residents were generally very approachable, medical students felt that they could learn well in the more comfortable and less fearful environment. Nevertheless, the teaching faculty or programme directors did not vet the teaching content and no formal documentation of the medical students' experience during these teaching sessions was available. Hence, the Education Subcommittee of the SingHealth Residents' Committee decided to spearhead an inaugural nationwide, resident-led, large-group teaching programme for medical students in Singapore. The purpose of our study was to describe the planning, development and evaluation of the success of the nationwide SIP Bootcamp. This teaching boot camp is an interactive teaching initiative that aimed to improve medical students' knowledge of the management of real patients during their clinical training and hone the teaching skills of resident educators.
METHODS
The nationwide, half-day teaching programme was organised for medical students of NUS Medicine and Duke-NUS in 2013. The four-hour boot camp took place at Singapore General Hospital, SingHealth, Singapore, and covered major surgical specialties such as general surgery, obstetrics and gynaecology, orthopaedics, and paediatric medicine.
Preparation for the boot camp started approximately three months prior to the actual day and was led by the head of the Education Subcommittee of the SingHealth Residents' Committee. Numerous stages of planning were required in order to maximise the experience of both the learners and teachers, and therefore ensure the success of the teaching boot camp. The stages included: (a) setting up an education subcommittee; (b) liaising with medical student leaders; (c) recruiting resident educators; (d) organising a meeting with all the stakeholders; and (e) organising the boot camp on the actual day. The Education Subcommittee comprised ten resident educators of different subspecialties, such as ophthalmology, family medicine, anaesthesia and those previously mentioned. These members were chosen by the head of the Education Subcommittee based on their previous education track record, as provided by their respective programme directors. Six resident educators were involved in the teaching boot camp, whereas the remaining four residents were involved in logistical and administrative matters.
After setting up the organising committee, the specialties to be included in the boot camp were decided. Internal medicine was not included as part of the programme, as its teaching programme was conducted separately by internal medicine residents in the small-group tutorial format. We selected three surgical disciplines and paediatric medicine based on student leaders' requests. Student leaders from both NUS Medicine and Duke-NUS felt that their curriculums were generally well-developed and -designed, but that the boot camp would be a beneficial platform for them to learn various case-based scenarios from the resident educators.
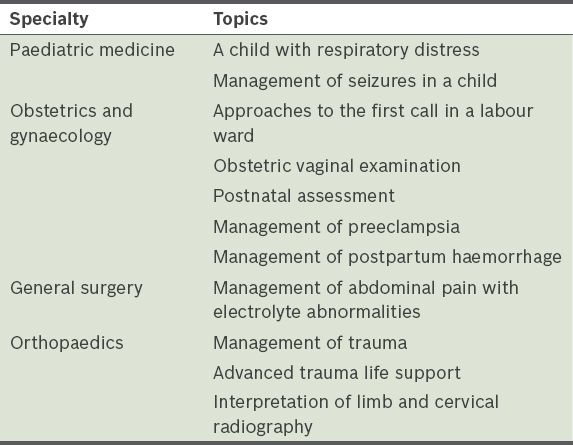
The resident educators, selected from their respective specialties (obstetrics and gynaecology, paediatric medicine, general surgery, and orthopaedics), were all identified as top performers in their specialties based on recommendations from their programme directors. They were required to develop and prepare their teaching plan, content and materials, then discuss the teaching content with core faculty and programme directors. These measures were taken to ensure the delivery of high-quality teaching and avoid teaching medical students incorrect information. Resident educators were each allocated one hour to deliver their topics, so as to avoid overwhelming the medical students with too much information, as well as train residents to deliver focused presentations of the most salient points about each condition. The topics selected by the resident educators and their respective programme directors focused primarily on the recognition of 'red flags' and management of surgical and paediatric emergencies (
Table I
Topics delivered by individual resident educators from paediatric medicine, obstetrics and gynaecology, general surgery, and orthopaedics.
Help was sought from the Graduate Medical Education (GME) Office for the booking of the venue, event publicity, and catering of food and beverages. An electronic poster was designed and disseminated through the medical students' portal in both NUS Medicine and Duke-NUS. The teaching boot camp was optional and open to medical students from all three medical schools.
On the day of the boot camp, resident educators conducted didactic lectures in combination with interactive sessions. Audience participation was strongly encouraged throughout the whole session. At various points during the case presentations, resident educators would actively engage the students by questioning them on history taking and clinical examination technique. In addition, the students were asked to interpret blood test results and imaging results (radiographs of the chest and abdomen and computed tomography scans of the abdomen); they were also asked to present a diagnosis and appropriate management plan.
At the end of the boot camp, the students were given a questionnaire on the residents' teaching performance, appropriateness of the content and quality of the teaching programme. The feedback questionnaire consisted of 15 questions on a five-point Likert scale (1 = strongly disagree, 5 = strongly agree). All data was analysed using SPSS Statistics version 17.0 (SPSS Inc, Chicago, IL, USA). This study was conducted in accordance with the Declaration of Helsinki, with an exemption for ethics approval from the SingHealth Institutional Review Board.
RESULTS
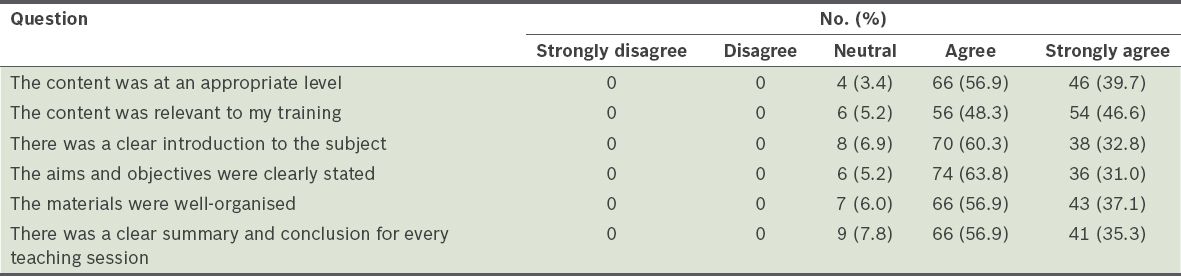
A total of 145 medical students attended the boot camp. Of these participants, 80.0% (n = 116) responded to the questionnaire. Most students felt that the content was delivered at an appropriate level (96.6%, n = 112) and relevant to their training (94.8%, n = 110). The majority agreed that the introduction, aims and objectives of the topics covered by each specialty were clearly stated, the flow of the presentation was well-organised, and there was a clear summary and conclusion for each teaching session (
Table II
Feedback from medical students on the teaching content of the Student Internship Programme Bootcamp (n = 116).
The medical students generally had positive feedback on the residents' medical knowledge (96.6%, n = 112) and enthusiasm (98.3%, n = 114) for their presentations (
Table III
Feedback from medical students on the teaching performance of the residents (n = 116).
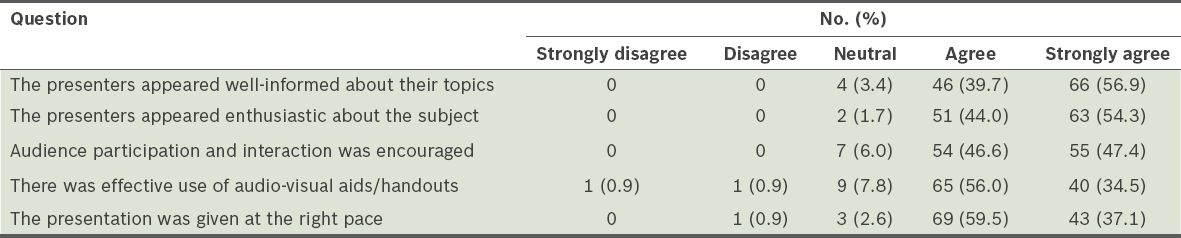
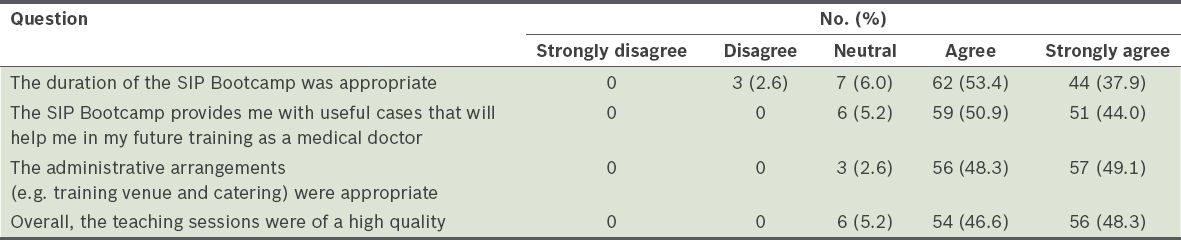
Table IV
Feedback on the medical students' overall experience with the Student Internship Programme (SIP) Bootcamp (n = 116).
DISCUSSION
The SIP Bootcamp was the first nationwide, large-scale, resident-led teaching programme for medical students in Singapore. It was a platform for residents to hone their teaching, collaboration and organisational skills, while medical students had the opportunity to learn in interactive sessions. Providing residents with sufficient depth of teaching skills is a challenge that medical schools and residencies currently face. Obstacles in administering teaching skills programmes for residents include the complexity of resident schedules, work-hour limitations and resident rotations at multiple clinical sites.(9)
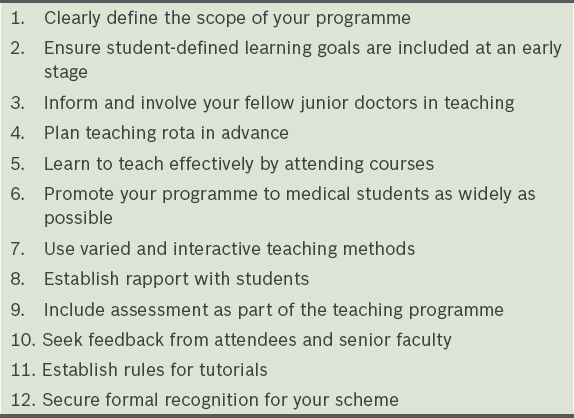
Mabvuure et al recommended 12 tips to run a successful junior doctor-led teaching programme for medical students (
Undergoing the actual clinical experience or sub-internships is always the best way to increase medical students' clinical competency. The boot camp was conducted with the aim of creating an interactive question-and-answer session using case-based scenarios that simulated the real clinical environment. Due to the available resources, teaching was performed through the use of clinical case presentations. It was also considered more manageable to organise a teaching boot camp that involved six resident educators and more than 100 medical students in a large auditorium. Nevertheless, future research aims to expand the boot camp to involve more specialties using different formats (e.g. small-group discussions and practical sessions).
Our results showed that the majority of students felt that the contents of the presentations were set at an appropriate level and, most importantly, found the teachings relevant to their medical training. From the informal feedback, we found that some medical students had difficulty applying their theoretical knowledge in a clinical situation. This boot camp was structured to provide them with a simulated clinical environment, giving them the confidence and competency to manage real patients during their clinical training.
This boot camp was initiated by a group of residents from the SingHealth Residents' Committee. They developed the concept, teaching programme and logistics with the support of programme directors, faculty and the GME Office. Student leaders from both NUS Medicine and Duke-NUS were invited to give feedback during the developmental process on the content and type of learning that they felt would be useful to them and was lacking in their medical school curriculum at the time. Such collaboration between residents from various specialties and medical student leaders is not common in routine clinical medicine. The opportunity offered by the SIP Bootcamp was unique and encouraged discussion and collaboration among potential future leaders in the healthcare service.
In order to engage the medical students, the presenters were advised to prepare their slides in the format of case-based scenarios and encourage audience participation throughout their talks, as students generally find it easier to learn in an interactive environment.(11) Medical students were given opportunities to ask questions during and at the end of each lecture, and lecture notes were distributed to them at the end of each session. The participant feedback questionnaire found that most students felt that the presentations were given at the right pace and presenters were enthusiastic about their subject; this suggests that this method of faculty-supervised development of teaching plans and content with residents is useful and facilitates the building of a successful teaching programme.
The SIP Bootcamp was a half-day, national, medical student teaching programme that ran for four hours. In Scotland, a well-established near-peer teaching programme involves various junior doctors as resident educators.(7,8) It started in 2006 as one programme (73 tutorials conducted by 18 tutors) and has now expanded to four programmes (324 tutorials conducted by 108 tutors), run throughout the year and focusing on bedside teaching. This is another teaching method that we may be able to implement in the future as part of the national teaching programme for medical students.
The overall mission of the World Federation for Medical Education is to promote the highest scientific and ethical standards in medical education, initiation of new learning methods and instructional tools, and innovative management of medical education.(12) Continuing medical education or continuing professional development (CPD) is routine in most healthcare systems around the world. CPD often implies self-directed and practice-based learning activities to maintain and develop competencies of individual doctors. Hence, residents should be encouraged to engage in more teaching activities as part of CPD activities throughout their medical career.
Kirkpatrick's Learning Evaluation Model, designed to evaluate training programmes,(13) contains the following four levels: (a) reaction – how the learners thought and felt about the teaching programme; (b) learning – the resulting increase in knowledge; (c) behaviour – application of the learning; and (d) results – the effect on the environment due to improved performance. In our study medical students were evaluated using the first level of the model. Future studies, using the model's subsequent levels, would be of great value to assess the impact of the teaching programme.
There were some limitations to our study. There was a lack of benchmark comparisons and preassessments of the needs of medical students from both universities. In addition, the academic effect of this teaching programme was not assessed. We did not compare the medical students' knowledge before and after the programme, as we did not want it to cause stress to the participants. Another limitation of the study was the lack of formal feedback from the resident educators themselves and their peers about their teaching during this programme. Self-reflection on residents' teaching experience could have been included as a formative assessment. Medical teachers should take responsibility for their personal CPD and regularly assess and review their own competence.(14) A longitudinal follow-up study on the subsequent teaching efforts of each of these residents can also help to build their teaching portfolio as they pursue the clinician-educator track.(15)
Even though our study found that the teaching quality was high and would be helpful to medical students' future training, this was only based on self-reported feedback. These medical students may be too junior to decide if the knowledge delivered would make any impact on their future training. Another limitation is the lack of self-assessment, as well as learner, peer and faculty assessments, of the teaching skills of the resident teachers.(16,17) A validated tool like the Stanford Faculty Development Programme (Form 26) has been widely used to evaluate the teaching knowledge, skills and attitudes of resident teachers.(18) To improve future SIP boot camps, it would be of great value to distribute separate questionnaires to medical students and resident educators during a subsequent teaching programme to collect feedback from participants and teachers.
In conclusion, this SIP Bootcamp was the first nationwide, large-scale, medical students' teaching programme led by residents in Singapore. It is an excellent platform to foster camaraderie among residents from various specialties and medical student leaders, and to train residents to be organisers and medical educators. Even though only four specialties were covered in this boot camp, it was a good start with excellent feedback from a large number of medical students. We hope to increase the recruitment of both medical students and resident educators in the coming years.
ACKNOWLEDGEMENTS
We would like to thank all the resident educators involved in this project, including Dr Celene Hui (obstetrics and gynaecology), Dr Katrina Heng (paediatric medicine), Dr Mark Cheah (internal medicine), Dr Sim Yi Rong (general surgery) and Dr Hamid Rahmatullah (orthopaedic surgery). In addition, this boot camp would not have been successful without the financial, administrative and manpower support from the SingHealth senior management and GME Office. Last but not least, we would also like to express our sincere gratitude to the SingHealth Residents' Committee, NUS Medical Society and Duke-NUS Student Council for helping us publicise this event to residents and medical students.
The study findings were presented at the ACGME Annual Education Conference 2014 in Maryland, USA.