Dear Sir,
In Singapore, the prevalence of moderate to severe obstructive sleep apnoea (OSA) is estimated at a high of 30.5%.(1) First-line treatment of OSA is continuous positive airway pressure (CPAP), but patient acceptance and tolerance as well as treatment adherence are poor.(2) A local study suggested that these factors may be contributed by craniofacial differences in Asian populations, which can result in ill-fitting masks and patient discomfort.(3)
OSA phenotyping is an active area of research to identify treatable traits in OSA. Positional OSA (POSA) is an OSA phenotype where breathing abnormalities are worse when patients sleep in the supine position. For these patients, targeted therapy with positional therapy may be an attractive strategy, given the challenges of CPAP treatment. Hence, we conducted a study to elucidate the prevalence of POSA, which is currently unknown, in our local OSA patients.
This is a retrospective observational study of subjects who underwent an overnight diagnostic polysomnography at Changi General Hospital, a tertiary 1,000-bed hospital in Singapore, from 1 January 2016 to 31 August 2018. All patients aged above 15 years who were diagnosed with OSA (defined as Apnoea-Hypopnoea Index [AHI] ≥ 5) were included. Subjects with total sleep time < 4 hours, supine sleep time < 15 minutes or non-supine sleep time < 15 minutes were excluded. Apnoea was defined as ≥ 90% drop in airflow ≥ 10 seconds. Hypopnoea was defined as ≥ 30% drop in nasal pressure signal, with either oxygen desaturation ≥ 3% or arousal.(4) POSA was defined as AHI ≥ 5 and supine AHI/non-supine AHI ≥ 2, with at least 15 minutes of supine sleep time and 15 minutes of non-supine sleep time.(5) Baseline demographics and sleep study data were obtained from electronic medical records (
Table I
Characteristics of patients with non-positional and positional OSA (n = 1,031).
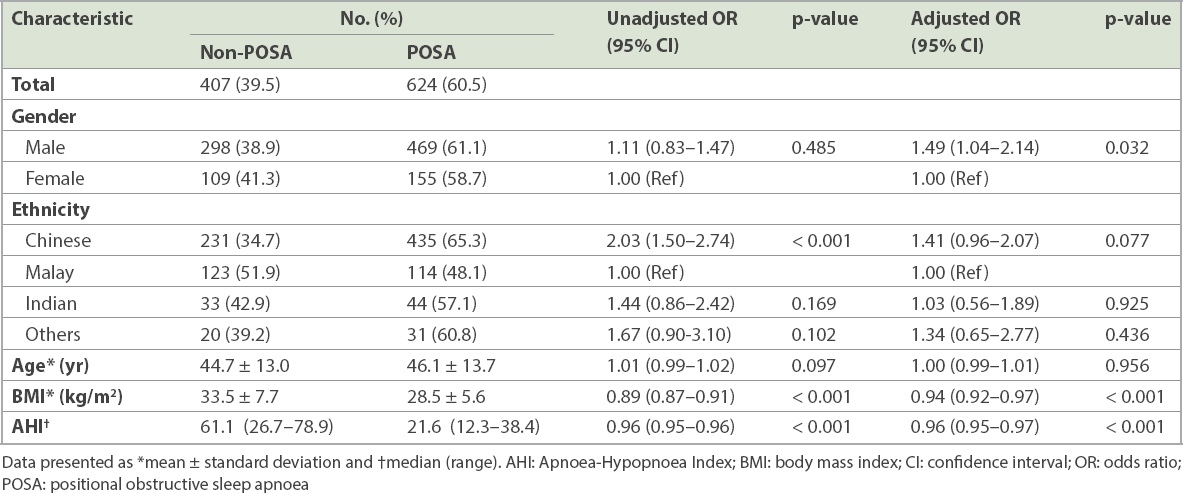
The prevalence of POSA among our local OSA patients presenting to a tertiary hospital was 60.5% (624/1,031; 95% confidence interval 57.5%–63.5%). This prevalence is much higher than a previously reported 27.4% in a Caucasian population.(6) Lower body mass index and AHI were found to be significant predictors of POSA (adjusted p < 0.001), which are consistent with previous reports.(7) In our study, ethnicity was also associated with POSA, with Malays having the lowest prevalence (adjusted p = 0.077). In our multivariate analysis, males were 1.5 times more likely to have POSA (adjusted p = 0.032) compared to females.
Our study has its limitations. As information on neck circumference and Epworth Sleepiness Scale scores was not systemically recorded, it was not included in our analysis. Selection bias may exist, as our study is limited to OSA patients presenting to a tertiary public hospital. However, as the majority of Singapore’s OSA patients are managed at sleep centres in public hospitals, we believe our result is representative of the true prevalence of POSA in our local OSA patients.
This is the first local data to demonstrate a high prevalence of POSA among OSA patients presenting to a tertiary centre. Hence, many of Singapore’s OSA patients may be potential candidates for targeted positional therapy. New vibratory positional devices have also been invented recently but are currently unavailable in Singapore.(8) More studies are necessary to explore targeted treatment strategies for our local POSA patients.
Yours sincerely,


