Megan, an 18-month-old toddler, was taken to your clinic by her mother for a routine well-child visit. She was a cheerful and sociable child. Her developmental milestones were appropriate for her age and she was otherwise fit for vaccinations. Her height and weight were measured, and she was noted to have a body mass index-for-age of > 90th percentile. Apart from appearing chubby, Megan was not dysmorphic, and the rest of the physical examination was normal.
WHAT IS OBESITY?
Obesity is the excessive accumulation of fat, resulting in adverse health consequences. It is a major risk factor for cardiovascular diseases, which is a leading cause of morbidity and mortality worldwide.
Obesity is the result of a relative excess of energy intake compared to output. Both genes and environmental factors contribute to obesity, with behaviour and environment influencing the development of obesity in genetically-at-risk individuals. It is a growing epidemic worldwide, affecting both developed and developing countries. The World Health Organization (WHO) estimates that in 2016, 39% of adults worldwide aged 18 years and above were overweight, while 13% were obese.
Obesity is no longer just an adult disease. Globally, among children and adolescents aged 5–19 years, the prevalence of overweight and obesity has increased from 4% in 1975 to 18% in 2016. Obesity in childhood not only puts children at risk of obesity-related childhood conditions, but also has the long-term effect of predisposing them to adult obesity and non-communicable diseases related to obesity, such as diabetes mellitus, hypertension and osteoarthritis in adulthood.
The first 1,000 days – the period from conception to two years of age – is an important period of development, which is increasingly being recognised as a stage that affects an individual’s risk for developing obesity later on in life.(1) At this stage, taste preferences, dietary habits and lifestyle behaviours start forming, and are easily retained in later life. Interventions at this early stage can help to alter this course before the child’s preferences and habits become entrenched.
HOW RELEVANT IS THIS TO MY PRACTICE?
In Singapore, obesity among children aged 6–18 years rose from 11% in 2013 to 13% in 2017.(2) Results of a survey released in 2017 showed that 70% of children who were overweight at seven years of age continued to be overweight as adults.(3)
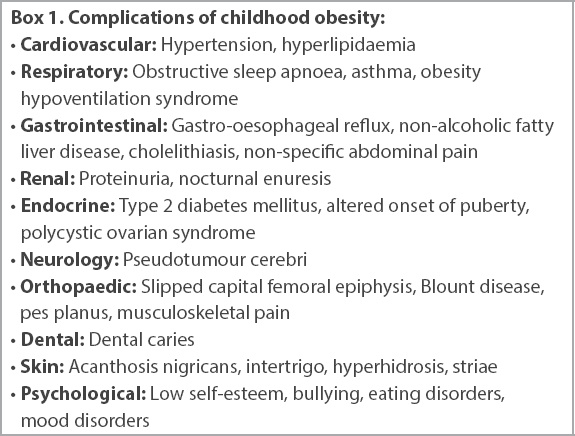
Childhood obesity affects both the physical and mental well-being of the individual (
Box 1
Complications of childhood obesity:
WHAT CAN I DO IN MY PRACTICE?
Primary care providers, with our experience in preventive care, play a central role in the fight against obesity. Starting from the child’s newborn years, frequent encounters for well-child visits and acute conditions present numerous opportunities for the healthcare provider to monitor a child’s growth, identify weight issues early and take action as necessary.
Obesity is an intergenerational condition where the need for intervention to address complications intersects with the social determinants of obesity. This can result in an emotionally sensitive situation for families in a healthcare setting. A child’s chubbiness may be viewed as acceptable, or desirable and reflective of the caregiver’s caregiving abilities. Primary care providers thus need to approach the topic of overweight and obesity in a sensitive, non-judgemental and non-stigmatising manner while highlighting the risks of future health consequences.
The family doctor is well placed to address the psychosocial and cultural aspects of feeding, nutrition and weight, and provide family-focused intervention for the child with a high body mass index (BMI), which is preferred over a patient-focused approach. This not only benefits the at-risk child, but also indirectly helps other members of the family to adopt a healthier diet and lifestyle.
Monitor a young child for obesity
Parental perceptions of the weight status of overweight (and underweight) children have been found to be inaccurate. Hence, objective measures are important for growth assessment, rather than relying on visual or verbal descriptions.(4) Children should have their height (or length), weight and BMI measured and plotted on the corresponding growth charts in their health booklets, which have been derived from population norms. Children aged two years and below should have their height and weight measured every 3–4 months, while those above two years of age should be measured every 6–12 months.(5)
For children in Singapore aged 6–18 years, the Health Promotion Board defines BMI > 90th percentile as overweight, while BMI > 97th percentile is considered severely overweight (obesity equivalent). For those aged two years and below, there is currently no consensus on what defines overweight and obesity. However, rapid weight gain in the first two years of life has been recognised as a risk factor for subsequent obesity.(6) Hence, longitudinal plotting of BMI-for-age on the health booklet growth charts serves as a valuable risk assessment tool. The WHO Child Growth Standards for children aged 0-59 months may also be used, where a z-score of > 2.0 and > 3.0 is defined as overweight and obese respectively.
Approach to an overweight/obese child in primary care
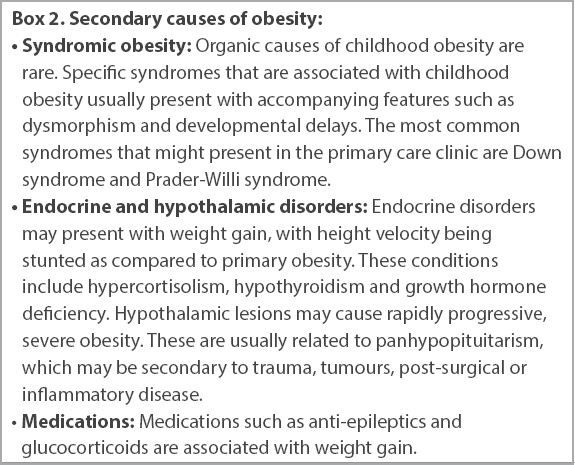
When approaching an overweight or obese child in primary care, a careful repeat measurement of the child’s height and weight should first be done, using the WHO recommended guide on measuring a child’s growth (see Useful Links), to ensure accurate measurement. Next, a review of the child’s medical history should be conducted, together with a physical examination, to identify secondary causes of high BMI that require specialist management (
Box 2
Secondary causes of obesity:
After secondary causes are excluded and/or addressed, the next step would be to look into the child’s nutrition and activities. The aim in the management of childhood obesity is commonly not for weight loss, but to control the rate of weight gain through preventive steps and behaviour modification to close the gap between excessive energy intake and insufficient energy expenditure.
Nutrition
Breastfeeding should be encouraged for as long as possible. The WHO recommends exclusive breastfeeding for the first six months, followed by complementary food with breastfeeding until the child is two years and older.
There are several reasons why breastfeeding is preferred to formula feeding in the prevention of childhood obesity. When compared to breastfed infants, formula-fed infants have a faster growth curve. Formula milk may be higher in energy and protein compared to breast milk. In addition, the composition of breast milk has been found to vary with the nutritional needs and feeding patterns of the child. Latching, as opposed to bottling, has also been suggested to allow better regulation of the infant’s own appetite. For these reasons, formula-fed infants could be at a higher risk than their breastfed counterparts of developing obesity later in life.(1)
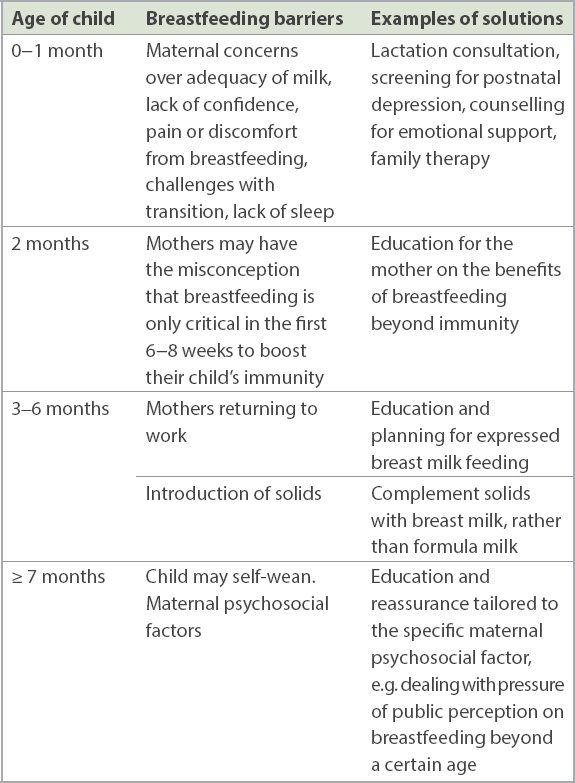
Mothers may choose not to breastfeed or discontinue breastfeeding early for various reasons.(7) While breastfeeding initiation rates are high with about 99% of new mothers breastfeeding, subsequent continuation of breastfeeding may not be sustainable after hospital discharge. Singaporean mothers with a lower education level were found to be at an increased risk of terminating breastfeeding compared to those with higher education.(8) A mother’s perception of breastfeeding was also found to be predictive of continued breastfeeding after six months.(9) Knowledge of these predictive factors can help clinicians to identify challenges faced by different mothers, so that personalised support and education may be offered.
Table I
Common reasons for discontinuing breastfeeding and recommended advice.
While complete breastfeeding is ideal, there may be instances where a mother is unable to or chooses not to breastfeed. Iron-fortified formula milk is a suitable alternative for most healthy, full-term infants up to one year of age. Formula milk should be prepared according to the manufacturer’s instructions (i.e. avoid overconcentration), and infant rice cereals should not be mixed into the milk bottle. Caregivers should be sensitive to the child’s hunger cues and feed in response to the infant’s needs, rather than adhering to a predetermined schedule and encouraging bottle emptying. As a general guide, infants aged 0–6 months should take approximately 150–200 mL/kg/day of formula milk. The frequency of feeds varies for each child and at different ages, from every 2–3 hours for newborns, to every 3-4 hours at three months of age, and every 4–5 hours by six months of age. At 6–12 months, when the child’s growth velocity slows and solids are introduced, infants should take about 120 mL/kg/day of formula milk.(10) Overnight feeds should be discouraged if the child is able to sleep through the night.
Caregivers who are anxious about the adequacy of feeds should have their concerns acknowledged and addressed to ensure that the child receives appropriate nutrition without overfeeding. Routine monitoring of growth during well-child visits can help to guide the family doctors in identifying any feeding concerns in the first few years of life.
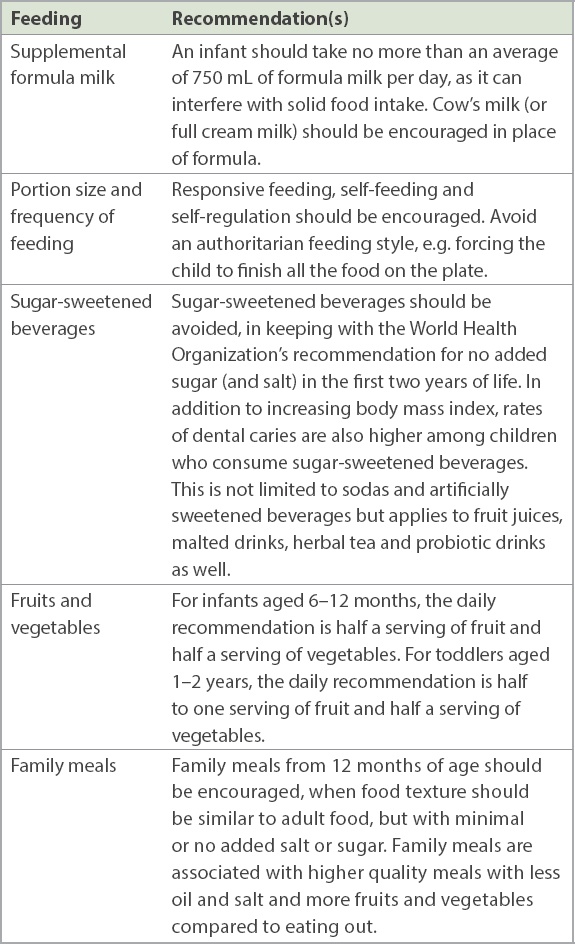
Once a child starts taking more solids from 12 months onwards, there are several common nutritional areas that can be explored to reduce excessive energy intake. These are presented in
Table II
Recommendations to prevent obesity when a child takes more solids from 12 months onwards.
Activities
Reducing sedentary activities has the effects of reducing caloric intake, as well as shifting the focus to other activities that expend more energy.
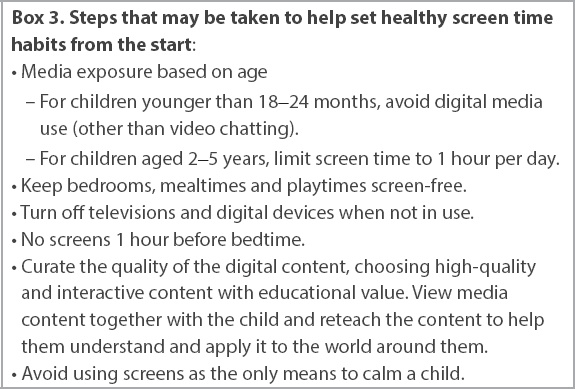
In developed countries, much of the sedentary activity comes in the form of screen time on television and handheld devices. In addition, it has also been found that children who spend more time watching television tend to consume more of the advertised items, such as sweets, sugary beverages and salty snacks.(11) Apart from its effects on obesity, excessive screen time can also affect a child’s cognitive, language and social/emotional development. The family physician should start the conversation about screen time early, beginning with an understanding of the family’s media use habits.
Box 3
Steps that may be taken to help set healthy screen time habits from the start:
Caregivers should avoid having the infant spend too much time in confining equipment such as car seats, swings, strollers and exersaucers. Time should be set aside each day for active, unstructured play. This not only helps with motor skill development, but also contributes to energy expenditure. Children with higher levels of physical activity in early childhood have been found to have better cardiovascular fitness indicators.(13) In addition to developing the musculoskeletal system in areas such as posture, coordination and strength, physical activity also helps with cognitive and social development, mental health and self-esteem.
Family-based approach
A child’s relationship with food starts at home and is moulded by the behaviours and attitudes of caregivers and family members towards their food and mealtimes. For example, it is not uncommon for caregivers to use food as a reward or a means of control over the child. The eating preferences of household members and the types of food in the house also influence the food options that a child is exposed to. Similarly, attitudes towards activities, whether physical or sedentary, begin from the home and immediate community. These environmental factors direct the child’s perception and eventual relationship with food and physical activity, which in turn contribute to the risk or successful management of obesity later in life.
Prevention and management of childhood obesity should, therefore, be family-focused rather than patient-focused. Parental role-modelling plays an important role in promoting physical activity and preventing obesity.(14,15) Strategies should target the caregivers and involve household-wide changes for a higher rate of success and long-term effectiveness. Healthy nutritional and physical activity habits in the home environment help to support and reinforce the desired behaviours in a child and reduce barriers to change. Person-centric forms of counselling, such as motivational interviewing, may be adopted to guide families to make these positive changes.
WHEN SHOULD I REFER TO A SPECIALIST?
Primary care providers play an important role in early identification of overweight children and to provide brief intervention. However, there are instances in which primary care providers should provide follow-up for children with high BMI and refer them to a tertiary centre for further investigation or specialist management. These include: rapid weight gain; increase in weight with slowing height growth; suspected secondary cause for obesity; severe obesity, especially if associated with comorbidities; or failure of primary care management after a six-month trial.
Referral to a dietician with paediatric experience may also be helpful for a more comprehensive nutritional assessment, meal planning and counselling.
USEFUL LINKS
Growth Charts:
Child Growth Standards, WHO:
Measuring a Child’s Growth, WHO:
TAKE HOME MESSAGES
-
BMI-for-age should be tracked and plotted over time for early identification of young children at risk of being overweight or obese.
-
Young children with uptrending or persistently high BMI-for-age (i.e. > 90th percentile) should receive management by the primary care provider to avoid excessive weight gain. This begins with early identification of at-risk children and education of caregivers on the potential implications of childhood obesity for the future health of the child.
-
Primary care providers should provide preliminary assessment and management to address modifiable risk factors in childhood, such as adopting healthy nutrition and physical activity habits, to prevent childhood obesity.
-
Management strategies to prevent obesity during childhood should be family-based, rather than focused on the child, and centred around long-term healthy behavioural and lifestyle changes.
Following an evaluation of Megan’s diet and activity level, you identified that she was taking more than 750 mL of formula milk a day on top of regular meals and snacks. She was also taking a packet of sugar-sweetened beverage with each meal. Her mother was educated on age-appropriate weaning strategies and the importance of preventing childhood obesity. You also discussed strategies to slowly decrease Megan’s formula milk and sugar-sweetened beverage consumption. Cow’s milk was also suggested to replace formula milk. When Megan was reviewed six months later, her body mass index-for-age was in the 75‒90 percentile. She was well, cheerful and developmentally appropriate for her age. You provided anticipatory behaviour and lifestyle advice, and scheduled her next well-child review in 6‒12 months.
SMJ-62-172.pdf
ACKNOWLEDGEMENTS
The authors wish to acknowledge Ethel Lim Jie Kai (Dietician, Department of Nutrition and Dietetics, KK Women and Children’s Hospital, Singapore) for her input, and Dr How Choon How for his invaluable thoughts and feedback in the writing of this paper.


