Abstract
The Singapore Health Services cluster (SingHealth) radiology film archives are a valuable repository of local radiological cases dating back to the 1950s. Some of the cases in the archives are of historical medical interest, i.e. cerebral angiography in the workup of patients with hemiplegia. Other cases are of historical social interest, being conditions seen during earlier stages of Singapore’s development, i.e. bound feet. The archives form a unique portal into the development of local radiology as well as the national development of Singapore. A selection from the archives is published in 2020 in commemoration of the 20th anniversary of the formation of SingHealth, the 55th National Day of Singapore, and the 125th anniversary of the International Day of Radiology. This pictorial essay comprises cardiovascular, respiratory and neurological cases from the archives.
INTRODUCTION
The Singapore Health Services (SingHealth) radiology film archives comprise radiography case records dating back to the 1950s. The archives are located within Singapore General Hospital (SGH) and comprise cases of historical medical interest as well as of historical social interest. The archives form a unique portal into the development of local radiology as well as the national development of Singapore. Additional commentary and anecdotes on these cases were obtained via oral interview with Dr Tan Kim Ping, a prominent local radiologist, former head of department of the SGH Department of Radiology and key proponent of the archives. A selection from the archives was published in 2020 in commemoration of the 20th anniversary of the formation of SingHealth, the 55th National Day of Singapore, and the 125th anniversary of the International Day of Radiology. This pictorial essay comprises cardiovascular, respiratory and neurological cases from the archives.
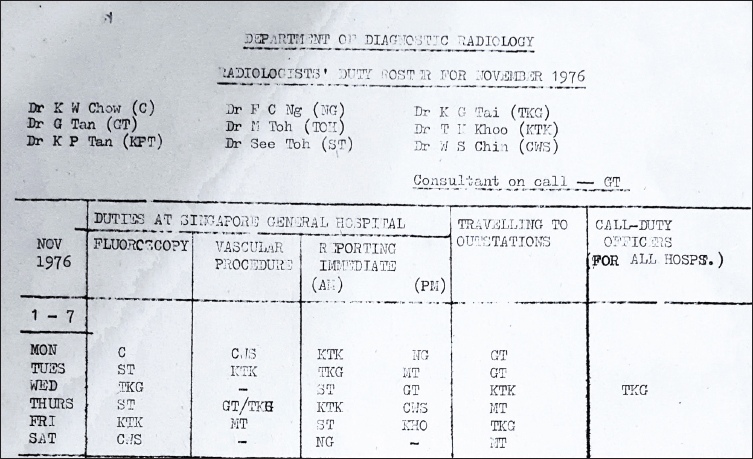
RADIOLOGIST STAFFING IN NOVEMBER 1976
In the 1970s, nine radiologists provided fluoroscopy, interventional radiology and plain radiography reporting services to SGH and three satellite (outstation) hospitals – Thomson Road General Hospital (precursor of the current Changi General Hospital), Alexandra Hospital and Kandang Kerbau Maternity Hospital (renamed KK Women’s and Children’s Hospital in 1997). A single doctor would provide on-call services for these four hospitals. A radiologist roster from November 1976 is shown in
Fig. 1
Radiologist roster in November 1976.
STANFORD TYPE A AORTIC DISSECTION
Fig. 2
Transfemoral catheter aortogram shows the (a) thoracic aorta and (b) abdominal aorta in the setting of a Stanford Type A aortic dissection.
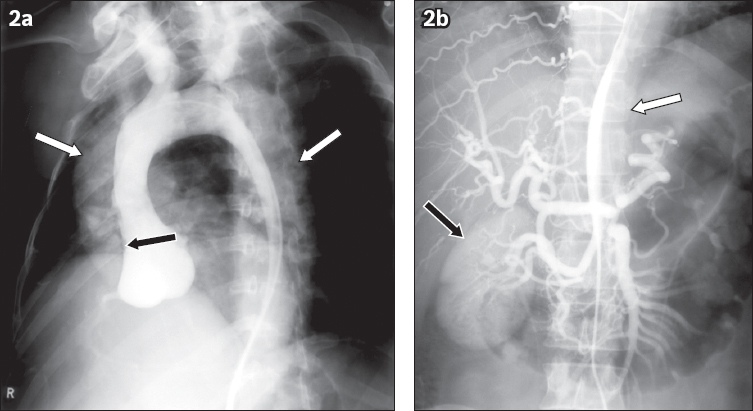
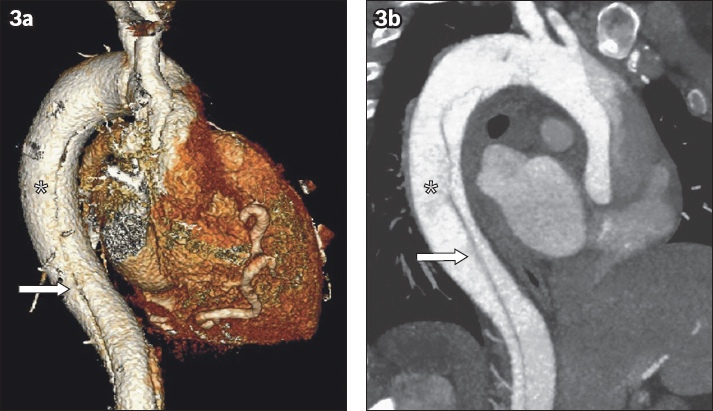
Catheter aortography was previously the gold standard for suspected aortic dissection. One of its pitfalls, however, is a false negative due to thrombosis of the false lumen.(1) CT has since replaced this procedure due to its high image resolution and amenability to post-processing reconstructions, as displayed in a three-dimensional reconstruction and maximum intensity projection sagittal image (
Fig. 3
(a) Three-dimensional reconstruction and (b) maximum intensity projection sagittal CT images show the dissection flap (arrows) and the subtle contrast differences between the true lumen (asterisks) and false lumen in the setting of a Stanford Type A aortic dissection.
LEFT ATRIAL ENLARGEMENT ON BARIUM SWALLOW
A middle-aged woman presented with hoarseness of voice. A barium swallow study performed in the lateral projection (
Fig. 4
Lateral projection radiograph shows posterior displacement of the distal oesophagus (arrows) in the setting of left atrial enlargement.
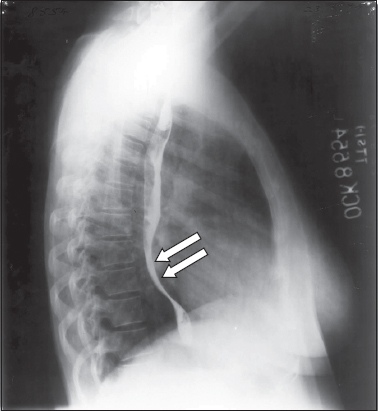
Fig. 5
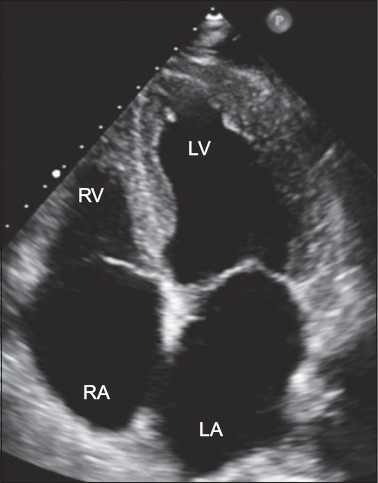
Transthoracic two-dimensional echocardiography was performed on a middle-aged man (different patient from the earlier patient who underwent a barium swallow procedure) with a history of atrial fibrillation. Echocardiogram in four-chamber view shows both cardiac atria enlarged relative to the ventricles. Note that the appearance of apparent communication between the cardiac atria was due to technical factors during image acquisition, and the patient has no atrial septal defect. LA: left atrium; LV: left ventricle; RA: right atrium; RV: right ventricle
EISENMENGER SYNDROME SECONDARY TO ATRIAL SEPTAL DEFECT
Chest radiography was performed in a woman with chronic shortness of breath (
Fig. 6
Chest radiograph of a woman with chronic shortness of breath shows enlargement of the pulmonary trunk and pulmonary arteries with decreased size of the peripheral vessels. Findings are suggestive of the presence of an atrial septal defect with resultant pulmonary arterial hypertension. Film degradation due to ageing is noted.

The upper half of the film (
CONJOINED TWINS
A pair of term dicephalus parapagus conjoined male twins born in the 1980s underwent contrast-enhanced aortography for pre-surgical separation evaluation, which was performed using catheter-guided contrast instillation via the shared umbilical artery. The study outlines a single cardiac silhouette in the right hemithorax with a shared common ventricle (
Fig. 7
A pair of term dicephalus parapagus conjoined male underwent catheter-guided contrast instillation via the shared umbilical artery. Contrast-enhanced aortogram shows a single cardiac silhouette in the right hemithorax with a shared common ventricle. A single united thoracoabdominal aorta in the midline provides arterial supply to each twin via the innominate arteries. Cardiovascular anatomy – A: aorta (shared); H: heart; (R) CCA: right common carotid artery of right twin; (R) IA: right innominate artery (shared); (R) SCA: right subclavian artery in right twin; (L) CCA: left common carotid artery of left twin; (L) IA: left innominate artery (shared); (L) SCA: left subclavian artery in left twin; SVC: superior vena cava, likely shared; UAC: umbilical arterial catheter, tip likely in the left hepatic lobe at the level of L2–3. Other structures – L: liver, shared between both twins, bridging the midline; LS: stomach of the left twin, which shows organoaxial rotation and has herniated through the left hemidiaphragm into the left hemithorax; RS: stomach of right twin; SB: small bowel loops of the left twin, with some loops herniated into the left hemithorax
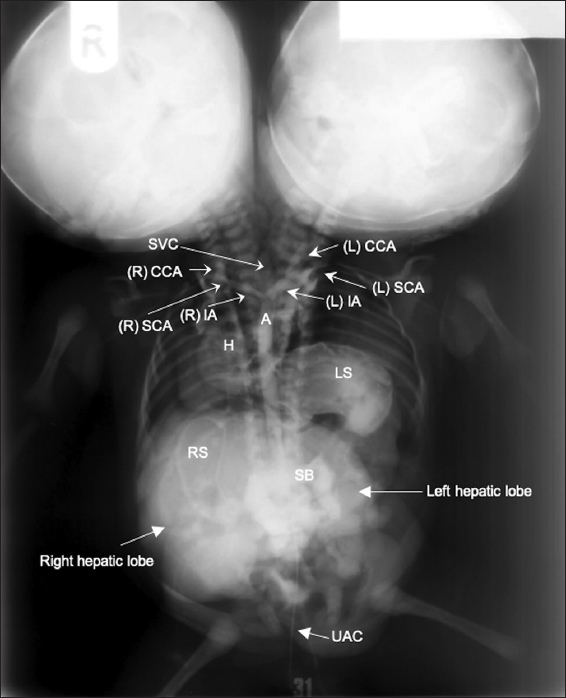
Unfortunately, the depicted case was not amenable to surgical separation given the shared heart. The surgical considerations in the separation of conjoined twins were fraught with ethical considerations and decisions depending on the anatomical configuration encountered, such as considering which twin should receive the pair of lower limbs or the set of sexual organs.
DEEP VEIN THROMBOSIS OF THE LEFT FEMORAL VEIN
Ascending phlebography was described in the 1970s and was previously the gold standard for the diagnosis of deep venous thrombosis (DVT). It involves cannulation of the dorsal foot veins, and assessment of the profunda vein is done with the Valsalva manoeuvre. Pitfalls of interpretation include false positive examination due to under-filling, dilution or admixture of contrast.(4) In
Fig. 8
Ascending phlebogram shows filling defects and distension of the left femoral vein, in keeping with deep venous thrombosis.
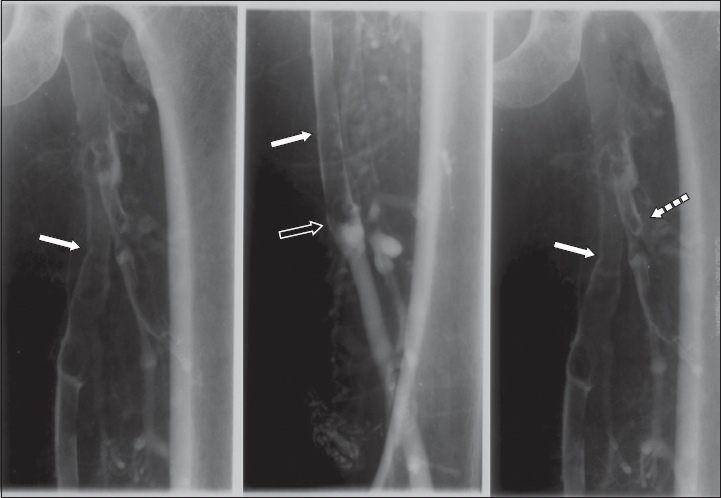
Ultrasonography Doppler assessment has since replaced phlebography for diagnosis of DVT. Nonetheless, this appearance of DVT on venography can still be seen during venous thrombolysis, which is performed to reduce post-thrombotic syndrome.
CHRONIC VENOUS INSUFFICIENCY
Invasive catheter venography was the gold standard test for venous disease before the introduction of duplex ultrasonography in 1989.(5) Plain radiographs of the calf (
Fig. 9
(a) Plain radiograph of the calf shows diffuse periosteal reaction, soft tissue swelling and phleboliths along the tibia and fibula. (b & c) Venograms of the same limb show prominent superficial veins. Overall features are consistent with chronic venous insufficiency.
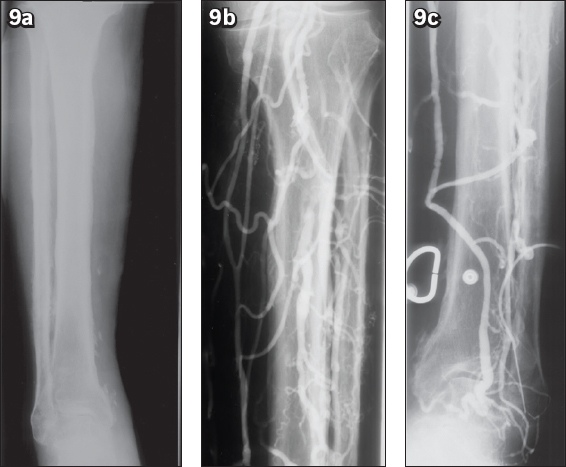
In the context of suspected CVI, ascending venography evaluates perforator competency and deep venous patency. Contrast is injected into a dorsal foot vein under fluoroscopy with the patient in a 30°–45° foot down position and a tourniquet at the ankle. The tourniquet occludes the superficial veins so that contrast is forced into the deep venous system. Any retrograde flow into perforating veins is diagnostic of perforator incompetence.(5) Descending venography via contrast injection into the common femoral vein grades the anatomic extent of the reflux.(6) Catheter venography remains relevant today if venous reconstruction is contemplated.
SILICOSIS
Silicosis was the predominant occupational lung disease in Singapore in the 1970s.(7) This was largely attributed to the presence of granite mines such as those in Bukit Timah, Bukit Batok and Pulau Ubin, where workers were exposed to free silica dust from detonating and processing the granite stones. A chest radiograph (
Fig. 10
Chest radiograph shows imaging features of bilateral hilar adenopathy demonstrating an eggshell calcification pattern (arrows), seen in the setting of silicosis.
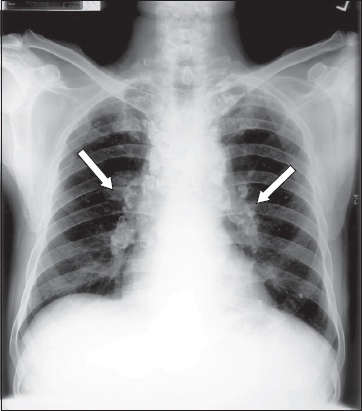
Measures were taken to decrease the prevalence of silicosis. Mines were asked to employ dust control measures. The government necessitated dust exposure monitoring, encouraged use of breathing devices and instituted medical surveillance. In the late 1990s, granite mining licensing was reduced and eventually stopped. Other industries associated with development of silicosis in its workers included the rubber industry, kaolin mines, foundries and brickworks. In the current age, as seen in
Fig. 11
CT image of a patient with complicated pneumoconiosis secondary to silicosis. Note the superior characterisation of mediastinal lymph node calcifications on CT compared to radiography (asterisk).

ASBESTOS LUNG DISEASE
From the 1950s to 1980s, raw asbestos was imported and mixed with cement in a factory to produce roof tiles, ceiling boards and pipes. It was also used as insulating material in shipyard industries and buildings as well as friction material for heavy vehicle components. The chest radiograph of an asymptomatic factory worker (
Fig. 12
Chest radiograph of an asymptomatic factory worker shows curvilinear calcifications along both hemidiaphragms (arrows) representing pleural calcifications. Asbestos lung disease must be considered in the imaging differential.
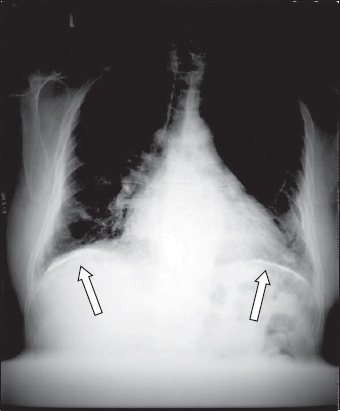
During the 1980s, as the association between asbestos and lung disease became apparent, its use was curtailed. Asbestos was completely banned for use in 2001. Occupational asbestos exposure is, however, still seen today, mainly during demolition or renovation of buildings constructed before 1989.(8) Under the Workplace Safety and Health Regulations 2011, chest radiography is to be performed every 36 months for workers with asbestos exposure.
EMERGENCY MYELOGRAM IN ACUTE PARAPLEGIA
A patient with a history of oesophageal carcinoma presented with acute paraplegia, and emergent myelography was performed. The fluoroscopy-guided myelogram (
Fig. 13
A patient with a history of oesophageal carcinoma presented with acute paraplegia. Emergent fluoroscopy-guided myelogram shows a filling defect within the anterior aspect of the column of contrast within the spinal canal (arrow) secondary to local invasion by the tumour.
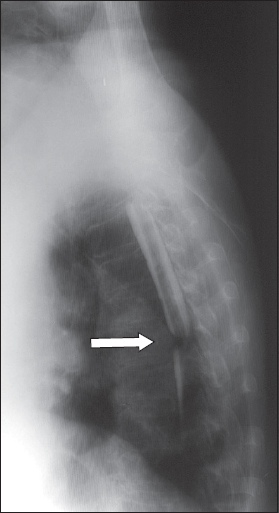
Myelography was first described in 1921. This procedure involved intrathecal instillation of contrast under fluoroscopic guidance by a radiologist, followed by the acquisition of fluoroscopic and, in later years, CT images of the spinal canal. The first contrast medium used was oil-based Myodil, which was used for years and later found to cause arachnoiditis. It was replaced when non-ionic water soluble contrast media became available in the 1980s.
For decades, myelography was the only diagnostic method available to investigate pathology within the spinal canal until the advent of MR imaging in the late 1980s. At present, myelography is still performed in patients for whom MR imaging is not possible for safety reasons(9) (e.g. non-MR-compatible pacemakers), and in patients with metal spinal implants that would result in severe degradation of MR image quality due to artefacts.
SUBDURAL HAEMATOMA
Catheter cerebral angiography of the right internal carotid artery was performed in a patient with left hemiplegia (
Fig. 14
Catheter cerebral angiogram of the right internal carotid artery shows leftward deviation of the branches of the anterior and middle cerebral arteries across the midline of the skull with a clear crescentic avascular space under the skull (arrowheads). These findings are worrisome for the presence of a subdural haematoma; this diagnosis was subsequently confirmed on right craniectomy.
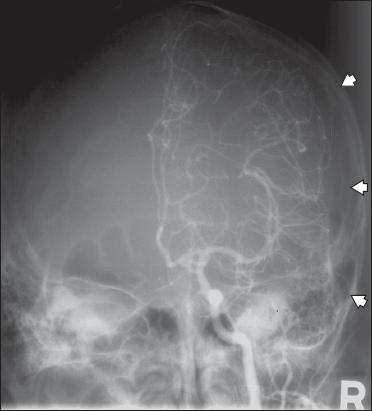
Prior to the advent of routine head CT imaging, emergent catheter cerebral angiography was the default radiological investigation for patients with neurological symptoms.(10) This study was performed at TTSH, which was the first hospital designated in Singapore for specialised neurosurgical procedures. The investigation, performed via femoral catheter or direct arterial puncture, was used to differentiate the pathological processes of intracranial mass (tumour blush pattern or deviation of vascular structures), infarct (absence of blood flow) and intracranial haemorrhage (vascular blush pattern in intraparenchymal haemorrhage, or the presence of an irregularly contoured intracranial aneurysm with or without mass effect in ruptured aneurysmal subarachnoid haemorrhage). Hydrocephalus may also be suspected and confirmed by air encephalography or ventriculography.
MENINGIOMA WITH PROMINENT MENINGOHYPOPHYSEAL ARTERY
Urgent catheter cerebral angiography of the left internal carotid artery was performed for a patient who presented with right hemiparesis (
Fig. 15
Angiogram of the left internal carotid artery shows an abnormally prominent meningohypophyseal artery arising from the cavernous segment of the left internal carotid artery and leading to a region of abnormal-seeming blood vessels, which show a characteristic ‘tumour blush’ (arrow) angiographic pattern. Surgery was performed, which demonstrated tentorium cerebelli meningioma.

ACKNOWLEDGEMENTS
The authors would like to acknowledge the staff of the Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital, Singapore, for their assistance in digitising the hard copy films from the SingHealth Radiology Archives; Dr Kamalesh Anbalakan (Cardiology) for the two-dimensional echocardiography image on the case ‘left atrial enlargement’; and Dr David Alexander Stringer (Paediatric Radiology) for his input on the case ‘conjoined twins’.
SMJ-61-640.pdf


