Abstract
INTRODUCTION
As the traditional overnight call system was shown to contribute to fatigue, Singapore implemented a shift system in 2014. We aimed to compare activity levels, sleep (using a wrist actigraph), fatigue and professional quality of life between residents working on night float and those on overnight calls.
METHODS
All Postgraduate Year 1 (PGY1) residents at our institution were invited to participate. Participants were required to wear a wrist actigraph for four months and complete two validated surveys (Epworth Sleepiness Scale [ESS] and Professional Quality of Life [ProQOL] scale) once each at the start and end of the study.
RESULTS
49 residents were recruited. Night float and on-call residents showed a comparable median (range) number of steps (10,061 [1,195–15,923] vs. 10,649 [308–21,910]; p = 0.429), amount of sleep logged (361 [149–630] minutes vs. 380 [175–484] minutes; p = 0.369) and time taken to fall asleep (6 [0–14] minutes vs. 6 [range 0–45] minutes; p = 0.726), respectively. Night float residents had less efficient sleep, with 90.5% having sleep efficiency of over 85% compared to 100% of on-call residents (p = 0.127). More night float residents reported ESS scores > 10 (73.1% vs. 38.5%) and higher burnout scores on ProQOL scale (41.4% vs. 21.4%) at the start of the study. However, this was similar to the end of the study and not statistically significant.
CONCLUSION
Physical activity and amount of sleep were not significantly different between night float and on-call residents. Residents on night float reported comparatively more fatigue and burnout.
INTRODUCTION
Since May 2014, all house officers in Singapore have come under a national framework for training and reassessment termed as Postgraduate Year 1 (PGY1) training, in which work should not exceed 80 hours per week, including night hours.(1) As the traditional overnight on-call system has been shown to contribute to fatigue, affecting mood and daytime sleepiness, there was a move to implement a shift system that would reduce the continuous stretch of overnight call work in clinical departments. Fatigue and burnout are known to have detrimental effects on residents, which may have long-lasting implications for their physical and mental well-being.(2,3) Studies have reported increased somatic complaints, depression and increased physical danger in residents who are more fatigued.(4) Hence, the aim of the night float system was to reduce fatigue in residents in order to minimise these detrimental effects.
Residents at our institution, National University Hospital (NUH), Singapore, are either on the night float system or the traditional overnight on-call system, depending on manpower allocation and department requirements. In the night float system, residents work for five consecutive nights a week once every two months, compared to the traditional on-call system where each resident is on call for 4–6 nights per month. Residents assigned to night float do not have daytime assignments; they perform on-site duty during evening/night shifts and are responsible for admitting or cross-covering patients until morning.(5) In our institution, this is defined as working from 8 pm to 8 am the next day. As our institution had two groups of PGY1 residents doing night duty on two unique systems, this allowed us to study whether there were any difference in terms of sleep, activity and fatigue levels in our PGY1 cohort. We hypothesised that the overnight on-call rota would be associated with less sleep and result in increased fatigue and burnout, and that the converse would be true for residents on the night float system.
METHODS
The study was approved by the National University of Singapore institutional review board. It comprised two components: (a) wearing a wrist actigraph for a continuous period of four months; and (b) completing two questionnaire surveys, namely the Professional Quality of Life (ProQOL) scale (
The ProQOL scale – initially created for therapists, nurses and humanitarian workers – is a widely used tool to assess positive and negative aspects of caring. It comprises the positive (compassion satisfaction) and negative (compassion fatigue or secondary traumatic stress) aspects of helping others who have experienced suffering. Compassion satisfaction is defined as the pleasure derived from being able to do one’s work well. Higher scores on this subscale represent greater satisfaction with one’s ability to be an effective caregiver. The compassion fatigue or secondary traumatic stress subscale measures work-related secondary exposure to extremely stressful events; higher scores represent greater compassion fatigue. The three aspects of the ProQOL scale were scored based on cut-off scores, as per the validated scoring, and analysed as categorical data. Compassion satisfaction scores ≤ 43 were defined as low (fewer positive aspects of working as a helper), while burnout scores ≥ 57 (inefficiency and feeling overwhelmed) and traumatic stress scores ≥ 57 were defined as high.
The ESS is a self-administered questionnaire with eight questions. It provides a measure of a person’s general level of daytime sleepiness, or their average sleep propensity in daily life. Scores > 10 generally depict increased fatigue. This simple questionnaire has been validated and shown reliability as a measure of daytime sleepiness.
All PGY1 residents in the institution were invited to participate. Participants were asked if they had any known medical conditions. Exclusion criteria were psychiatric disorders, sleep disorders and cardiac problems. Information about the study was presented to PGY1 residents across all departments during their weekly continuing medical education sessions over four weeks prior to the launch of the study. Recruitment posters were also placed in the residents’ lounge and lift lobbies around the hospital. Although the residents were working in different departments, their job scope was largely similar. Residents were responsible for interviewing and examining newly admitted patients, creating admission histories, writing admission orders, performing phlebotomy services, following up on laboratory results, reporting interim updates to their supervising resident and doing discharge summaries. Participants provided voluntary written informed consent. They were allowed to keep the wrist actigraph after the completion of the study.
Study participants were instructed to wear the wrist actigraph on their non-dominant hand every day for four months throughout the study period. Data from the wrist actigraph was downloaded weekly or fortnightly into an actigraphy-based scoring software program (Detalytics Pte Ltd, Singapore) that enables calculation of sleep duration, sleep latency (time taken to fall asleep) and sleep efficiency (non-restless sleep ≥ 85%). Resident call schedules were used to label sleep and activity logs that corresponded to overnight call or night float periods. In addition, residents were routinely required to log their duty hours using the New Innovations online software (
Data was analysed using IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp, Armonk, NY, USA). Mann-Whitney U test was used for continuous variables (e.g. number of steps and minutes of vigorous/moderate activity) with non-normal distribution. Chi-square test was used for categorical variables (e.g. ESS and ProQOL scale scores, which were categorically split based on the defined cut-offs).
RESULTS
Of the 87 PGY1 residents, 49 (56.3%) consented to participate in the study. Recruited residents were either from or were rotating through the departments of inpatient general medicine, paediatrics, orthopaedics, obstetrics and gynaecology, and general surgery. The actual study took place over a four-month period from 1 January 2015 to 30 April 2015. As the intake for PGY1 residents is between May and September each year, all residents in the study would have worked for at least four months prior to the study’s start date.
The median age of residents was 25 (range 25–27) years and 42.8% of participants were men. 5 (10.2%) residents reported having medical problems including allergic rhinitis, asthma, eczema, glaucoma or Graves’ disease (
Table I
Characteristics of study population (n = 49).
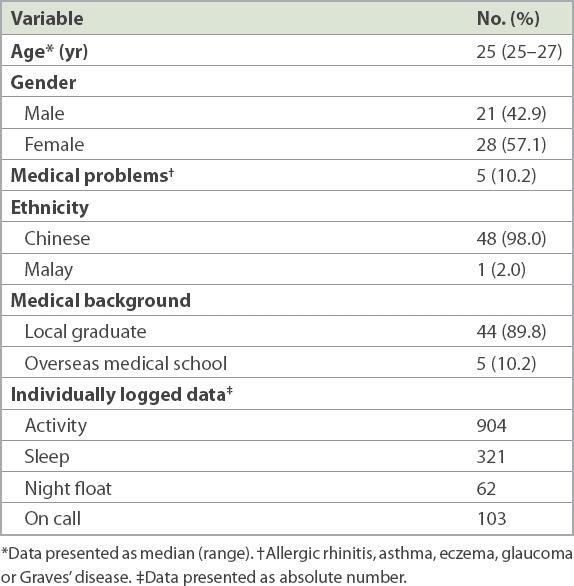
Throughout the study period, the PGY1 residents had 904 individually logged records for activity and 321 individually logged records for sleep. Residents on night float had 62 individually logged records and on-call residents had 103. Of the 49 PGY1 residents who participated, only 11 (22.4%) residents completed all four months of the study using the wrist actigraph; 24 (49.0%) residents logged at least one month of data and 14 (28.6%) residents recorded less than one month of data. At the start of the study, 43 (87.8%) residents completed both surveys, while at the end of the study, 28 (57.1%) residents and 27 (55.1%) residents completed the ESS questionnaire and ProQOL survey, respectively. Residents with less than one month of data were omitted from analysis.
The recorded logs were analysed based on whether they corresponded to activity or sleep during night float or on-call rota. Average number of steps and activity duration per day were similar for both groups of residents. The median number of daily steps for residents on night float (10,061 [range 1,195–15,923]) was similar to that of on-call residents (10,649 [range 308–21,910]; p = 0.429). The median duration of vigorous activity per day was 22.5 (range 0–67) minutes and 24 (range 0–110) minutes for residents on night float and on-call rota, respectively (p = 0.582). The median duration of moderate activity per day was 110.5 (range 2–183) minutes and 108.0 (range 0–197) minutes for residents on the night float and on-call rota, respectively (p = 0.506) (
Table II
Quantitative comparisons of activity levels and sleep, measured with wrist actigraphs, between the two groups.
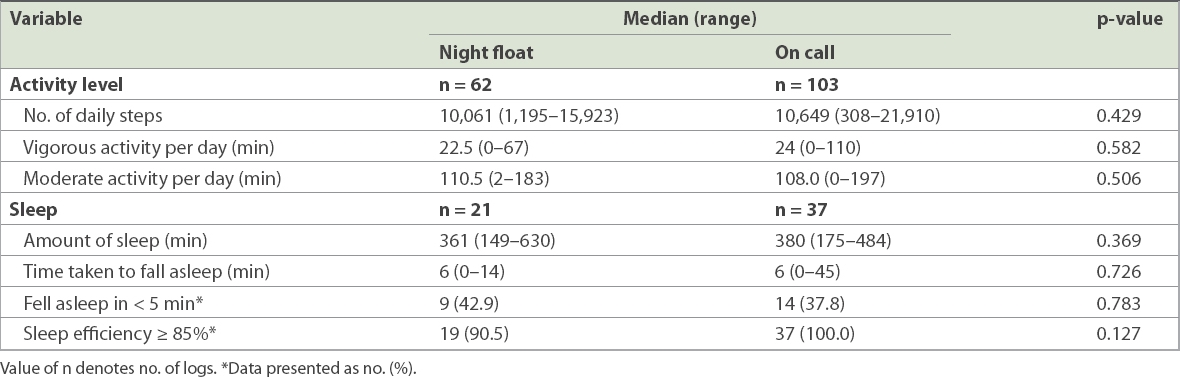
With regard to sleep, residents on night float appeared to have less efficient sleep when compared to those on the on-call rota despite spending similar amounts of time asleep. The proportion of residents on night float with sleep efficiency of at least 85% was 90.5%, as compared to all residents on overnight calls for whom data was available, although the difference was not statistically significant (p = 0.127). The median amount of sleep for night float residents (361 [range 149–630] minutes) was comparable to that among on-call residents (380 [range 175–484] minutes; p = 0.369). Both groups of residents took a median time of six minutes to fall asleep (night float: 6 [range 0–14] minutes, on call: 6 [range 0–45] minutes; p = 0.726). Many residents in both groups took less than five minutes to fall asleep (night float: 42.9%, on call: 37.8%; p = 0.783).
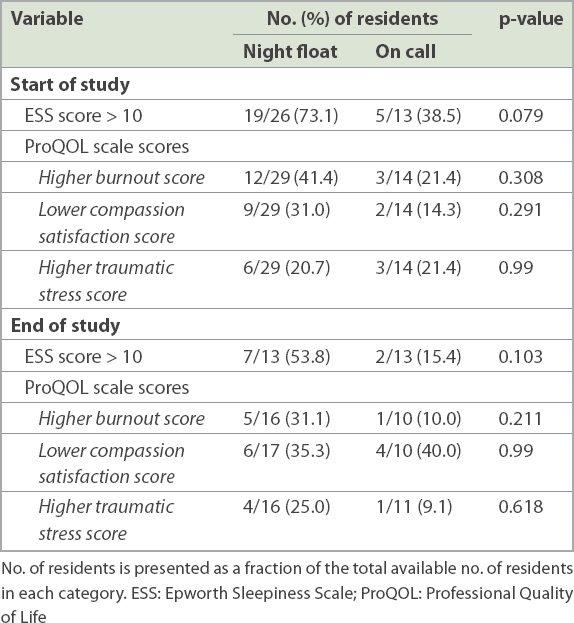
At the beginning of the study, 73.1% of residents on night float reported an ESS score > 10, as compared to 38.5% of on-call residents (p = 0.079). This was similar to findings at the end of the study, where 53.8% of residents on night float reported an ESS score > 10 versus 15.4% of those doing calls (p = 0.103). A larger percentage of residents on night float also had a higher burnout score on the ProQOL scale (night float: 41.4%, on call: 21.4%) at the start of the study, although the difference was not statistically significant (p = 0.308) (
Table III
Comparison of the ESS and ProQOL scale scores of the two groups.
DISCUSSION
Our study demonstrated that physical activity and amount of sleep were not significantly different between residents on night float and those on call. These results are surprising, as the implementation of the night float system did not appear to reduce physical activity or increase the amount of sleep even though these were important contributing factors to the development of fatigue. Furthermore, residents on night float reported higher fatigue and burnout, although these were not statistically significant.
To the best of our knowledge, this is the first study that uses quantitative means to measure amount of sleep and activity levels together with the degree of fatigue and burnout, among PGY1 residents in Singapore. As our hospital has residents rotating through both the night float and traditional on-call systems, we were able to compare the sleep and activity levels of the same group of residents who were rostered to do night duties either on night float or on call over the four-month study period.
Our study showed similar amounts of activity and sleep patterns in these residents regardless of whether they were doing shift work or overnight calls. This suggests that shortening the interval of work hours by promoting shift work has not increased sleep in residents. Results of the ESS survey also do not suggest that residents on the shift system were less fatigued than those doing overnight calls. Similarly, a recent study by Richardson et al reflected that trainees with protected time failed to use the time to sleep and slept the same amount as when they were doing calls.(8) This suggests that implementing a shift system to combat fatigue levels alone is not sufficient to counteract the effects of sleep deprivation on physician performance.
In terms of sleep, residents in our hospital averaged approximately six hours of sleep every night. While some experts claim that at least six hours of sleep is required for optimal day-to-day functioning,(9) it is worth noting that the average amount of sleep obtained by residents is the bare minimum needed. Recent reviews have also reported that the average underlying sleep tendency among young adults is about 8.5 hours per night.(10,11) Both groups had residents who fell asleep in less than five minutes, which corresponds to severe sleepiness. This finding implies that residents might have chronic sleep deprivation and is in accordance with our survey data, where up to half of residents reported increased fatigue and high burnout rates. This is a worrying trend, as multiple studies have shown that chronically sleep-deprived residents have decreased vigilance and work productivity, with deleterious side effects for health.(12,13)
Our study suggested that working shorter hours on night float did not change the amount of physical activity of our residents (measured in terms of activity levels and amount of vigorous activity) or the amount of sleep the residents had. Both groups of residents demonstrated similar activity levels and vigorous activity throughout the day. As we did not specifically ask residents to log their activities outside of work or specify exactly how many hours they were at work, we were unable to determine if the physical activity, in terms of steps taken, was predominantly during night float (i.e. at work) or in the daytime (i.e. when they were not working and could rest).
Our study was not without limitations. There was a high dropout rate, with only one-third of residents wearing the wrist actigraph for the entire duration of the study, and only half of the cohort completing the surveys at the end of the study. We postulated that residents who completed these surveys were the ones who were less fatigued, as they had more bandwidth and were therefore able to comply with the study protocol. This could imply that our data underrepresented the true amount of fatigue and burnout felt by PGY1 residents. Conversely, we also could not rule out the possibility that residents who were more fatigued felt more compelled to complete the surveys at the end of the study. We acknowledge that the use of surveys for data collection may be open to recall bias.
We note that it would have been interesting to compare the activity levels of residents during and after working hours. However, we did not have all the appropriate data necessary to correlate the activity levels of residents with the periods that they were at work or doing call duties, as a number of residents did not log their duty hours for certain time periods. Additional studies can be done to directly compare this. Furthermore, the sleep data collected was a summation of the entire amount of sleep throughout the 24-hour day, without distinguishing it from daytime naps or sleep during rest periods while still at work.
In summary, our study suggests that adoption of a night shift system alone is insufficient for reducing fatigue and burnout levels among PGY1 residents. Further studies can be done to identify other factors outside of work that might contribute to fatigue. These may include the effect of off-duty activities on residents’ sense of fatigue, burnout and overall quality of life.
ACKNOWLEDGEMENTS
Funding for the Fitbit devices was provided by the National University Health System Clinical Quality and Innovation Fund, Singapore. We thank Dr Janelle Maria Liwanag, NUH, and Ms Wang Sha, Detalytics Pte Ltd, Singapore, for their assistance with data collection, and Ms Rajgor Dimple, NUH, for her assistance in the editing and submission of the manuscript.


