Abstract
INTRODUCTION
Increasing financial challenges have resulted in great debt among medical graduates worldwide. In Singapore, more scholarships and bursaries have been disbursed in recent years to support students who are financially challenged. We aimed to study the financial status of medical students in National University of Singapore (NUS) Yong Loo Lin School of Medicine (i.e. NUS Medicine), Singapore, and the financial support available to them.
METHODS
A cross-sectional quantitative study was performed. Surveys were distributed and completed by medical students of NUS Medicine. Information regarding household income, financial assistance, monthly allowance and expense, and concurrent occupations was collected. We compared our findings with the results of a similar study performed in 2007 and national income data.
RESULTS
A total of 956 (66.2%) out of 1,445 medical students completed the survey. 19.5% and 58.5% of respondents came from households with monthly incomes < SGD 3,000 and > SGD 7,000, respectively. 20.6% of students had loans, 18.9% had scholarships and bursaries, and 14.4% worked to support themselves.
CONCLUSION
Medical school fees have risen by more than 50% over the past ten years. Our study found that there were increases in the proportion of students from both the lower- and higher-income segments, with proportionally fewer students from the middle-income segment. A large number of students were working and/or had some form of financial support. More should be done to meet the needs of financially challenged medical students to ensure equal access to quality medical education.
INTRODUCTION
Determining the true cost of a university medical education is complex.(1) From the medical student’s perspective, the cost includes medical school tuition fees, textbook and instrument costs, as well as transportation and other costs of daily living. Globally, medical school tuition fees vary greatly. In some European countries, medical students pay minimal or no tuition fees.(2) However, in most parts of the world, tuition fees for a medical education are much higher compared to those of other undergraduate and graduate programmes. In the United States (US), the annual tuition fees in private medical schools often exceed USD 40,000 per student.(3) High tuition fees may have deterred certain disadvantaged groups from entering medical school despite their potential to contribute to society and academia.(4) High fees are also reported in some settings, affecting career choices and postgraduate community involvement,(4-7) and causing most medical students to depend on external sources to finance their medical education.(8) With rising tuition fees and general costs of living, the rate of increase of debts incurred by medical students has far exceeded the inflation rate in many countries.(9) In the US, for instance, 87% of students who graduated from medical school in 2008 carried some form of debt.(10)
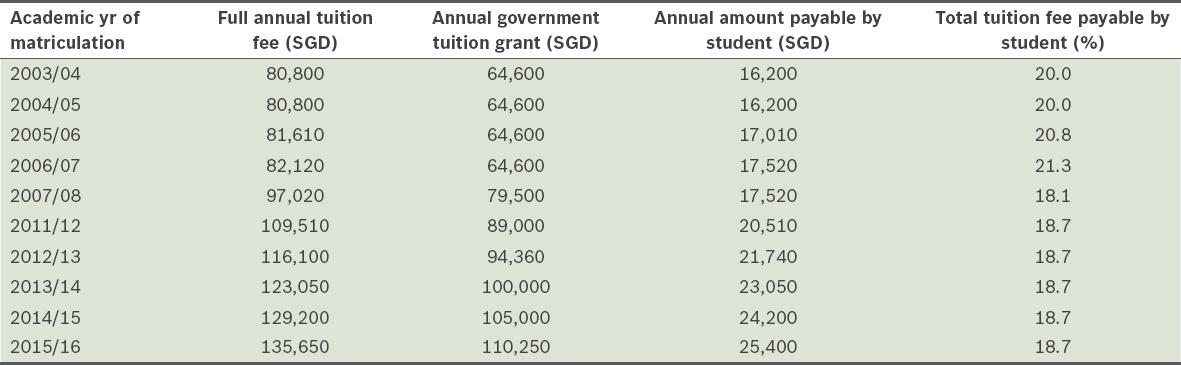
In Singapore, medical school tuition fees have been increasing rapidly in the last decade. The teaching grant provided by the Singapore government under the Medical/Dental Undergraduate Agreement(11) has greatly reduced tuition fees for Singaporean medical students. However, the amount paid by students still continues to rise. Details of tuition fees for National University of Singapore (NUS) Yong Loo Lin School of Medicine (i.e. NUS Medicine), from academic year (AY) 2003/04 to 2015/16 are shown in
Table I
Trend of tuition fees per annum for an MBBS degree in National University of Singapore Yong Loo Lin School of Medicine (Singapore citizens).
In 2009, Ng et al published the results of a financial study conducted on medical students from NUS Medicine.(12) It revealed that a large number of medical students experienced severe financial difficulties coping with the tuition fees, despite the existence of numerous financial aid schemes. This study was instrumental in raising awareness about the needs of financially disadvantaged medical students and helping to establish a number of new scholarships and bursaries to assist these students. Thus far, the financial aid schemes that have been established are offered to students based on certain criteria. Some forms of aid disbursed are purely based on household income levels, while others are merit-based with consideration of both the academic standing of the individual and his/her household income level.
In the current study, we aimed to examine whether the rise in medical school fees over the years has increased the proportion of NUS Medicine students with a significant financial burden. We also described the current distribution of financial aid available for NUS Medicine students. We hope that the study findings will provide decision-makers with useful information, allowing them to better support medical students financially.
METHODS
A quantitative survey was conducted on all medical students from NUS Medicine. The authors obtained ethical approval for this study from the NUS Institutional Review Board (IRB; NUS IRB code: IRB-2014-07-015), with permission for a waiver of consent to preserve the anonymity of the participants, due to the sensitive nature of the questionnaire. Completion of the survey was considered to be consent for involvement in the study. Hard copies of the questionnaire forms were distributed to all Year 1–5 NUS Medicine students in 2014. No faculty members were involved in the distribution of questionnaires, and an attempt was made to ensure that there was no incentive for participation or disincentive for non-participation. No identifiers were collected within the survey. Participant information sheets were provided along with the questionnaires to all potential participants. A briefing was also provided before the start of the survey.
Information regarding household income, financial assistance, monthly allowance and expense, and concurrent occupations was collected. All data collected was analysed using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA). Chi-square test was used to determine statistical significance in differences between groups. Where relevant, we included error margins in the form of confidence intervals. Data from this study was compared with that from a previous study conducted among NUS Medicine students in AY 2007/2008.(12) Where relevant, the key household income trends in the years 2006(13) and 2014(14) were compared. These national trends are based on studies published by the Singapore Department of Statistics in the years 2006 and 2014.
RESULTS
A total of 956 out of 1,445 medical students responded to the survey in AY 2014/2015, translating to a response rate of 66.2%, compared to 735 out of 1,143 (64.3%) medical students in the AY 2007/2008 survey.(12)
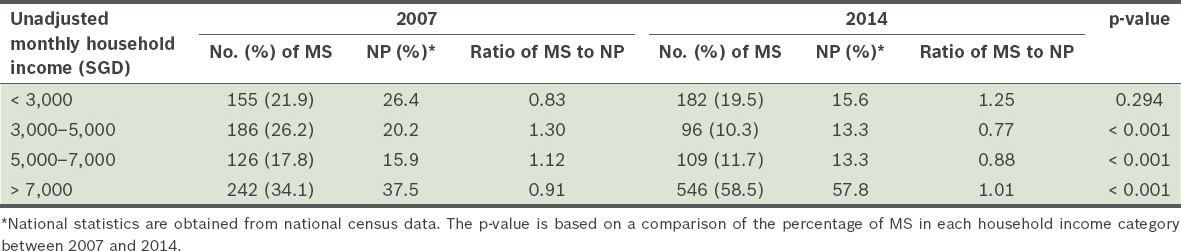
The proportion of medical students from households with a monthly household income from work (unadjusted for inflation) of at least SGD 7,000 (i.e. higher-income) was much higher in 2014 than 2007 (58.5% vs. 34.1%; p < 0.001). However, the proportion of such medical students was similar to that of the national population (57.8%), based on 2014 national census data. Further details are shown in
Table II
Comparison of monthly household incomes, from work, of medical students (MS) and the national population (NP) in 2007 and 2014.
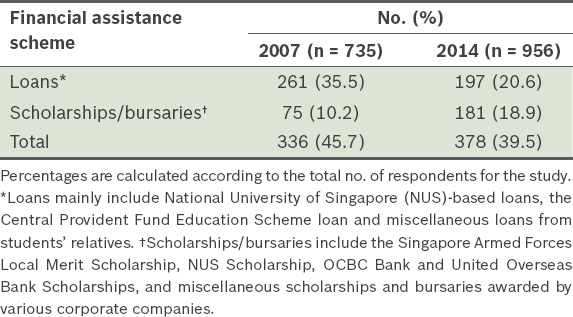
The total number of students on financial assistance schemes decreased from 45.7% in 2007 to 39.5% in 2014 (
Table III
Proportion of medical students under the various financial assistance schemes in 2007 and 2014.
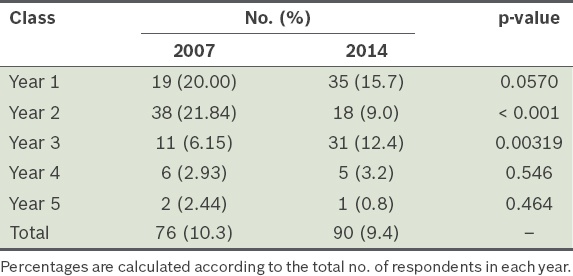
The proportion of medical students who resided in on-campus accommodation was similar, at 10.3% in 2007 and 9.4% in 2014 (
Table IV
Comparison of proportion of medical students who lived in on-campus accommodation in 2007 and 2014.
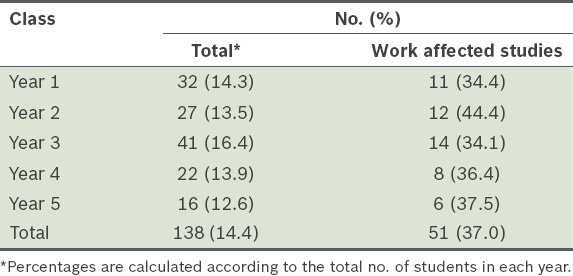
About 14.4% (n = 138) of medical students engaged in work over and above their medical studies (
Table V
Proportion of medical students who worked and stated that their work negatively impacted their studies in 2014.
DISCUSSION
Medical school tuition fees in Singapore have risen by almost 50% over the last seven years, since the last comprehensive analysis of the financial status of medical students conducted in 2007.(12) We studied the financial status and impact of these rising fees among NUS Medicine students in 2014 and compared our findings with those of the earlier cohort. While household incomes had increased among medical students in tandem with the national figures, the most striking finding was the rise in the proportion of students who came from lower-income households. This was accompanied by a decrease in the proportion of students from the middle-income groups and an increase in the proportion of students on financial aid and loans. A large number of students were also engaged in some form of work in the course of their medical education. Many of these students opined that their work had negatively affected their education.
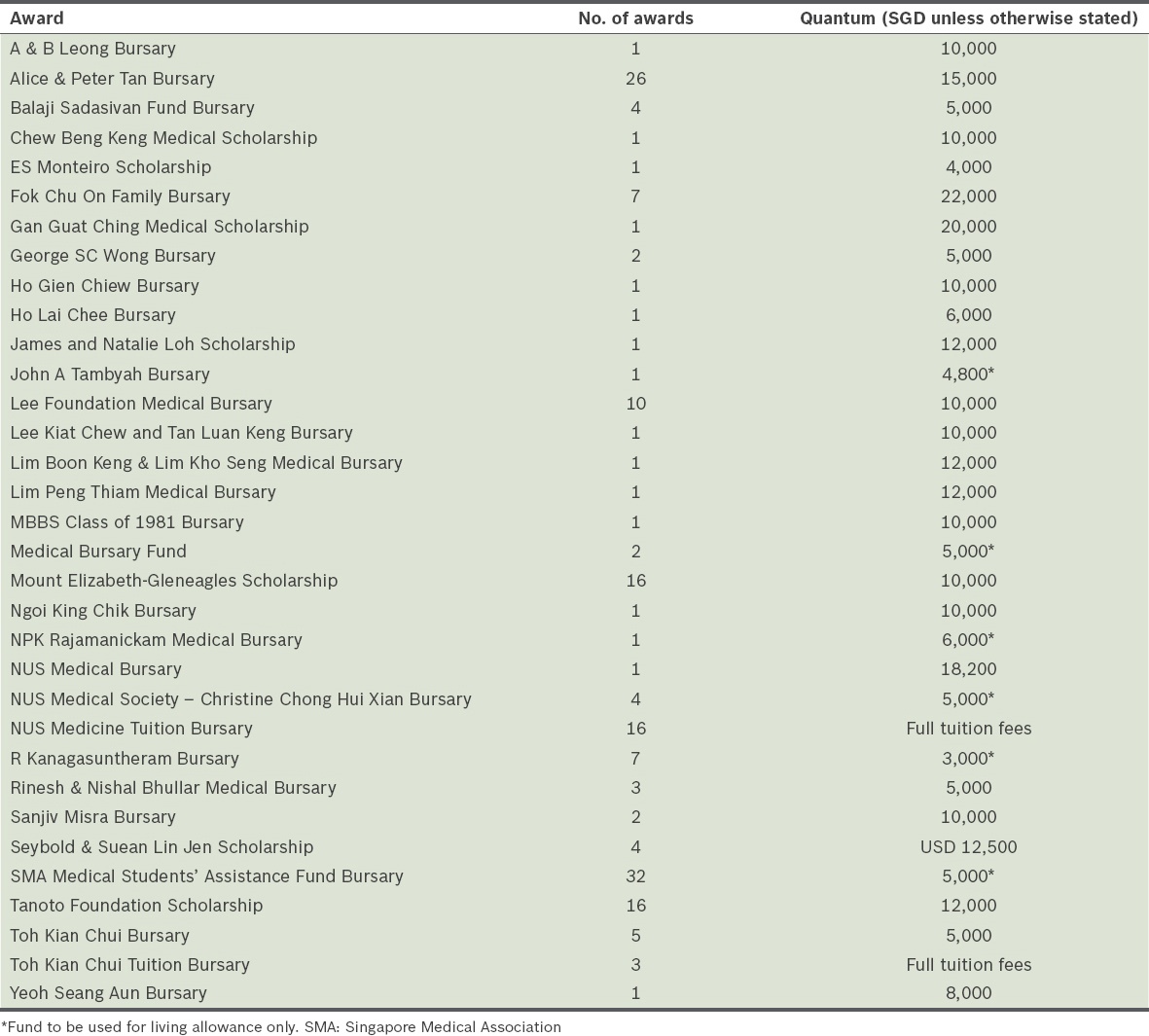
The shifts in the proportion of medical students from the groups with the highest and lowest income between 2007 and 2014 are generally consistent with the changes in the national household income distribution in Singapore. However, interestingly, there was a higher proportion of medical students from the lower-income group (19.5%) compared to the national proportion of households from this group (15.6%) in 2014. This is different from in 2007, during which the proportion of medical students from lower-income households (21.9%) was lower than the national proportion of lower-income households (26.4%). There are some possible reasons for this: a rising number of non-citizen families residing in Singapore that may have a lower household income from work, reflected in lower incomes in Singapore dollars; and greater outreach by NUS Medicine to increase the diversity of applicants to the medical school. The current financial bursaries offered to medical students at NUS Medicine are shown in
Table VI
Bursaries and scholarships available to National University of Singapore (NUS) Yong Loo Lin School of Medicine students.
In the current study, we found a statistically significant shift in the proportion of medical students from the higher-income group, from 34.1% in 2007 to 58.5% in 2014. However, as there was a concomitant rise in the national proportion of households in the higher-income group, from 37.5% to 57.8%, the ratio of medical students compared to the national population in this group remained similar (0.91 in 2007 vs. 1.01 in 2014). This suggests that despite the increased proportion of medical students from the higher-income group and decreased proportion from the middle-income groups, increasing medical school fees over the years may not have deterred the middle-income from applying for medical school. Instead, our finding may have been another manifestation of economic differences within the strata of Singapore’s society.
From 2007 to 2014, we noted a decrease in the number of medical students who received some form of financial assistance, from 45.7% to 39.5% of students. This was despite an increase in the number of medical students who received bursaries and scholarships, from 10.2% in 2007 to 18.9% in 2014. The rise in the number of students depending on scholarships and bursaries could be partly due to the relatively higher proportion of students from lower-income households and the sharp rise in the overall total cost of medical education over the years (
We also found that 14.4% of NUS Medicine students were involved in some form of work during their medical school years. More than one in three of these students stated that their work had negatively affected their studies. This suggests that a high proportion of medical students who work do so out of necessity, to support themselves financially and reduce the financial burden on their families. The impact of work on a student’s medical education, in addition to existing heavy financial burdens, further contributes to the potential mental health issues the student may face. All this may lead to a suboptimal medical education. Studies from the United Kingdom, where medical school tuition fees rose from just over GBP 3,000 per year in 2011 to GBP 6,000–9,000 in 2012, have shown that poor mental health in medical students was related to financial challenges, with some considering leaving school due to financial challenges,(18-20) financial concerns,(21) being in debt(22) and being concerned about debt.(23) Other studies have also shown that financial challenges result in poorer mental health in tertiary students.(24-27)
To overcome the issue of rising tuition fees, several solutions have been proposed in the literature. Weinstein et al,(28) for instance, discussed the SAFE (Strategic Alternative for Funding Education) programme, in which practising physicians pay for their medical school education over a ten-year period after completing relevant postgraduate training, rather than through loans obtained while studying. Other suggestions from overseas include shortening the length of medical school training,(29) raising the salary of residents so as to increase the ease of debt payment, and decreasing the length of residency and fellowship training.(30) With the ever-increasing medical school tuition fees, practical solutions have to be considered to reduce the financial burden of a medical education and to ensure increasing diversity in the medical students whom we attract. In Singapore, students start repaying their student loan once they start working, which potentially has an adverse impact on postgraduate career choices.(5,7) When this medical school was first established in Singapore in 1905,(31) it was recognised that medical education had to be accessible to the best students with aptitude and interest in medicine as a career, in order to serve the local community. Hence, a number of scholarships were made available and fees were kept low.(1,31) Hopefully, some of that spirit can continue as NUS Medicine moves forward into its second century.
This study had certain limitations. First, as it is primarily a survey of medical students, our data heavily depended on self-reported information and was therefore prone to recall bias. Second, despite our best efforts to reach out to all the medical students in NUS Medicine, there was still a 33.8% non-responder rate for the current survey. The participation of this group of non-responders could have resulted in some differences and impacted our findings.
In conclusion, undergraduate medical school tuition fees in Singapore have been rising over the years. It is reassuring that the proportion of students from the lowest household income group has increased, possibly in response to efforts by NUS Medicine to increase the diversity of applicants to the school. However, the drop in proportion of students from lower- and middle-income households and the large number of students who have to work despite its impact on their studies are both serious concerns. We need to establish more comprehensive funding models to ensure that Singaporeans are served by the most qualified doctors in the future, regardless of the socioeconomic background of the doctors in their formative years.
ACKNOWLEDGEMENTS
The authors would like to thank the Singapore Medical Association (SMA) and NUS Medicine for their unwavering support for this study. We especially thank Prof Hooi Shing Chuan, Vice Dean of NUS Medicine; Mr Martin Ho, Chief Administrator of SMA; as well as Mr Ivan JR Low, Mr Koh Hwei Keong, Ms Yap Pek Be and Ms Salbiah Binte Amin of NUS Medicine for their guidance and administrative support throughout the study.


